Working in resource-constrained settings presents many challenges. Healthcare systems may be understaffed,1 and advanced care options can be cost prohibitive for many individuals.2 Additionally, pre-hospital care is fragmented outside of metropolitan areas and patients frequently present to healthcare facilities in later stages of their disease processes, resulting in an overall sicker population of patients seeking care compared to populations in high income countries (HIC).3 In the 21st Century, there have been increasing numbers of individual and institutional efforts from HIC to support healthcare in low-to-middle income countries (LMIC).4 Often this takes the form of visiting clinicians and educational partnerships, as well as donations of equipment such as technology like ventilators and monitors, or consumables like certain drugs or airway and vascular access equipment. The arrival of these items can mean life-saving treatment for patients but also necessitates creativity on the part of the receiving institutions and clinicians to implement this equipment safely and cost-effectively. In this paper we present an example from a faith-based, East African mission hospital of a challenge and ensuing solution in hopes of encouraging others working in resource-constrained settings to develop creative, patient-centered solutions to the unique challenges these environments present.
The COVID-19 pandemic catapulted the need for critical care services to the forefront of healthcare discussions around the world. Social expectations and the images of hypoxic patients accelerated the sense of urgency for expanding access to organ-supporting technologies.5 At the onset of the pandemic, there were estimated to be 256 mechanical ventilators in the country of Kenya that could be made available for patients experiencing severe respiratory failure.6 As hospitals such as our own expanded oxygen delivery capacity and added services like mechanical ventilation and hemodialysis, the utilization of other consumable goods increased. In our institution, this meant an increased frequency of central venous catheter (CVC) placement, for both resuscitation and management efforts in the critically ill, as well as placement of temporary catheters for patients in need of emergent hemodialysis, a relatively new service in our region.
CASE DESCRIPTION
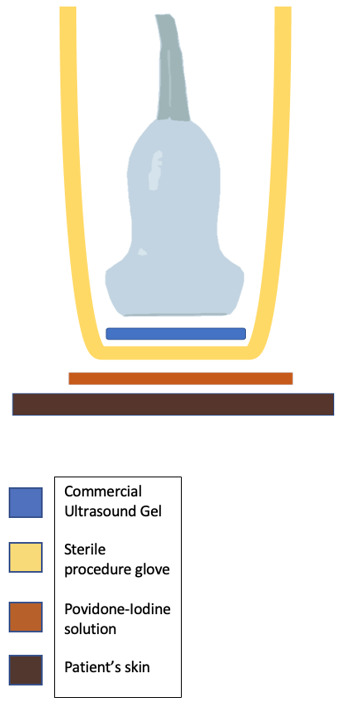
As access to ultrasound has expanded with the advent of handheld devices over recent years, CVC placement has become safer.7 In our hospital, we faced the question of how to provide ultrasound-guided CVC placement while maintaining appropriate sterility. Sterile probe covers and sterile ultrasound gel, previously a rarity in the medicine department, were needed for safe placement of ultrasound guided in-dwelling catheters. As an alternative to purchasing novel items and risk adding expenses and workhours to the procurement process, our team looked within our existing resources to come up with a solution. We began using povidone-iodine solution as a gel-substitute to serve as a medium for ultrasound image acquisition. We also were able to utilize sterile gloves from the gynecology service–which are longer than the gloves typically used in sterile procedures–to serve as sterile probe covers (see Figure 1). With this we have been able to perform CVC placement with ultrasound-guidance while maintaining sterility during the procedure without the need to procure any new consumable goods for the operation of our critical care and dialysis services.
DISCUSSION
We believe this practice is worth sharing as an example of creative problem solving in resource-constrained settings. Admittedly without objective data, it is the authors’ opinion that maintaining a stock of sterile equipment for specific procedures performed infrequently adds financial and logistical burdens to hospitals in resource-constrained settings that overall might outweigh the benefits of offering the procedure. Healthcare teams in similar environments may find this practice helpful in improving procedural technique while reducing the burden of additional equipment costs that may come with expanding services. In our institution, povidone-iodine solution is readily available and is the cleaning solution of choice for sterile procedures,8 so it was already a part of our procedural setup. While saline has been compared with ultrasound gel,9 we were unable to locate any reports of Povidone-iodine solution being used as a gel-substitute for ultrasound-guided CVC placement, leading us to believe that while we may not be the first to try this approach, we should share our ideas with the broader healthcare community. In our context, a few ounces of povidone-iodine is already accounted for in these procedures and is less of an investment than a bottle of sterile saline. The povidone-iodine solution seems to provide comparable image acquisition and clarity to commercial gel, with examples provided (see Figure 2). Although we have no data available in our facility to compare before and after implementing this approach, after more than 40 procedures performed using this approach, our cannulation success rate with ultrasound guidance does not appear to have changed in a negative way with this approach. The authors do note that with prolonged procedure time, the povidone appears more apt to disperse and dry out, requiring re-application more frequently than commercial ultrasound gel. While this may not represent a problem for the experienced and efficient operator, trainees in the early stages of performing the procedure frequently require extra time, and in this scenario our approach could require frequent re-application of povidone-iodine during cannulation, possibly adding steps to the procedure. Despite this concern, our experience thus far in the teaching environment has been one of success, with the strategy being adapted and easily reproduced by trainees. The use of the longer sterile gynecology gloves did add an item to the list of equipment needed for the procedure, but a sterile cover is needed regardless if ultrasound guidance is to be utilized. With this approach we can use an item that is readily available and simple to stock in our facility. The authors note that an objective outcomes assessment was not possible due to lacking a mechanism to track patients through hospitalization and after discharge, but we hope that by sharing our approach, others would be encouraged to search for creative solutions to healthcare challenges unique to the resource-constrained setting.
CONCLUSION
As healthcare systems in LMIC advance, they will interact with increasingly complex procurement procedures and supply chains, many of which are fragile in the settings of war and pandemic affecting global markets.10 Creative, effective, and most importantly safe solutions for our patients’ healthcare challenges will continue to be of utmost importance as healthcare systems in resource-constrained environments continue to advance.
Acknowledgements
The project was reviewed by the AIC Kijabe Hospital ISERC and received an exemption.
Funding
The authors received no funding in the course of developing and writing this manuscript.
Authorship Contributions
WMS: initial project development, image gathering, manuscript writing
PMOA: image gathering, manuscript writing
Competing Interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.