COVID-19 infections were first reported in Wuhan City, Hubei Province, China, in December 2019, leading to strict nationwide lockdowns being implemented across the globe to reduce transmission of the virus.1 On Mar 18 2020, the Malaysian government declared a state of epidemic emergency and imposed the first Movement Control Order (MCO), which resulted in the suspension of face-to-face learning in universities. Malaysia has been hit by three waves of the COVID-19 pandemic over the past 15 months, which has greatly disrupted teaching in many institutions, especially medical schools. As a result, universities had to migrate classes online to adapt to the new normal, ensuring continuity of education.2
The numerous disruptions to education delivery amidst the pandemic have affected students’ psychological well-being. Negative impacts on mental health were prevalent in studies conducted amongst medical students in various countries, with findings that most students were experiencing deterioration in their mental states.3–5 It was apparent that students concerned about transitioning to e-learning were at greater risk of anxiety and depression.4 Conversely, improved psychological welfare in students was found with lower rates of depression and anxiety reported upon adjusting to online education.6 Many variables could contribute to escalating or alleviating stress levels of an individual student, especially in the era of the pandemic, and it was clear that the shift to e-learning played an important role too.7
After one year of transitioning to e-learning, we aim to explore the pandemic’s effects on mental health among students at Newcastle University Medicine Malaysia (NUMed).
METHODS
Study design and participants
A cross-sectional study using a convenience sampling of university students was conducted between Jul 12 and Aug 12 2021. All students registered with NUMed during the academic year 2020/2021 including medical students from Year 1 to 5, Biomedical Science students in Year 1 & 2 and Foundation Programme were invited to participate in the study. Students who were taking a year out or undergoing an Intercalation programme in another campus were not invited to participate in the study.
The self-administered online Google form questionnaire which comprised of sociodemographic, mental health assessment questionnaires (depression, anxiety, somatic symptoms and stress), clinical teaching, and concerns about COVID-19, was sent through an embedded link via email invite to all students.
Informed consent was obtained from the students before participation, and the survey was anonymized to ensure confidentiality. Prior to the survey, a pilot study was undertaken with a sample of students to assess the suitability and understanding of the questions asked.
Measurements
Anxiety
Anxiety disorders were screened using the 7-item Generalized Anxiety Disorder (GAD-7) scale. The total score for the GAD-7 ranges from 0 to 21 and was interpreted as follows: 0–4 scores (Minimal), 5–9 scores (Mild), 10–14 scores (Moderate), and 15–21 scores (Severe). We defined a score of 5 or more as anxious. GAD-7 has demonstrated excellent internal consistency (Cronbach’s ɑ = 0.91).6
Depression
The 9-item Patient Health Questionnaire (PHQ-9) scale was used to assess depression. Participants reported their responses on a 4-point scale, with higher scores indicating worse symptoms. The total score for the PHQ-9 ranges from 0 to 27 and was interpreted as follows: 0–4 scores (Minimal or none), 5–9 scores (Mild), 10–14 scores (Moderate), 15–19 scores (Moderately severe), and 20–27 (Severe). A score of 5 or more was considered depressed. PHQ-9 has shown good internal consistency (Cronbach’s ɑ = 0.89).6
Somatic symptom
The Patient Health Questionnaire-15 (PHQ-15) scale of 15 items was used to assess common physical symptoms. The total PHQ-15 score ranges from 0 to 30, and scores of equal or more than 5, 10, 15 represented mild, moderate and severe levels of somatization, respectively. We defined a score of 5 or more as having somatic symptoms. PHQ-15 has shown good internal consistency (Cronbach’s ɑ = 0.88).6
Stress
The Perceived Stress Scale (PSS-10) is a 10-item questionnaire used to assess stress levels. The total PSS-10 score ranges from 0 to 40 and interpreted as follows: 0-13 scores (low stress), 14-26 scores (moderate stress), 27-40 scores (high perceived stress). We defined a score of 14 or more as perceived stress. PSS-10 showed good internal consistency (Cronbach’s ɑ = 0.85).8
Participants reported their responses for clinical teaching on a 5-point Likert scale from “1 = Not helpful at all” through to “5 = Extremely helpful” and concerns over COVID-19 issues was measured on 5-point Likert scale of “1 = Never concerned” to “5 = Very concerned”. The participants were able to check all the boxes that apply for the type of support students needed from university i.e. financial, livelihood, healthcare, mental health, technical and clear information. We considered the answer as “Yes” if the box is checked and “No” when the box was unchecked.
Statistical analysis
Data analyses were performed using IBM SPSS Statistics Version 27. Spearman’s correlation test was used to identify correlations between psychological well-being, the effectiveness of e-learning and participants’ concerns over COVID-19. We used ordinal logistic regression analyses to examine the predictive factors of categorical dependent variables such as anxiety (GAD-7), depression (PHQ-9), somatic symptom (PHQ-15) and stress (PSS-10) levels. A P-value of <0.05 was considered statistically significant. A two-sided P-value was used for statistical significance.
Ethics approval
The study was approved by the NUMed Research Ethics Committee and the Newcastle Institutional Review Board (Ref: 13518/2020).
RESULTS
Of the 725 overall student population who received the invitation to participate in the survey, a total of 285 students responded to the self-administered questionnaire, thus giving a response rate of approximately 40%.
The demographics of the responses are shown in Table 1. Among 285 participants, 71.6% were females, more than half (54.0%) were Chinese, and the majority (80.4%) consisted of Malaysians. One-third of the students (33.3%) lived away from their hometowns, with a majority (90.5%) of respondents living with family or friends. Most students (84.9%) did not report any medical illnesses, while only 15.1% reported physical, psychological, or learning disabilities. At the time of the study, more than half (60%) of the students had received at least one dose of the COVID-19 vaccine.
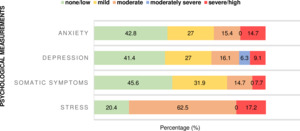
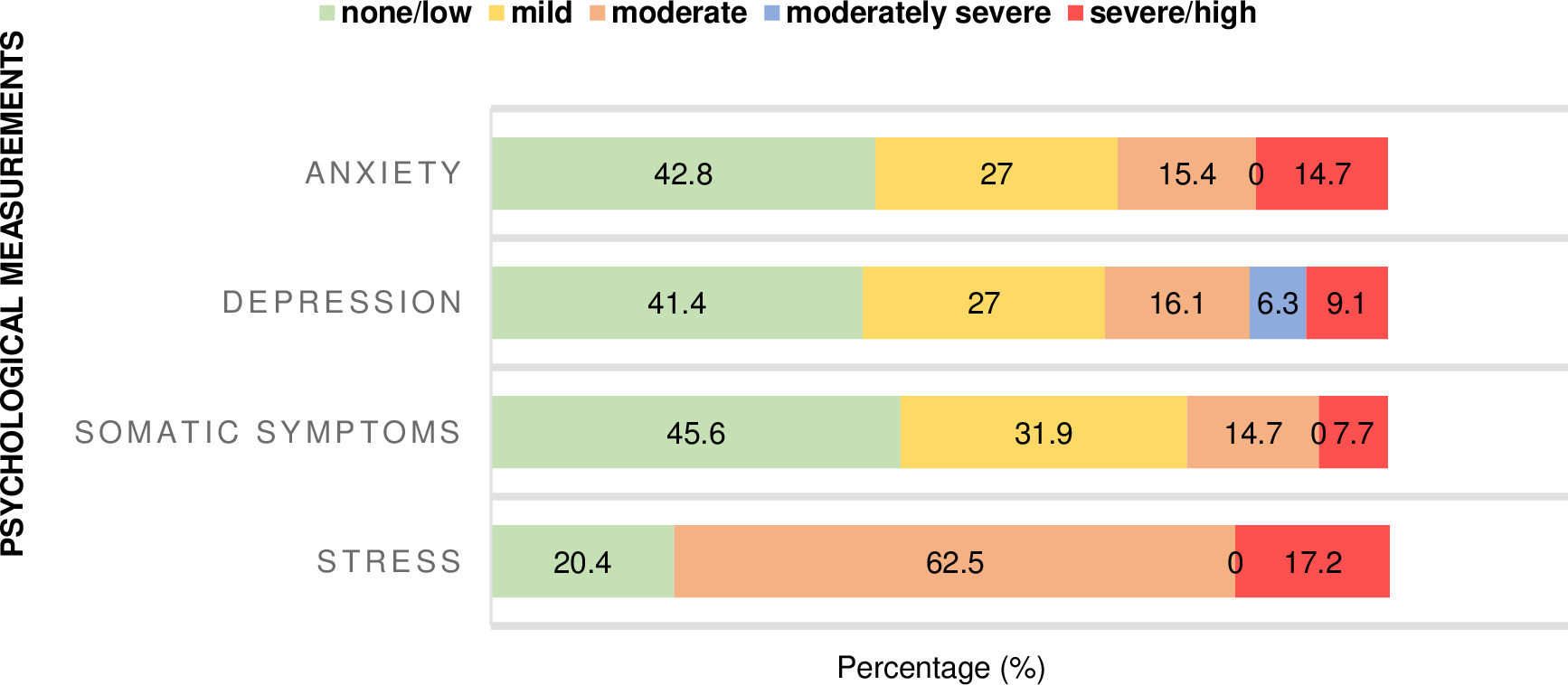
Our study showed that more than half the students presented with anxiety (57.2%). Among the 285 students, 77 (27.0%), 44 (15.4%), 42 (14.7%) reported having mild, moderate, and severe levels of anxiety, respectively. Only 122 (42.8%) of the participants had not reported anxiety. Depression was seen in 167 (58.6%) students with 77 (27.0%), 46 (16.1%), 18 (6.3%), 26 (9.1%) having mild, moderate, moderately severe, and severe symptoms, respectively. Meanwhile, 118 (41.4%) students reported no signs or symptoms of depression. More than half of students (155, 54.4%) reported having somatic symptoms, with 91 (31.9%), 42 (14.7%), and 22 (7.7%) students experiencing moderate, medium, or severe somatic symptoms, respectively. To maintain consistency with the other mental health scales, minimal somatic symptom levels were considered ‘none’ for 130 (45.6%) responders. The stress level was high among students, with the majority (227, 79.7%) experiencing moderate to high-stress levels during the pandemic. Students reported low, moderate and high-stress levels with 58 (20.4%), 178 (62.5%) and 49 (17.2%), respectively (Figure 1).
Female students had higher anxiety (P<0.039), somatic symptoms (P<0.002), and stress (P<0.016) levels compared to their male counterparts, as shown in Table 2. Students who lived alone were more anxious (P<0.043) and showed more somatic symptoms (P<0.033) than those living with their family and friends during the pandemic. Students with medical illness demonstrated greater psychological distress with higher levels of anxiety (P<0.002), depression (P<0.001), somatic symptoms (P<0.001) and stress (P<0.001) compared to those who did not.
Only medical students were asked about their clinical teaching experience, and the results are presented in Table 3. Medical students who found online role-play sessions unhelpful had increased anxiety levels (rho=-0.18, P=0.005). However, somatic symptoms were reduced among medical students who found campus role players helpful (rho=0.16, P=0.012).
The most concerning issues perceived by students during the COVID-19 pandemic were the disruption to the ongoing clinical teaching and research activities, followed by worries about their future careers being negatively affected due to the COVID-19 pandemic. There were also concerns about the shift towards online education and contracting COVID-19, as presented in Table 4. Anxiety (rho=0.19, P<0.001), depression (rho=0.13, P<0.001), and somatic symptoms (rho=0.17, P<0.005) levels were high among the students who felt their future careers might be negatively affected due to the COVID-19 pandemic. Somatic symptoms (rho=0.16, P<0.007) were experienced by students concerned over the disruption to their ongoing clinical teaching or research activities during the pandemic. Depression (rho=0.16, P<0.006) was also reported by students concerned about the education’s shift towards the online setting.
Table 5 shows that more than half (55.8%) of participants felt that the university supported them during the COVID-19 pandemic. The most sought-after mode of support during the pandemic was clear information and prompt update from the university (91.6%), followed by financial aid (73%), mental health resources (55.4%) and healthcare support (51.9%). The psychologically distressed students with anxiety (OR=2.47, 95% CI 1.49-4.08, P<0.001), depression (OR=3.22, 95% CI 1.94-5.34, P<0.001), somatic symptoms (OR=2.94, 95% CI 1.76-4.91, P<0.001), and stress level (OR=3.08, 95% CI 1.75-5.40, P<0.001) expressed that the university could provide support in terms of mental health resources during the pandemic.
DISCUSSION
This study, conducted amongst NUMed students, illustrated the effects of online learning on students’ mental health. Our findings showed that most of our students experienced some levels of psychological distress, such as anxiety, depression, somatic symptoms and stress during the COVID-19 pandemic, which is consistent with other studies recently conducted in different regions of the world.9 A study in Australia found that two-thirds of their students had reported moderate levels of psychological distress with consequently poorer mental health since the start of the pandemic.10 In comparison to an earlier study conducted among NUMed students in 2020, our data collected a year later showed that anxiety levels have risen to 57.2% from the previously reported 42%.11 This could be explained by the disruptions our current students experienced over nearly two years, where hospital teachings and campus sessions had been suspended, medical electives cancelled, and most teachings had migrated online. The extension of the course duration aimed at replacing insufficient clinical contact hours had also caused a delay in our final year students’ graduations, affecting career progression, which could have contributed to the increased anxiety levels among our students.
Female students reported higher anxiety, somatic symptoms and stress levels than their male counterparts. This trend was seen globally10,12,13 where the female gender generally has higher rates of psychological distress and was known to have different ways of expressing emotions and coping mechanisms compared to males.13 In contrast, a study in China showed no gender differences where both genders whereby equally affected by the pandemic.5 Students who lived alone were more anxious and showed more somatic symptoms of depression than those who lived with their family and friends during the pandemic. The possible reason for this could be due to the lack of support received by those staying alone during these difficult times.13 These findings were also consistent with a study from Kazakhstan.6 A study in China reported a double risk of depression among healthcare workers who lived alone and less anxiety among those who lived with parents or relatives.5 Moreover, our study also showed that students with medical illnesses demonstrate greater psychological distress with higher levels of anxiety, depression, somatic symptoms, and stress than healthy students. It has been established that there is a much higher risk of depression, potentially two- to three-fold, with essentially any medical illness compared to healthy individuals.14 Hare et al. also published data showing that psychological distress is linked to underlying medical illness, reporting the massive implications on their functions, hence this should not be neglected.15
Role players have long been an integral part of medical education, but unfortunately, little research has been done on their effectiveness. During this pandemic, our study has highlighted the importance of and reliance on role players in the continuation of medical education. Anxiety level has increased in medical students who found online teaching sessions involving role-player interaction challenging. However, somatic symptoms were reduced among medical students who found campus role-player sessions helpful. In a case study conducted in the United Kingdom, Nestel et al. established that medical students found role players helpful in communication skills as it allowed students to practice non-verbal communication in a doctor-patient consultation.16 However, students responded that role-play sessions were often unrealistic and the instructions provided were unclear. Students were also sceptical about whether the role players could adequately prepare them for real patient assessments once they joined the workforce. It was also previously identified that role players should be adequately prepared before the session to produce better outcomes.16
Students who felt that disrupting the ongoing clinical teaching and research activities was the most concerning issue during the COVID-19 pandemic experienced some somatic symptoms. The mandatory closure of universities, laboratories and suspension of hospital sessions for extended periods during the pandemic has had detrimental effects on education resulting in students’ poor mental well-being. A study in the African continent reported that students who could continue their education amidst the pandemic saw reduced hours in the laboratory, faced difficulty meeting research fund deadlines, and experienced less informative teaching rounds with less patient contact due to widespread fear of COVID-19. The social distancing regulations have greatly impacted medical teaching and the availability of placements, exacerbating the students’ stress levels.17
The most sought-after support from the university during the pandemic was in the form of clear information and prompt updates. Sundarasen et al. have previously shown that uncertainty on exams, completion of semesters and graduations had great repercussions on students’ anxiety levels.13 To combat the uncertainty, medical schools and the Medical Students’ Society in Australia have taken proactive measures to provide constant communications and updates to alleviate students’ worries.10 Furthermore, psychologically distressed students would have welcomed better mental health support from the university during this pandemic. Although NUMed has a support system with on-site counsellors, and every student has regularly scheduled meetings with their educational mentors, most still find it lacking. Many reasons could contribute to the dissatisfaction - the stigma surrounding mental health, personal struggles to confide in others, accessibility for students living off campus and international students who may face a language barrier. A study in China has suggested that students should be introduced to specific portals and sites that will be most helpful in supporting their mental health and that the university could launch online platforms to allow students to communicate with each other, while lecturers should be more attentive to students’ mental well-being.5 Another university had piloted innovative methods, such as organizing mental health education livestream events on social media, to disseminate relevant information to improve students’ understanding of mental health and promote better help-seeking behaviours.18,19
Limitations
Our sample size in this study was small, with 285 participants and involved mostly medical science students from only one study site. It also did not consider the perspective of educators. Ideally, psychological well-being should be investigated across different periods to understand the pandemic’s true implications better. However, with the voluntary nature of the study’s recruitment strategy, it will be challenging to conduct a follow-up study. Lastly, reporting bias may be an issue due to the self-reporting nature of the survey as students might choose not to reveal their struggles and mental health conditions.
CONCLUSIONS
This study demonstrated further insight into the psychological well-being of students from a medical college in Malaysia one year into the pandemic. It had shown that students faced difficulties coping with the transition to e-learning, and many of them experienced anxiety, depression, somatic symptoms, and stress during the pandemic. This study identified a few contributing factors to their psychological well-being. Medical students preferred campus role-play sessions over online role-play sessions as they provided a better opportunity for students to replicate real-life consultations. The types of university support, such as clear information and prompt updates from the university, were highly desirable by students as they wanted more certainty in their education and future careers, which many feared would be negatively affected by the pandemic. Psychologically distressed students would also value more mental health resources to help them cope with the pandemic. Therefore, universities should focus on collecting students’ feedback on multiple aspects of their well-being to optimize their educational experience and in readiness to respond to any future pandemic.
Acknowledgements
None.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Authorship contributions
SK and EO contributed to conception of the study. SK, SC and JY contributed to its design, methodology, data acquisition, formal analysis, data interpretation and writing the original manuscript. EO contributed to design, methodology, data acquisition, data interpretation and supervision. All authors contributed to manuscript revision, have read, and approved the submitted version.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Dr Edmund LC Ong, MBBS, MSC, FRCP, FRCPI, DTMH
Newcastle University Medicine Malaysia (NUMed Malaysia)
1, Jalan Sarjana 1, Educity, 79200 Iskandar Puteri, Johor, Malaysia.
Email address: [email protected]