Globally, HIV remains a significant public health problem. The 2020 Joint United Nations Programme on HIV/AIDS (UNAIDS) estimates that 37.6 million people live with HIV globally. Cumulatively, it is estimated that 77.5 million and 34.7 million people have been infected with HIV and died of AIDS, respectively, since the start of the epidemic.1 Whereas the number of people dying of AIDS-related illnesses fell by 39%, from 1.2 million in 2010 to 690,000 deaths in 2020, new infections continue to occur at a high rate. In 2020 alone, 1.5 million new infections occurred.1 The COVID-19 pandemic has impacted the HIV epidemic.2 A UNAIDS report indicates that the risk of dying from COVID-19 is double among people living with HIV compared to the general population,3 and the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFTAM) reports a 41% reduction in HIV testing, which is an entry point for HIV and AIDS care, between April and September 2020 compared to the same period in 2019.4
Furthermore, the UNAIDS notes that the gains made in HIV prevention will likely be eroded by the COVID-19 pandemic.2 The burden of HIV and AIDS has a considerable opportunity cost, especially in low-income countries. In 2020 alone, US$26.2 billion was required to combat HIV and AIDS globally, but only US$18.6 billion was available.1 HIV-related care costs are estimated to reach US$40 billion annually by 2030.5
Africa carries a disproportionate burden; it is the continent most impacted by HIV and AIDS, accounting for two-thirds of the global HIV cases. At the end of 2018, it was estimated that 25.7 million people were living with HIV, and 1.1 million new infections were registered in Africa. Within Africa, eastern and southern Africa are the most affected regions, with 20.6 million people (55% of the cases) living with HIV.1 To achieve the 2016 United Nations resolution of ending HIV and AIDS as a public health problem by 2030, UNAIDS estimates that investments of up to US$29 billion are required for low- and middle-income countries (LMICs) by 2025.1 Expenditure on HIV-related activities accounts for 20% of the total health budget in Sub-Saharan Africa.6
Donations from high-income countries that are least affected by HIV remain a significant source of funding for HIV and AIDS activities in LMICs.6 Although there has been an increase in domestic funding that currently accounts for 57% of the resources,1 overall, the total resource envelope continues to decline. Funding from bilateral governments remained the same between 2008 and 2019 despite a 25% increase in people living with HIV and AIDS in LMICs. Funding from donors such as the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) has been instrumental in reducing HIV-related mortality in low- and middle-income countries.7
Atun and Chang8 estimate that nine Sub-Saharan countries will require US$261 billion between 2015 and 2050 to avail all people living with HIV of antiretroviral therapy (ART), a need that is too substantial to be met through the current funding streams. For instance, Uganda estimates it will require US$8.2 billion between 2021 and 2030 to prevent 130,000 new HIV infections and 51,000 AIDS-related deaths.9 This has significant resource implications for other public sectors and calls for other options to provide sustainable support for HIV and AIDS interventions in the most affected countries. Out-of-pocket payments are one of the options.
It is not well documented if people in need of various HIV prevention, care and treatment services would be willing to pay for them as an alternative approach to sustain these services in the most affected countries. The primary objective of the review is to determine the extent of the willingness to pay (WTP) for HIV services. The willingness-to-pay method is one of the tools used to measure health benefits in cost-benefit analysis by eliciting the consumer’s value for non-market health goods.10 The secondary objectives include determining the methods used to investigate the WTP for HIV services, the type of HIV services evaluated using the WTP and the factors that influence the WTP for HIV services in Africa. In this review, HIV services are operationally defined as World Health Organisation (WHO)-approved services for diagnosing, preventing, treating, and supporting HIV and AIDS.
METHODS
Eligibility criteria
To be eligible for inclusion in the review, studies had to meet the following inclusion criteria: 1) studies had to evaluate WTP, 2) about HIV and AIDS services, 3) conducted in Africa, and 4) were published in English. The exclusion criteria included 1) studies that used preference elicitation methods other than WTP, 2) studies that were not about an HIV service, 3) studies about tuberculosis among people living with HIV, and studies not published in English. The review was restricted to Africa for two reasons. First, Africa is the most affected continent,11 highly dependent on HIV donor resources.12 Second, socio-economic status is documented as influencing WTP; thus, the inclusion of studies from other continents, such as Europe and North America, has the potential to skew the findings, a limitation noted in other systematic reviews.10
Information sources and search strategy
An electronic search was conducted in PubMed, EMBASE, Web of Science, and CINAHL using search terms presented in Online Supplementary Document Table S1. A manual search for additional articles and grey literature was conducted on the International AIDS Society, Avert, and World Health Organisation websites. The references of relevant published articles were also searched for additional articles. The databases were searched from inception until 30 June 2023. Alerts for new articles were created for the electronic database before the final data analysis was completed. All identified papers were managed using EndNote 20™ software.13 The review protocol was registered with PROSPERO under number CRD42021275215.
Data abstraction and synthesis
Data extraction was performed independently and sequentially by the authors. A thematic descriptive analysis was used to synthesize findings because of the heterogeneity of the retrieved articles. With a standardized data abstraction template that was pilot tested prior to use, data about the authors, the country of the study, the theory used to inform the study, HIV thematic area (diagnosis, prevention, treatment), the objective of the study, population, sample size, survey method, WTP elicitation method, type of statistical analysis conducted, factors associated with the WTP, and data on the sufficiency of the amount to pay for full service were extracted. Due to the type of studies included, mixed methods were used to synthesize data. Quantitative data were synthesized using descriptive statistics, and qualitative data was synthesized through a narrative approach. The methodological quality of the included articles was assessed using the JBI critical appraisal tools.14,15 The findings are presented using tables and graphs.
RESULTS
Study selection
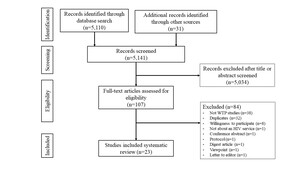
A total of 5,141 records were retrieved, with 5,110 articles identified from databases and 31 documents retrieved from other sources, including references to other articles and websites of HIV and AIDS organisations. The number of records was reduced to 107 articles after screening for the key terms in subject headings, titles, and abstracts. Of the 107 records available for review, 84 were excluded for the following reasons: 38 articles were not about willingness to pay studies and used other preference elicitation methods, such as willingness to accept; 32 were duplicates; and eight were about willingness to participate. Other reasons for excluding articles were study protocol,16 not evaluating an HIV service,17 a digest article for an article that was already included,18 a viewpoint,19 and a letter to the editor about an article already included.20 Twenty-three articles (23) were available for data extraction.
Study characteristics
The studies’ characteristics are presented in Table 1. The articles were published between 2000 and 2022, with the majority (13; 56.5%) published between 2016 and 2020. The studies were conducted in ten African countries, including Nigeria, which had ten21–30; Kenya, which had six23,31–35; Tanzania36–38 and Zimbabwe,23,39,40 which each had three; and one article each from Zambia,23 Uganda,41 Cote d’Ivoire,38 South Africa,23 Cameron,42 and Ghana,43 as shown in Figure 2. Two studies were conducted in multiple countries.23,38
The total sample size of the included studies was 20,783, ranging from 26 participants37 to 6,566 participants for a multi-country study.23 The majority (20; 87%) of the studies were conducted amongst users of the service under study, such as people living with HIV (PLHIV) who are on antiretroviral therapy (ART) and condom users. Two studies22,34 were conducted amongst people drawn from the general population. One study21 was conducted among university students. Among the retrieved articles, only one22 mentions the theory underpinning the study.
Willingness to pay for HIV studies in Africa mainly uses face-to-face interviews to collect participant data. Most studies (18; 78.3%) used interviewer-administered face-to-face interviews to collect data, while three studies23,38,39 (13%) used interviewer-administered electronic questionnaires to collect data. Only two studies used self-administered questionnaires.33,35
Seven (33.3%) articles did not explicitly state how WTP figures were elicited. Among the fifteen articles that mentioned the elicitation method, 46.7% (7/15) used the bidding game,21,23,25,29,30,35,42 26.7% (4/15) used the payment card,22,27,31,36 and one study each addressed multiple price lists,37 open-ended questions,43 bidding games with minimum and maximum,26 and structured haggling.28
The findings indicate that statistical analysis to determine factors that influence WTP was mainly done using regression analysis (94.7%, 18/19) among the quantitative studies explicitly stating the data analysis used. The chi-square test27 was used in one study.
The scope of HIV services investigated using the willingness-to-pay approach in Africa.
Table 2 presents the themes and types of HIV services that have been investigated using the WTP approach in Africa. Among the articles retrieved and eligible, 30.4% (7/23) covered the theme of HIV diagnosis,21,22,30–32,37,38 39.1% (9/23) the theme of HIV prevention,23,24,26,27,30,33,34,39,43 and 34.9% (8/23) the theme of HIV care and treatment.25,28,29,35,36,40–42 Regarding HIV diagnosis, the articles are evenly distributed between WTP for HIV counselling and testing (HCT) and WTP for HIV test kits, with one article about HIV self-testing. There is an uneven distribution across the types of services under the themes of HIV prevention and HIV treatment. Under HIV prevention, 33.3% (3/9) of the articles are about the Prevention of Mother-to-Child Transmission of HIV (PMTCT),26,27,43 33.3% (3/9) are about WTP for condoms,23,30,39 22.2% (2/9) on PrEP30,33 and one article each for voluntary medical male circumcision,34 and cervical cancer screening.24 Seven articles (87.5%) on the treatment theme were about ART, while one was about general HIV care services.35
Willingness to pay for HIV services.
All twenty-three articles that were reviewed found that people were willing to contribute to the payment of HIV services but to varying levels. From the twenty-two quantitative studies that reported on the percentage of people who are willing to pay, the proportion of people willing to pay for various HIV services ranged from 34.3% for payment of ART in Nigeria25 to 97.1% for payment of PMTCT services, also in Nigeria.26 Only two studies25,34 found that less than 50% of people were willing to pay for services. More people were willing to pay for HIV diagnosis, with a median of 80% compared to HIV prevention (73%) and HIV treatment (67.7%), as shown in Figure 3. Studies on HIV prevention reported the highest proportion of people willing to pay26; however, they also have the widest range (from 39.6% to 97.1%) of the proportion of people willing to pay compared to other HIV services. The majority (16/22, 72.7%) of the studies that indicate the amount people are willing to pay show that it is less than the actual cost of the full service in a real market. Only one study23 reports willingness-to-pay amounts higher than the market value. Five articles (22.7%) did not state if the amount was below, equivalent, or more than the actual market value.
Factors that affect the Willingness to pay for HIV services in Africa.
Figure 4 shows the themes influencing the WTP for HIV services in Africa. Socio-economic status was the most common theme cited as influencing WTP. Variables under the category of socio-economic status include income, ability to pay, employment education, salary, and male gender. The second, and the third most common themes, with a frequency of nine and eight mentions, were knowledge and people’s beliefs, respectively. The cost of the item or service, perceived benefits and the influence of peers were other themes cited as influencing factors of the willingness to pay. Detailed information on the factors that influence willingness to pay for HIV services in Africa is shown in Table 3.
Qualitative findings
Of the twenty-three articles that were reviewed, only one used a qualitative methods design.41 Using semi-structured key informant interviews and focus group discussions, Twimukye, King, Schlech, Zawedde, Kakaire and Parkes-Ratanshi41 explored the attitudes and perceptions of HIV patients and their willingness to pay using a fee-based after-hours HIV clinic in Uganda. The key informants were people with high HIV stigma, high net-worth individuals, busy individuals and staff working at the clinic. The focus group discussions comprised randomly selected individuals attending the clinic on a given day. The study found a varied willingness to co-pay, with some respondents willing to pay as high as Uganda Shillings 40,000 (approximately US$11) per visit. The themes associated with WTP include the perceived benefits of attending a special clinic, such as privacy and short waiting time, convenience for those in formal employment, and giving people another choice. The themes associated with a negative attitude towards payment mentioned in the article include the perceived fear that fees might become mandatory for all HIV patients, including those attending the general clinic, poor quality services for those unable to pay and the belief that HIV services should be offered free. The other reason cited for the unwillingness to pay is that the clinic is not a one-stop center for additional services, such as being a prostate cancer clinic.
Quality assessment of the studies
The articles were assessed for methodological quality using components of JBI tools applicable to the retrieved studies. The quantitative articles were assessed for; 1) the presence of clearly defined criteria for inclusion in the sample, 2) a description in detail of the study subjects and the setting, 3) measurement of the exposure validly and reliably, 4) objective and standard criteria used for measurement of the condition, and 5) use of appropriate statistical analysis. The qualitative paper was assessed for; 1) congruity between philosophy and methodology, 2) congruity between methodology and methods, 3) influence of the researcher on research and vice versa, 4) representation of the Respondent’s voice, and 5) ethical approval. The retrieved articles were scored as “Yes”, “No”, or “Unclear”. Items that scored “Yes” were assigned one point, while articles that scored “No” were assigned a score of zero. The “Unclear” items were not scored. The total maximum score was five. Articles that scored 4-5 were ranked as high quality, 2-3 as medium quality and 0-1 as low quality. All articles that were scored as medium to high quality were included in the final review. The scoring system was adapted from other studies.45 No study had an item marked as “No.” Nine (40.9%) studies that had all items marked as “Yes” and 10 (45.5%) studies that had four “Yes’” and one “Unclear” domain were classified as being of high quality. Three studies (13.6%) had two “yes” and three “unclear” and were classified as medium quality. Both high- and medium-quality studies were included in the final review.
DISCUSSION
This systematic review investigates the willingness to pay for HIV services in Africa. The review finds evidence of willingness to pay for HIV services even though the amount is insufficient to pay for the full service at market value—the proportion of people willing to pay ranges from 34.3% to 97.1%. A greater proportion are more willing to pay for HIV diagnosis compared to prevention and treatment. This may be attributed to the fact that HIV diagnosis costs much less compared to HIV prevention and treatment service, and thus, many more people are able to afford it. Several factors are significantly associated with the willingness to pay for HIV services. Among the factors, socio-economic status (including income, the ability to pay, employment, education and status) was the most frequently mentioned, followed by knowledge and beliefs about the HIV service or product. Other factors include the level cost of service or product, perceived benefits and the influence of other people. These factors are similar to those previously reported.10,45,46 However, the findings must be interpreted in the broader context of the prevailing global economic situation and foreign exchange rates for imported commodities.20 Further, willingness to pay for healthcare is subject to be used as a political tool to seek free services. Therefore, the findings need to be contextualised to the prevailing political situation.
To the best of our knowledge, this is the first review on this topic. The review covers the methods used in WTP studies for HIV services in Africa and the factors associated with the willingness to pay. Twenty-three articles that met all the inclusion criteria and none of the exclusion criteria were included in the final review. The main reason for excluding studies is that they focus on the trade-off for specific HIV services using the discrete choice and willingness to accept elicitation methods but not to assess the willingness to pay for the services.
The review includes articles not in three recent reviews.10,47,48 The majority (73.9%) of the articles were published between 2016 and 2022. This coincides with the period when donor funding for HIV started to stagnate or fall and, hence, may relate to the interest in exploring alternative sources of funding.12 All three thematic areas of HIV diagnosis, prevention and treatment were investigated using the WTP approach. Although HIV prevention had the highest number of articles amongst those included in the review, within the HIV prevention scope, there are few HIV prevention services covered by WTP studies. For instance, voluntary medical male circumcision a cost-effective intervention for HIV prevention had just one article. HIV prevention remains the hallmark for long-term control of HIV and AIDS,49 and thus, that alternative measures for sustaining HIV prevention interventions in Africa must be explored.
We find that using the WTP to investigate HIV services is a relatively new concept. Other than Nigeria and Kenya, in most countries, less than three studies have been conducted and further research into why this is the case is needed. We find incomplete reporting on the methods used in WTP studies. The theories underpinning the studies and the methods used to elicit willingness to pay are two notable items not consistently reported in the reviewed articles. There is little mention of the theoretical approaches to study willingness to pay for HIV services in Africa. Only one study about WTP for HIV services in Nigeria explicitly states the theory underpinning the research,22 while another40 states the conceptual framework but not the theory. Research should ideally be guided by an appropriate theory.50 Adekunjo, Rasiah, Dahlui and Ng22 used the neoclassical economic theory that assumes people to be rational and, thus, make decisions that maximise their utility.51,52 The neoclassical economic theory has been critised for assuming humans are always rational; in contrast, individuals sometimes make decisions that are not in their best interests.53 Rice53 recommends integrating behavioural economic tools in health economics to address the shortcomings of the neoclassical theory. The available evidence indicates incomplete documentation on the method for eliciting WTP. Only fifteen of the twenty-two quantitative studies (68.2%) fully mention the elicitation method for obtaining the WTP. The bidding game is the most common method used among the retrieved articles, similar to what another systematic review found.10
Most (87%) of the included studies are conducted amongst users of the service being evaluated. This is similar to what was found in a systematic review of WTP for HIV prevention technologies.48 Although Foreit and Foreit54 recommend that WTP studies for clinical services be conducted among people attending clinics, conducting WTP studies amongst people already using the service and who already find utility in the service may lead to systematic bias.55
Among the articles retrieved, only one uses a qualitative method study design,41 perhaps unsurprising because WTP is largely a quantitative tool. This qualitative article shows evidence of WTP for an after-hours HIV clinic. The themes favouring WTP include perceived benefits such as privacy, less waiting time, and the convenience of attending an after-hour clinic. The themes reported by participants who were not willing to pay include perceived threats such as fear that payment might become mandatory, including the general clinic, poor quality services for those in the general clinic who are unable to pay for the after-hours clinic, and the belief that HIV services should be free. The qualitative findings41 highlight the importance of exploring other factors beyond the ability to pay that influence willingness to pay. The key informants, who were high net worth individuals and, thus, more likely to be able to pay, are concerned not only about the quality of care in the after-hours clinic but also in the general clinic where those unable to pay to seek care. These findings are similar to what Steigenberger, Flatscher-Thoeni, Siebert and Leiter10 found that perceived benefits and fears/threats are among the factors that influence WTP for health services.
Almost all the studies (90.3%) used interview-administered questionnaires to collect data, with only two studies reporting the use of self-administered questionnaires.33,35 Interactive data collection formats that allow clarifying questions and probing for higher amounts are generally recommended for WTP.56,57
This review has several strengths compared to other recent reviews. We attempted to address the limitation of excluding qualitative articles from preference elicitation studies, as acknowledged in the systematic review by Beckham, Crossnohere, Gross and Bridges.48 Our search for evidence included grey literature sources that were omitted by other reviews.47,48 All the studies included were classified as medium to high quality. However, our review is not without limitations. Willingness to pay is largely a quantitative approach. Although we aimed to include qualitative articles, there is a possibility that our search criteria may not have been sensitive enough, and thus, we may have missed some articles that used qualitative methods. We restricted our search to only English articles, which may have excluded important articles in other languages. One of the limitations of contingent valuation studies is the assumption that stated preference equates to actual payment,20 which may not be the case, and this systematic review is no exception; thus, the findings should be interpreted with some caution.
CONCLUSIONS
This systematic review has provided evidence of willingness to pay for HIV services in Africa. More people are willing to pay for HIV diagnosis than HIV prevention and treatment. The amount people are willing to pay is insufficient to cover the full cost of services, which is an important potential consideration when determining how to fund a sustainable HIV service in the future. Several factors, including socio-economic status, knowledge, and beliefs about HIV services, influence the willingness to pay for HIV services in Africa. These findings are important in developing policies for sustaining HIV services in a world where donor funding is declining.
Given the constrained public health budgets, we recommend that Ministries of Health consider offering HIV testing services at a fee since it has more people willing to pay for it and reserve the public resources for HIV and AIDS prevention and treatment. Several factors, including equity to prevent financial impoverishment, knowledge about the services, and beliefs about some HIV services, should be considered before introducing fee-for-service HIV services. We recommend further research to identify the reasons that inform WTP decisions and to address the methodological gaps in the available studies.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Funding
No funding was received.
Authorship contributions
BBJ conceived and planned the review. BBJ led the design of the review. LM and HB contributed to the design. BBJ developed the study tools and instruments, collected and analysed the data, and led the implementation of the study. LM and HB contributed equally, reviewed and supervised all study stages, and edited the manuscript. All authors read and approved the final manuscript.
Disclosure of interest
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests / declare the following activities and relationships.
Additional material
An additional file that contains the search terms is attached as ONLINE SUPPLEMENTARY DOCUMENT.
Correspondence to:
John Byabagambi
Lancaster University
Bailrigg, Lancaster LA1 4YW, United Kingdom
[email protected] / [email protected]