Malnutrition persists at unacceptably high levels on a global scale.1,2 Worldwide, 20.5 million newborns (14.6% of all live births) have a low weight at birth. Among children under five years of age, 149.2 million are stunted, 45.4 million are wasted (6.7%), and 38.9 million (5.7%) are overweight (5.7%).1,2 Mozambique still experiences a chronic malnutrition burden among its under-five population, accounting for a national prevalence of 37.5% stunting, 3.9% wasting, 4.6% overweight, and 13.8% low birth weight.3 Meanwhile, globally, 570.8 million girls and women aged 15 to 49 years (29.9%) are affected by anemia with progress toward reducing the burden of anemia having stagnated over the past decade. This high burden of malnutrition has substantial implications for female morbidity and mortality, adverse pregnancy outcomes, and adverse newborn outcomes.2,4
Nutrition is a core part of health, and without ensuring that everyone has access to high-quality nutrition services, universal health coverage (UHC) cannot be reached.5 UHC is the cornerstone to achieving sustainable development goals (SDGs) 2 and 3 which focus on ending hunger and improving nutrition alongside ensuring healthy lives.5,6 Nutrition and universal health coverage are interlinked, as the burden of malnutrition and non-communicable diseases place a disproportional strain on health systems, threatening their progress.7,8 Universal health coverage can improve nutrition in the population through a more effective provision of curative and preventive services.8
The health sector is central to delivering high-quality nutritional interventions to women and children in low- and middle-income countries (LMICs), and Mozambique is no exception.9 Efforts to improve health systems have highlighted the multiple system building blocks that must be strengthened to improve health systems.10 Focusing on health service delivery, there is a need to ensure access to high-quality health services for the population. A health systems framework proposed by Roberton et. al further unpacks the required components to ensure population coverage of key health services. This framework (Figure 1) proposes that four health system components affect coverage of services (including those related to maternal and child nutrition services), namely: availability of health workers, availability of supplies and equipment, demand for services, and access to services. In improving the provision of health services along with utilization of those services, population coverage with high-quality health services can be achieved, leading to improved health outcomes.7
In Mozambique, the public health sector comprises four levels, namely: primary (urban and rural health centers), secondary (general, rural, and district hospitals), tertiary (hospitals of the provincial capitals), and quaternary (central hospitals and specialized hospitals). Past geographical analysis showed problems of accessibility to the Mozambican primary health care level, with 66.7 % of underserved health services areas.11 In addition, throughout the years, Mozambique has also continuously faced persistent challenges linked to low quality of care, inequalities, the impact of the HIV/AIDS pandemic, and the ability to rapidly adapt to a constantly changing socio-economic environment at the local level, particularly in remote areas.12,13
High-quality health services, particularly related to nutrition interventions, have the potential to accelerate progress toward achieving global targets. However, there are still challenges linked to limited data on nutrition intervention coverage and the quality of nutrition service delivery. In addition, there are no standardized approaches to defining and measuring nutrition service quality in LMICs.7,14,15 Specifically, in the nutrition field, health facility surveys can be used as a powerful tool to describe the availability of services related to nutrition and the readiness to carry out nutritional interventions in health facilities.16,17 The 2018 Mozambique Service Availability and Readiness Assessment (SARA survey) was a census of all health facilities in Mozambique, capturing information on the availability of supplies and equipment, the presence of health workers, and the services, including nutrition services, offered by each facility across the country.18 In this study, we aimed to assess the accessibility and readiness of health facilities to deliver maternal and child nutrition services in Mozambique using the health facility data from the SARA.
METHODS
Using multiple data sources within a Geographic Information System (GIS) environment, we calculated facility readiness to deliver nutrition services, population access to health facilities, and population access to health facilities ready to deliver nutrition services.
Facility data
Facility data from Mozambique’s 2018 Service Availability and Readiness Assessment (SARA)18 were used for this analysis with permission from the Instituto Nacional de Saúde (INS) and the World Health Organization (WHO) in Mozambique. Data were collected between February and April 2018 through a cross-sectional survey of health facilities. The survey included a census of all health facilities in the country and collected data through interviews with key informants at health facilities using the core standard SARA questionnaire, which was adapted to the Mozambique context.18,19 The SARA questionnaire focused on key health services, including maternal, newborn, and child health, communicable diseases, non-communicable diseases, and surgical services. Within the maternal and child health modules, there were specific questions related to nutrition interventions. Global positioning system (GPS) coordinates of all health facilities were collected during the SARA survey.18 For more detailed information on the methods for the Mozambique 2018 SARA, see the final survey report.18
Spatial data
In order to conduct geographic analysis, several data sources were used including:
Population distribution: for the measures of population density, we used high-resolution geospatial data from WorldPop.20,21 Specifically, we used a raster image obtained from WorldPop of the number of people per 100-meter square across Mozambique in 2020, with the country total adjusted to match United Nations population estimates.22,23
Provinces: a polygon shapefile of the boundaries of the provinces in Mozambique was obtained from the National Institute of Statistics (INE) in Mozambique.
Health facility locations: GPS coordinates for all health facilities in the country were obtained from the 2018 Mozambique SARA18 dataset and converted into a shapefile.
Assessment of nutrition readiness
We defined “readiness to deliver nutrition services for pregnant women and children” after reviewing the literature and assessing data available in the 2018 Mozambique SARA survey.18,19,24–26 Based on this information, four maternal nutritional interventions and three child nutrition interventions were selected for the analysis. For each intervention, readiness was defined based on the availability of the service plus key physical inputs required for service delivery, including equipment, diagnostics, and medicines/commodities. The list of interventions and readiness indicators can be found in Table 1. For breastfeeding promotion through prevention of mother-to-child transmission (PMTCT) services, guidelines were considered an essential equipment item as the service is largely based on counseling, and the guidelines serve as a job aid for delivering key counseling messages.27 For each readiness indicator, we calculated the availability of the item nationally as well as by province, facility type, managing authority, and urban/rural. We then created a readiness score per nutrition intervention. A facility was considered “ready” to deliver the intervention if it reported offering the service and had all the items required for service delivery. Facilities received a score of 1 if they were deemed ready and 0 if not deemed ready. Finally, we calculated an overall maternal nutrition readiness score and an overall child nutrition readiness score. For the overall score, a facility received a score of 1 if they were “ready” to deliver all maternal/child interventions or 0 if they were not “ready” to deliver all interventions.
Assessment of facility accessibility
For each pixel in the raster image of population density (i.e. for each 100-meter square across Mozambique), we calculated the distance in kilometers from the center of the pixel to the nearest health facility. We did this using the GPS coordinates of each pixel and facility and the Haversine formula for calculating the great-circle distance between two points given their longitudes and latitudes.28 If the distance from a pixel to the nearest health facility was less than or equal to 10 kilometers, we considered all of the people represented by that pixel to have access to a health facility. If the distance was greater than 10 kilometers, we assumed that none of the people for that pixel had access to a health facility. In this way, we calculated the proportion of people with access to a facility, using those with access as the numerator and all people as the denominator. We chose the threshold distance of 10 kilometers based on previous studies29,30 and a consensus among a multidisciplinary and multisectoral panel from the ´Women and Child Health & Nutrition Platform´ (PSMCN) of the National Health Observatory of Mozambique.31 This panel considered 10 kilometers a reasonable upper limit of distance that one can walk to obtain health services in the country.
The main finding from this study concerns the proportion of people with “access to a ready facility” – an indicator of how well the health system is positioned to provide facility-based nutrition services for pregnant women and children. Similarly to the method described above, for each pixel in the raster image, we identified all of the health facilities within a 10-kilometer radius of the pixel. If no facilities were in range, we assumed that none of the people for that pixel had access to a ready facility. If at least one facility was in range, we observed whether any of the facilities in the range were “ready” to provide a service (per the indicator definitions and readiness methodology described above). If at least one of the facilities within 10 kilometers was “ready”, we considered all of the people represented by the pixel to have access to a ready facility. If not, we assumed that none of the people for that pixel had access to a ready facility. In this way, for each province, region, and for the country as a whole, we calculated the proportion of people with access to a ready facility, for each of the seven nutrition interventions in Table 1.
Ethics considerations
Permission to utilize the 2018 SARA data for this analysis was granted by the Instituto Nacional de Saúde (INS) in Mozambique. This analysis did not involve human subject research. All methods utilized in this study were carried out in accordance with relevant guidelines and regulations. The ´Service Availability and Readiness Assessment´ and linked protocols were granted approval by Mozambique’s Ministry of Health. More information about the primary data collection procedures is available in the Mozambique SARA 2018 report (https://www.afro.who.int/sites/default/files/2020-02/SARA_2018_Invetário_Nacional.pdf). Informed consent was obtained from all survey participants.
RESULTS
Characteristics of health facilities
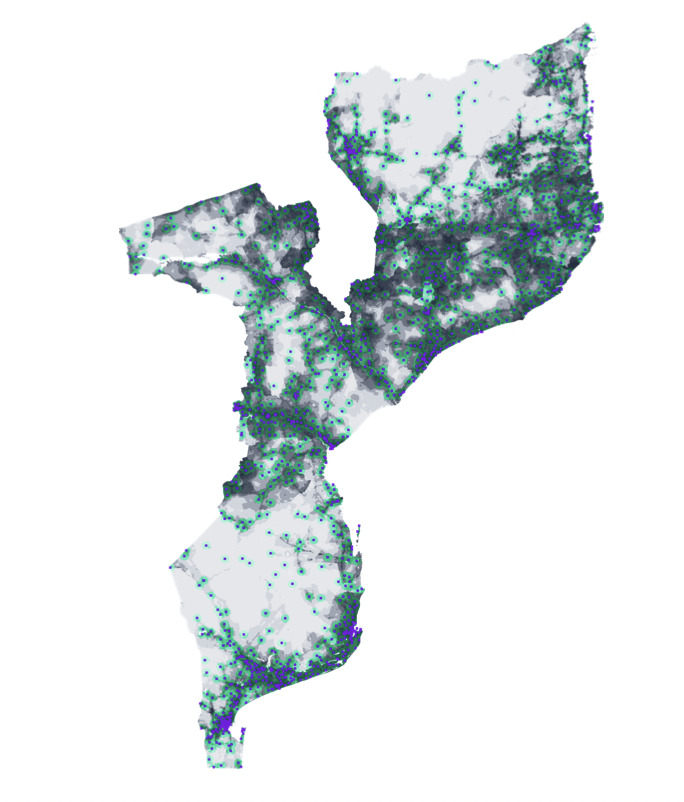
In 2018, there were 1643 health facilities in Mozambique. Most of the health facilities were primary-level facilities (95.9%), under governmental management (99.5%), and located in rural areas (84.4%) (Table 2). Of the 1643 facilities, 91.6% offered antenatal care and 95.0% child preventive and curative care. The location of health facilities and their 10-kilometer radius areas are presented in Figure 2. Our analysis of population density and health facility locations showed that 76.7% of the nation´s population lived within 10 kilometers of a health facility. This proportion varied by province. In Maputo City, 100.0% of the population lived within 10 kilometers of a health facility. In the provinces of Tete and Zambezia, this proportion was 60.3% and 67.9%, respectively.
Availability of nutrition items
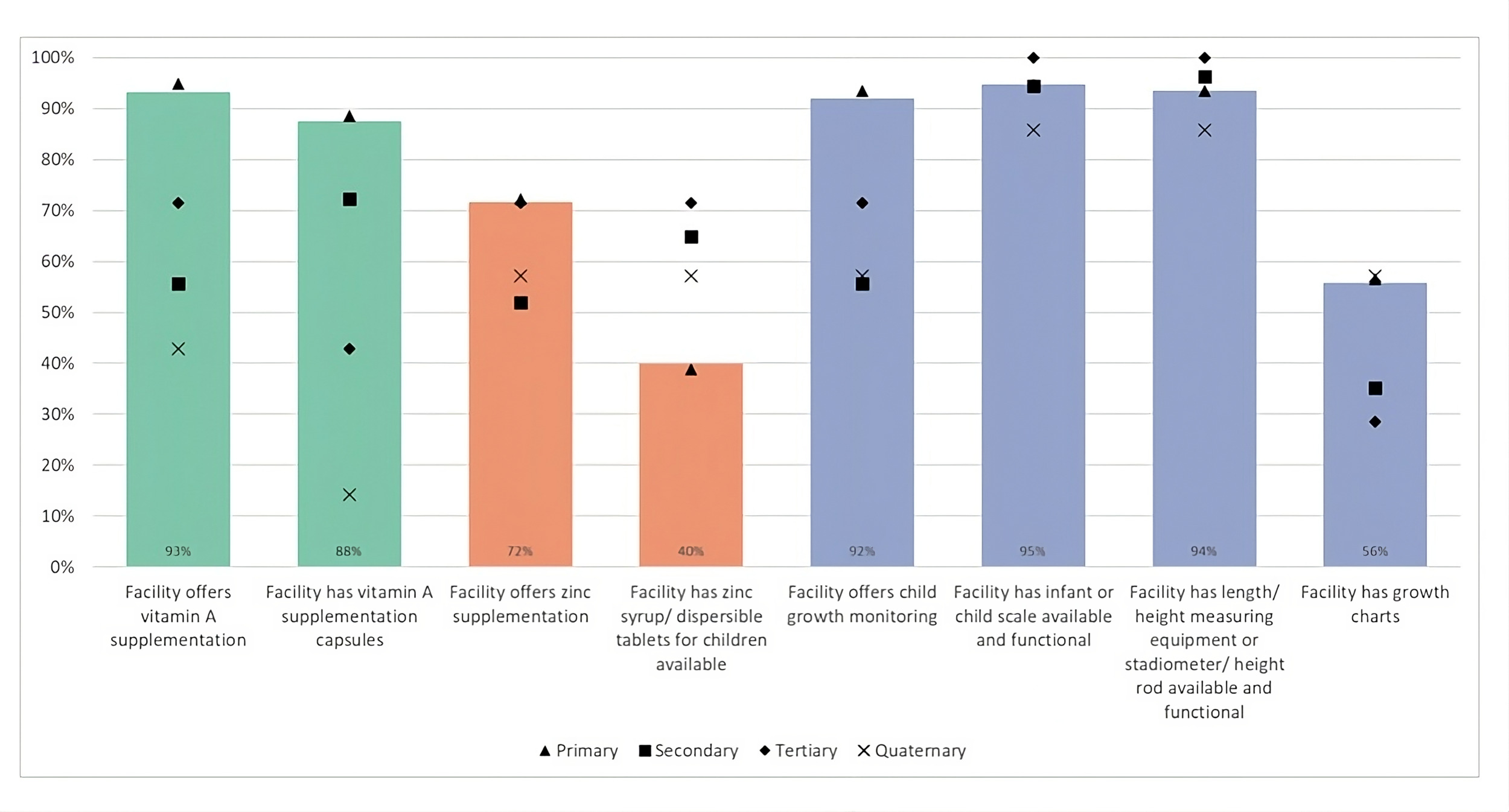
Figures 3 and 4 show the availability of items needed to deliver maternal and child nutrition services at health facilities. For maternal nutrition, only 41.1% of health facilities nationally could conduct hemoglobin testing on or off-site; while most facilities had iron supplements (94.0%) and folic acid supplements (88.0%); and only 43.0% had guidelines for infant and young child feeding counseling. For child nutrition, 87.5% of facilities had vitamin A supplementation capsules, only 39.9% had zinc syrup or dispersible tablets, 94.7% and 93.5% had the equipment to weigh and measure children, respectively, and 55.8% had growth charts. As shown in Figures 3 and 4, the availability of some items varied considerably by facility level, notably, vitamin A supplementation, zinc supplementation, and the capacity for hemoglobin testing.
Health facilities ready to deliver nutrition interventions
We used the same data on the availability of individual items to calculate the readiness to deliver the seven nutrition interventions listed in Table 1. The results of this analysis are presented in Table 2, which shows the proportion of facilities “ready” to deliver maternal and child nutrition interventions by province, facility level, managing authority, and urban/rural. At the national level, only 12.4% of facilities were ready to deliver all four maternal nutrition interventions (anemia testing/iron supplementation, folic acid supplementation, breastfeeding promotion through PMTCT services, and pregnancy growth monitoring). Only 20.4% of facilities were ready to deliver all three child nutrition interventions (vitamin A supplementation, preventative zinc supplementation, and growth monitoring). The service with the smallest proportion of ready facilities was anemia testing/iron supplementation (28.2%), followed by preventative zinc supplementation for children (35.8%) and breastfeeding promotion through PMTCT services (42.8%). The service with the largest proportion of ready facilities was vitamin A supplementation (84.2%). Most facilities were not ready to offer more than two or three of the seven nutrition services. This was true across provinces, facility levels, managing authorities, and urban/rural.
Access to a health facility that is ready to deliver nutrition interventions
Table 3 shows the results of our geospatial analysis, combining the data on population density and distance to facilities with the results on the readiness of facilities to deliver nutrition interventions. At the national level, 29.1% of the population was within 10 kilometers of a facility ready to deliver all four maternal nutrition interventions while 37.3% of the population was within 10 kilometers of a facility ready to deliver all three child nutrition interventions. Pregnancy growth monitoring (73.8%) and vitamin A supplementation (72.4%) were available to the largest proportion of the population. Anemia testing/iron supplementation was the least available nutrition intervention at 45.1% of the population. Overall, the Central region and North region had much lower coverage than the South region across all seven interventions. This is likely due to the high population density of Maputo City and Maputo province, where 100.0% and 95.8% of the population live within 10 kilometers of a health facility. The results in Table 3 for Maputo City show 100.0% for all interventions, which indicates that everyone in Maputo City lives within 10 kilometers of at least one facility ready to provide the nutrition interventions.
DISCUSSION
This study shows that in 2018, 76.7% of the Mozambican population lived 10 kilometers from a health facility. Nonetheless, this differs from previous studies in Mozambique which reported that about 66.9 % of Mozambicans lived in underserved areas (long distance from health facilities) in 2016, thus showing an improvement at the country level.11 In Mozambique, Maputo City remains the only province where 100% of the population has access to a health facility within 10km. This finding is similar to several studies which found high access to health facilities in Maputo City,11,32 this can likely be attributed to the better economic and social development in Maputo City compared to other provinces in Mozambique. Our results demonstrate that access to a health facility is similar to, albeit slightly higher than other countries such as Uganda (71.7%) and Niger (75.0%).33,34 Geographic factors, population density, and socioeconomic disparities may explain the differences in distances to access health facilities in these countries.11,33,34
Despite the increase in the absolute number of health facilities in Mozambique in the last five years,35,36 our analysis suggests that much of the population still does not have access to facility-level nutrition interventions. Similar to other studies on nutrition in Mozambique, our results demonstrate that there are gaps in the Mozambican health system related to the availability and provision of items at health facilities required for adequate delivery of maternal and child nutrition interventions.37–39 We also found that many health facilities offer maternal and child nutrition services nationally, but only a fraction of facilities have the necessary commodities to deliver services such as anemia testing, child growth monitoring, and infant and young infant feeding counseling. This is similar to other studies in low- and middle-income countries which found that the availability and provision of commodities (such as medicines and vaccines) were also a critical problem in Namibia, Zambia, Kenya, Uganda, Malawi, and Bangladesh.40–42 This underscores the key finding that living near a health facility does not guarantee that people will have access to basic nutrition interventions.
The Mozambican health system relies on governmental health facilities to offer maternal and child nutrition interventions.38,43 Our study found that across Mozambique, private providers are lagging behind public facilities in their readiness to offer a comprehensive package of high-quality maternal and child nutrition interventions. The quality of private healthcare is often poor in low-income countries despite the increase in private healthcare provision,44 and our findings show this is likely the case for the provision of nutrition services in Mozambique. In Mozambique, governmental health facilities are the primary source of care and have the ability to provide affordable and appropriate maternal and nutrition interventions. However, to do so, further health systems strengthening is needed to ensure these facilities are sufficiently equipped with the supplies required to deliver basic nutrition services.
Our study highlighted the difficulty of achieving high coverage of interventions in subnational areas where population density is low and health facilities are scarce. In our results, Mozambique’s Central and Northern regions had much lower coverage of all nutrition interventions than the Southern region. This disparity was driven by the low proportion of people within 10 kilometers of a health facility in the Central and Northern regions and by the lower availability of commodities and equipment in these regions. One strategy to increase access to services could be to build new health facilities, however, we show here that large gains could be made by first increasing the availability of supplies at existing facilities. This is aligned with previous studies which suggest that apart from infrastructural development, the provision of essential commodities (such as medicines, equipment, and guidelines) and a skilled health workforce are crucial factors for improving and ensuring the quality of care in health facilities.13 Therefore, ensuring the adequate provision of commodities through strengthening the logistic and management coordination and the appropriate training of healthcare staff can contribute to overcoming the gaps related to health facility readiness in countries like Mozambique.13,42,45,46
Our study has several important strengths and limitations. Monitoring the world’s path towards universal coverage health (UHC) requires data on the coverage of essential health services. In Mozambique, as with other low-income countries, population-level coverage data is not readily available.47,48 Large-scale household surveys are conducted every five years at best. This study adds insights into how health facility and population density data can be combined to give information on the proportion of the population with access to adequate nutrition services. Our coverage estimates indicate the upper bound for the proportion of the Mozambican population that could receive services if they seek care. In future analyses, additional data could be incorporated on care-seeking and demand for services to estimate the proportion of pregnant women and children who actually receive nutrition services.
Our analysis has several limitations. First, we only used distance in kilometers to estimate access to a ready facility, and we did not consider other geographic factors, such as terrain or transport networks. Also, although it is established that geography is one factor that influences healthcare access, there are additional factors that affect access to care, such as the ability to understand the health provider or to participate in informed decision-making; the ability to navigate the healthcare system; language access and availability of translation services; and access to understandable information before, during, and after the health care.49–51 Despite this limitation, we believe our results are still valuable and give an important benchmark for the availability of nutrition interventions to the Mozambican population. In fact, the limitations of our results mean that our estimates are likely too optimistic. Including more factors in the analysis would only decrease the numbers (by introducing more barriers to care), and the results are already alarming for many interventions in our analysis. We believe that our findings can contribute to improving the planning and implementation of maternal and child nutrition services (such as growth monitoring, anemia testing, and iron supplementation) at health facilities in Mozambique. The second limitation of our analysis is that it focuses on delivering nutrition interventions at health facilities and does not consider the potential for delivering nutrition interventions through community health workers or other strategies such as fortification or campaigns. This limitation is largely due to the fact that the SARA data, our primary data source for this analysis, does not contain this information. Thus, our results purely reflect the readiness of health facilities, which was the focus of the study. Future efforts could also incorporate data on the readiness of community mechanisms to deliver nutrition services.
CONCLUSIONS
Improving nutrition in Mozambique will require multisectoral effects within and outside the health system. Although facility-based interventions are insufficient, they are necessary to ensure that all mothers and children in Mozambique achieve optimal health. To achieve high coverage of nutrition interventions, facilities need a full suite of commodities and equipment, including iron, zinc, folic acid, and vitamin A supplements, capacity for hemoglobin testing, and equipment for weighing and measuring children. Currently, too many facilities in Mozambique have only some of these supplies, meaning that only a minority of the children and pregnant women will receive effective nutrition services when they need them.
ACKNOWLEDGEMENTS
We want to thank Acácio Sabonete, António Junior, Amisse Momade, Amélia Chiche, Egídio Cueteia, Euridsse Amade, Hélder Macul, Hilénio Sabão, Graça Salomé, Maria Patrícia Gonçalves, Maria Vilma Josefa, Marla Amaro, Nora Nhacuto, Ofélia Simão, Paulino da Costa, Sheila Nhachunge, Rui Mondlane and Rui Langa. The first author wishes to thank and acknowledge Isabel Craveiro, Luís Varandas, the Calouste Gulbenkian Foundation, and the Foundation for Science and Technology (UI/BD/151065/2021) for supporting her research project program.
ETHICS STATEMENT
Permission to utilize the 2018 SARA data for this analysis was granted by the Instituto Nacional de Saúde (INS) in Mozambique. This analysis did not involve human subject research. All methods utilized in this study were carried out in accordance with relevant guidelines and regulations. The ´Service Availability and Readiness Assessment´ and linked protocols were granted approval by Mozambique’s Ministry of Health. Informed consent was obtained from all survey participants.
DATA AVAILABILITY
The ´Service Availability and Readiness Assessment 2018 Mozambique´ dataset can be requested from the Instituto Nacional de Saúde from Mozambique through this Google form (https://docs.google.com/forms/d/e/1FAIpQLSfcaILV-RDz3rVKhhA7V6OsblIQ0FPW1Z1ECaCVHN1SwTOQPQ/viewform). After completing the form, email [email protected]. The Mozambique population raster image used for this analysis is publicly available from WorldPop (https://www.worldpop.org). The country and province shapefiles are publicly available via the Humanitarian Data Exchange (HDX) (https://data.humdata.org/dataset/cod-ab-moz).
FUNDING
The data analysis workshop with PSMCN members and Johns Hopkins University was supported by the European Union through a grant (FED/2017/385-650) to the Instituto Nacional de Saúde. The views expressed in this paper are from the own authors and not the official position of the institutions or funder.
AUTHORSHIP CONTRIBUTIONS
TR, AS, TS, and RC conceptualized and designed the study. AS and TR performed the preliminary data analysis. RC, CS, JS, EM, EI, AA, and EM performed the final data analysis with support from AS, TS, and TR. All co-authors contributed to the interpretation of the findings. RC wrote the initial draft of the manuscript. RC, AS and TR contributed to revising and editing it. All authors approved the final version and agreed to the published version of the manuscript.
DISCLOSURE OF INTEREST
The authors completed the ICMJE Unified Competing Interest form (available upon request from the corresponding author) and declare no conflicts of interest.
CORRESPONDENCE TO:
Réka Maulide Cane
Email: [email protected]
ORCID: 0000-0001-8209-4976