Traditionally, oral health has not figured prominently in national healthcare frameworks of low- and middle-income countries (LMICs). The WHO Oral Health Resolution has addressed this challenge head-on and ratified it at the 2021 World Health Assembly.1 The resolution echoes what key international health organizations, such as the International Dental Federation (FDI) and World Health Organisation (WHO), have been emphasizing for many years, that context-relevant policies and research to determine needs and monitor progress are key components in efforts to eradicate oral health inequalities.2,3
Africa is a region with severely compromised oral health service delivery.4 Oral health inequities are acute in many parts of Africa, with wide disparities in access to quality care between urban and rural areas.3,5 In most LMICs, policymakers have not prioritized oral health, underestimating the burden of oral and maxillofacial problems, their connection with systemic health and possible threat to human life, resulting in little focus on dental public health programs.6
The burden of oral diseases in LMICs is also increasing because of rapidly growing populations, rapid westernization of diet, and lack of resources.6 Dental diseases can severely impact the day-to-day activities of an individual. This can include being unable to work effectively because of dental pain, which can have profound economic implications for both individuals and national prosperity.4
The WHO (2020) proposes effective and sustainable oral health solutions in Africa, including primary healthcare, information surveillance and developing policies that tackle priority oral health conditions.7 If progress is to be made in addressing these challenges in oral health, governments need to develop appropriate national oral health policies and to provide resources to support policy implementation.8 This paper focuses on the work of one country, Malawi, to follow the direction of travel outlined by the WHO.
In 2018, the Scottish Government agreed on funding for a joint project between the University of Malawi College of Medicine (now Kamuzu University of Health Sciences) and the University of Glasgow to establish the first Bachelor of Dental Surgery (BDS) course in Malawi and to work with the Ministry of Health and other key stakeholders to create a National Oral Health Policy.9 The BDS course was launched in 2019, and following a workshop in Lilongwe in February 2020, a multi-stakeholder Oral Health Policy Taskforce was set up to develop the policy over the next two years. This international partnership presented an opportunity for an in-depth examination of oral health policy development in the African context with the unique involvement of a country (Scotland) that had a successful track record in oral health research and policy development at a global level.
This study, utilizing a case study approach, aimed to report on the processes followed to develop a National Oral Health Policy. The research questions to be answered were:
How is Oral Health Policy being developed within an African context?
Specific Questions:
-
How is oral health policy being developed in Malawi?
-
Who contributes to developing oral health policy in Malawi, and what is their contribution?
METHODS
A case study approach was adopted. The study was qualitative. Semi-structured interviews were chosen as the method of data collection. This allowed the researcher to prepare questions ahead of the interviews and allowed the interviewee to elaborate on and explain issues through open-ended questions. The researcher took the ontological position of interpretivism to accommodate inductive and deductive approaches.10
Ethical issues
Ethical Approval was obtained from the University of Glasgow College of Social Sciences Ethics Committee (Reference Number: PGT/SPS/2021/018/GLOB). Permission was also sought from the University of Malawi College of Medicine Research and Ethics Committee to conduct the study and an ethical waiver was obtained (Reference Number: P.05/21/3313).
Informed verbal consent was obtained from respondents prior to interviews. The Participant Information Sheet indicated that it might be impossible to keep participants’ identities confidential due to the specificity of the study. This was mitigated by giving participants their transcripts to read before analysis to identify areas where they would not want to be directly quoted. No participant requested to have any information changed or removed
Recruitment
The target population comprised 21 health policy actors in the Malawi National Oral Health Policy Taskforce, representing the Malawi Ministry of Health and other key stakeholders, all participating in the policy development process.11 A key informant administering the MalDent Project provided a list of the task force members. From this list, ten health policy actors were identified through purposive sampling. Following Etiaba et al. (2015) and Mozhdehifard et al. (2019), the first author selected participants to incorporate experts in the following categories: international development partners, academics, policy experts, dental practitioners, and civil society organizations.12,13
The researcher introduced the study to the identified task force members via an e-mail, which included the Participant Information Sheet and Consent Form. A total of 12 task force members were approached, of which ten responded. Of these ten respondents, eight indicated a willingness to participate in the study and identified a suitable date and time for the interview. Two respondents were unwilling to participate because they had been part of the task force but had not participated extensively in the policy development process.
Data collection
In light of travel restrictions imposed by the COVID-19 pandemic, the interviews were conducted remotely on Zoom. During the interview, some participants switched off video cameras to improve internet connectivity.
The five themes informed the semi-structured interview guide of ‘Policy Analysis Models in Oral Health Issues’ described by Mozhdehifard et al. (2019)13:
-
The role of stakeholders in oral health policy-making
-
Assessment of the oral health system
-
Oral health policy development
-
The process of oral health policy-making
-
Oral health policy learning and capacity building
The interview guide (online supplementary document) was pre-tested in May 2021 by administering it to an oral health professional with experience at the Ministry of Health, who assessed it for content, logical flow, and contextual relevance. No restructuring was required based on feedback from the pre-test.
The researcher obtained verbal consent for all interviews and audio-recorded them. The interviews were approximately one hour (ranging from 43 minutes to 75 minutes) and took place remotely via Zoom from May-July 2021.
Data analysis
Recordings were transcribed verbatim. A thematic analytic approach was taken.14 Data were read and re-read and then initially coded using an inductive approach, allowing themes to emerge naturally from the content of the interviews. Those codes were later grouped into broader categories based on similarity and then into themes organized according to the five themes of ‘Policy Analysis Models in Oral Health Issues’.13 They were further merged into Walt and Gilson’s (1994) Policy Triangle Framework (actors, content, context, processes) and subsequently into key themes of the two research questions, ‘who’ and ‘how’.15
FINDINGS
The eight respondents represented the organizations indicated in Table 1. Not all task force members that were appointed played an active role in the policy development work, as indicated by an international development partner below:
‘‘We have a task force of about 15 or 16 people, most of the meetings it is only about seven are present and there are some who never came to a meeting….It happens in this country [the United Kingdom] as well.’’ - Respondent 1, International Development Partner
The study findings described below will be presented in the order of who contributed, the processes undertaken, and the challenges encountered during developing Malawi’s National Oral Health Policy.
Who is contributing to developing oral health policy in Malawi?
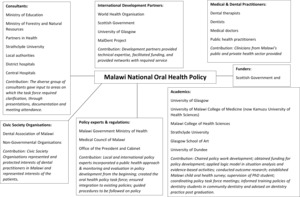
Figure 1 shows the stakeholders that the interview respondents collectively identified as having contributed in some way to the National Oral Health Policy development process. Table 2 captures the stakeholders as individual entities and their contributions to policy development.
It is clear from the data in Figure 1 and Table 2 that a diversity of stakeholders contributed a wide skill set to developing Malawi’s National Oral Health Policy. Academics initiated the policy development process at the University of Malawi College of Medicine (now Kamuzu University of Health Sciences) and the University of Glasgow. The involvement of these academics enabled funding to be sourced from the Scottish Government and key technical expertise to be drawn into the process. Compared to many African countries, this provided Malawi with the distinct advantage of the involvement of local and international multidisciplinary experts and their networks.16 Development partners were instrumental drivers in providing specific content and detail due to their technical expertise and experience. Scottish development partners were valuable in aligning the policy to the oral health discipline from their experience in similar projects, whilst World Health Organisation representation made it regionally and globally contextually relevant by utilizing the African Region’s Oral Health Strategy and World Health Assembly Oral Health Resolution respectively.17,18
Multidisciplinary skills
Some representatives of the task force were multidisciplinary and were involved as actors in varying categories, exemplified by one International Development Partner who stated their contribution:
‘‘It was in two capacities; it was both in my academic role but also I am an NHS consultant in Dental Public Health.’’ - Respondent 5, International Development Partner, Dental Public Health Expert
This individual contributed as an experienced academic, a dental public health consultant and an oral health policy expert. This is different from scenarios in many other African countries that have undergone this process, where individual contributors do not have such a multidisciplinary background relevant to the discipline of oral health.3 This diversity in the skillset of a relatively small number of individuals actively involved in the task force enabled progress, despite the challenge of a limited oral health workforce in Malawi, delicate political manoeuvring and the controversial past of the oral health system’s governance and leadership. This approach supports the proposal by the World Health Assembly (2021) for oral health policy development requiring a multidisciplinary approach.18
The stakeholders that played a role in shaping the oral health policy were categorized according to the roles they played: policy experts, health practitioners, dental practitioners, academics, international development partners, and Civil Society Organisations.12,13,15,19 What is unusual about the Malawi actors is that other categories emerged which are not included in the above list. This is exemplified by the category of consultancies, where several organizations were consulted, such as the Ministry of Forestry and Natural Resources and Strathclyde University on water and fluoride content, the Ministry of Education on child oral health and the NGO Partners in Health regarding the incorporation of oral health into the broader Non-Communicable Disease agenda in Malawi.
Fortunately, the support from the Scottish Government funded MalDent Project, Malawian and Scottish academics, together with their networks, has helped the Ministry of Health to continue the policy development despite previous distractions such as the COVID-19 pandemic.
Networks
The development of Malawi’s Oral Health Policy has been strongly supported by the extensive networks of the actively involved task force members, which have helped to foster technical expertise and extract resources. Without these networks, the policy development process would have been very challenging. Several studies have shown that resource limitations and low numbers of experienced dental public health experts and academics have inhibited oral health policy development in the African region.20,21 Malawi has shown that outsourcing expertise is an option that can reduce gaps in capacity within oral health systems. COVID-19 showed us that video and internet access could enable actors to connect more efficiently and effectively than before. Such technological advancements have enabled progression through contributions from actors in different parts of the world.22
In the case of the MalDent Project, the interaction between the Ministry of Health, local stakeholders, and international development partners have been coherent and cohesive. Josefczyk (2015) stated that power dynamics in countries undergoing political transitions could be a hindrance to policy development.23 Contrary to this, changes in Malawi’s political leadership that occurred in 2020 during the policy development process resulted in new leaders in the Ministry of Health responsible for oral health. In their role of regulating the policy development process, they have been keen to develop the oral health sector and work with the pre-existing health team members. The power dynamics have been well managed based on the participants’ perspective and the research team’s interpretation of their experiences.
‘’ It has been very good, it’s been extremely good. First they [Ministry of Health] supported the establishment of the dental program, they’ve supported the MalDent program because there’s no way you can do that without Ministry, without Government, knowing so. And they also supported the health policy to have a component of oral health, so the next thing. And they’re the ones who identified that the absence of a policy was a major constraint in developing oral health services at a community level and the difficult-to-reach areas and things like that. So they are aware, and the key people are the curative and preventive section with the ministry so at the moment they’re the ones who are saying let’s have this done so, there has been no conflict, no push and pull, it’s all been very cohesive arrangement and discussion.‘’ - Participant 3, University of Malawi College of Medicine (now KUHeS), MalDent Project Coordinator
‘‘Malawi have a stronger stakeholder environment and very strong leadership, I did not see much difficulty because of that support to develop the Oral Health Policy compared with other countries that don’t have funding, that don’t have a supporter, then from scratch, we need to support.’’ - Participant 4, International Development Partner
Regardless of the funding coming from external sources, boundaries were described as established at the outset, and political considerations have been accommodated, recognizing that leadership and oversight of health policy development sits with the Ministry of Health.11,13 The World Health Organisation’s role is very important in providing a suggested direction of travel for oral health policy in the region. However, it had limited capacity to provide hands-on assistance to the task force as it has a small oral health staff complementing only two members, one in Geneva and one in Africa. Nevertheless, Malawi’s Oral Health Policy followed the precepts of the WHO strategy for Africa very closely.
How is oral health policy being developed in Malawi?
Based on the discussions during the interviews, Tables 3, 4 and 5 succinctly present a large amount of information that emerged as themes relating to how the policy was developed. These themes were organized according to those suggested by Mozhdehifard et al (2019) in their paper ‘Policy Analysis Models in Oral Health Issues’.13 The question ‘how’ was answered by responses to three of these themes: the assessment of Malawi’s oral health system, the areas to be addressed by the oral health policy development, and the process to be followed in oral health policy development. Table 3 outlines the state of Malawi’s oral health system, which informs the areas of interest the policy had to address in the thematic areas outlined in Table 4. Table 5 is the mechanism for oral health policy creation that had to be followed. These themes from the different respondents were then connected to create the outline in Figure 2 and a step-by-step section on the policy’s creation.
Table 3 illustrates that Malawi’s oral health system needed the new policy to address the following key issues: a massive oral disease burden unmet at a population level, a small and overwhelmed oral health workforce, limited representation of the oral health discipline in leadership roles; insufficient and urban-skewed oral health service provision; inadequate oral health data and information for decision making; and finally the apportionment of limited resources for oral health service provision.
The sequential steps taken since February 2020 for the Malawi oral health policy development process were further organized into the flowchart in Figure 2 from the accounts of the participants and emerging themes indicated in Table 3. The elements and sequence of the process are similar to those used by other countries, such as Nigeria, when they developed their policies.12 The Ministry of Health provided the formal policy development procedure, as the Malawi Government dictated. The synchronized guidance of the Ministry of Health and development partners that was followed is similar to the steps suggested by Easton’s (1965) iterative policy development process and the oral health policy development process synthesized from the accounts of Etiaba et al. (2015) and Mozhdeharfard et al. (2019).12,13,24 The two studies outlined that oral health policy is developed through agenda setting, problem identification, situation analysis, policy formulation, policy approval, policy implementation, and policy evaluation. The results present each of these steps. The groups of actors influenced the specific steps of the development that were aligned with their expertise.
Step 1: Establish multisectoral working group
The Malawi Government Ministry of Health led the first two steps of establishing a multi-stakeholder task force and drafting a concept paper.
'‘The thing that was very clear from an early stage is that the Ministry had to be seen as the organization that was leading the policy development.’’ - Participant 1, International Development Partner
The Malawi National Oral Health Policy task force was established to conduct the policy development.
‘‘Through cohesive arrangement and discussion MOH [Ministry of Health] are the entity that is saying ‘let’s have this done’.’’ - Participant 3, University of Malawi College of Medicine (now KUHeS), MalDent Project Coordinator
Step 2: Concept Paper
International development partners consolidated the Concept Paper and drove the drafting of the Narrative Review. Their prior experience participating in Scotland’s oral health policy development, academic contributions to global oral health, and experience in oral health collaborations proved beneficial. One challenge encountered was a deficiency of published material on Malawi’s oral health system, but regional data and information from other developing countries were useful in mapping the direction. This showed the significance of having a World Health Organisation representative who provided technical expertise.
‘‘The Concept Paper, I should say, was largely written by a member of the Planning Department within the Ministry of Health, who had attended the national oral health policy meeting in February 2020. And he took that on board and did the first draft of the concept paper which the Dental Public Health expert and I then worked on afterwards.’’ - Participant 1, International Development Partner
Respondent 5 (International Development Partner, Dental Public Health Expert) further clarified that the Concept Paper;
‘’… was designed to understand terms of reference of the national oral health policy development. It comprehensively clarified what the policy was intended to achieve through establishing challenges, inputs, outputs and outcomes.‘’
Step 3: Narrative Review
A review of what was happening in oral health within Malawi, Africa and globally was conducted. The review was based on an initial literature search, including PubMed and Google Scholar. According to Respondents 4 and 5, who were both International Partners, the reviewed content included national resolutions and published peer-reviewed papers. For example, Malawi’s Health Sector Strategic Plan 2, the WHO Regional Oral Health Strategy Africa (2016-2025), the publication Addressing Oral Diseases as Part of Noncommunicable Diseases, Promoting Oral Health in Africa, the World Health Assembly Oral Health Resolution, broader World Health Organisation resolutions, and The Lancet Commission on Global Oral Health reports were all consulted.
Step 4: Situation analysis
Dental practitioners in Malawi were the drivers providing data for the situational analysis. Their familiarity and experience of practising in the field and knowledge of the Malawian context were required for this stage.
‘‘We looked at demographics, the burden of disease, oral health workforce, oral health care activities, data on risk factors for oral diseases, other existing policies relating to oral health such as NCDs, alcohol, sugar consumption, tobacco, as a measure of what the policy had to address;……seven Policy thematic areas were to be covered in the oral health policy: dental public health; clinical practice; human resources; infrastructure and equipment; evidence-based research, data collection and information management; governance and leadership; finance.’’ Participant 3, University of Malawi College of Medicine (now KUHeS), MalDent Project Coordinator
This exercise exposed a weakness of poor data and information management. This alerted the local stakeholders, including policy regulators, to the exclusion of oral health in the health system’s District Health and Information Surveillance System, which had been revamped some years earlier. The exclusion was attributed to a lack of leadership representing dentistry and oral health when the Ministry of Health conducted the exercise.
Step 5: Developing oral health policy
The macro and micro policies were then developed from the information gathered in the preceding stages. The dental public health expert emphasized the inclusion of oral health prevention surveys and programs, how to collect useful, relevant data and systematically manage the information. They also stated that:
‘‘I think the WHO has done a lot of work on that, and there are documents on that for guidance, so there is no need to reinvent the wheel, let’s use what is there already. It is good to see the resolution with WHO for oral health, I try to incorporate it in what I do. Again, with Universal [Health] Coverage, it’s good to understand what it means for each country.’’ - Participant 5, International Development Partner, Dental Public Health Expert.
A Ministry of Health policy expert (Participant 8) highlighted that he had helped the task force members distinguish between the detail that goes into a policy document and that to be put in a strategic implementation plan. Many task force members were putting bulk detail into the policy, unaware that the policy needed to be lighter. Task force members were initially concerned that key information was being stripped out but realized it had already been included in the way that it should appear in a policy document.
Step 6: Consultation
At the time of the interviews, the oral health policy development process was still ongoing. It was at the consultation stage, and from the task force, perspective linkage with key result areas had been achieved. The Ministry of Health was leading the consultation phase.
‘‘So we’re moving away from the theoretical part of it and now working into a realistic way of how best we can do this…so it aligns to all other policies that we have in the Ministry of Health.’’ - Participant 8, Ministry of Health Policy expert
Unfortunately, public consultations could not be held due to the COVID-19 pandemic
''One of the things we didn’t do because of time and which we really should have done, and at some point, probably should do is take soundings from ordinary people in the villages and in the cities about their experience of getting access to dental care. And with COVID and the fact that the Ministry was very keen to keep this project moving, we decided that we would be very open about the fact we hadn’t done that.‘’ - Participant 1, International Development Partner
Step 7: Implementation
The implementation stage of the policy was said to involve launching the policy document, disseminating it and ensuring the application of the contents. All respondents were concerned that implementation would not succeed without a Chief Dental Officer for Malawi. They agreed that financial support of the policy was also required beyond what had been previously available and that successful implementation required access to opinion formers in local communities, including villages. A Ministry of Health policy expert confirmed that this was no longer a concern because a national Oral Health Coordinator for oral health implementation and program oversight had been appointed after a 3-year lapse. However, the national Oral Health Coordinator appointed to the Ministry of Health still has clinical duties and is based at a Central Hospital in Northern Malawi rather than the Ministry of Health Headquarters in Lilongwe. The concern of the Ministry of Health policy expert was that a detailed implementation or detailed operational plan needed to be developed, which would help with driving oral health interventions. It should specify the individual or group of persons to activate the policy beyond their roles and responsibilities in the routine provision of oral health services in the Ministry of Health. It was further elaborated by a development partner who said:
‘‘Development of policy is often done by a Ministry of Health person whilst implementation happens at primary care level/community level…Not many oral health professionals need to think about training other health professionals. Task shifting primary care worker/community health worker is critical.’’ - Respondent 4, International Development Partner
Step 8: Monitoring and Evaluation (M&E)
Regarding monitoring and evaluation, there is a clear thrust for evidence creation through various oral health projects in varying stages of publication and current multiple research projects either in the planning stages or underway. In the initial stages of policy formulation (concept paper, narrative review, and situation analysis), there was a deficiency in Malawi’s oral health research on policy linkages. The low number of dentist-scientist workforce and the accompanying data surveillance challenge identified by Adeola et al. (2018) as prominent in African nations was shown to be present in Malawi.25 Some local Malawian oral health professionals involved in the policy development process expressed that they and their colleagues in the field were challenged in research competencies. This was the chief reason for the delays in providing information and the mismanagement of data and information experienced during policy development. The Ministry of Health proposal to manage the problem by focusing on standardizing and incorporating oral health indicators into the District Health Information Surveillance System is urgent. However, it should be easier than before due to the recently developed Health Sector Strategic Plan 2 (HSSP 2). The HSSP 2 has been an enabler for the oral health policy development process.
A development partner who is also a dental public health expert emphasized that to establish if the policy is working as intended, they are working on the monitoring and evaluation to be:
"…‘clear on research outputs, outcomes, surveys, involve quantitative and qualitative outputs for the population and stakeholders’ thoughts on how policy is working.‘’ - Participant 5, International Development Partner, Dental Public Health Expert
Step 9: Policy review
The National Oral Health Policy is intended to undergo review every five years. Several respondents highlighted that for this to occur, there is a need for the younger generation of oral health professionals to be developed to carry on the work. Respondents from the Dental Association of Malawi and the Ministry of Health Policy Department expressed commitment to appraise the younger generation in their transition from dental school to working in an internship. A way intended to equip these students is creating community dental health teams at their workstations whilst under the mentorship of the oral health leadership in the organizations mentioned above.
DISCUSSION
The policy development process was guided by Malawi’s Ministry of Health and a diverse group of actors, local and international, all of whom contributed. Challenges identified related to resource availability for implementation of the policy; funding and human resources for health; weak and difficult-to-access pre-existing supporting evidence of oral health research, information and data; poor and partially used in-country network of oral health professionals; and weak leadership and governance in Malawi’s oral health system. The funding of the policy development process by the Scottish Government and Borrow Foundation provided critical support and allowed a successful conclusion.
Several lessons can be learnt from this study. First, various documents relating to oral health policy in the African region provide valuable strategic guidance. Secondly, networks are an under-utilized resource in Africa, but despite being resource-constrained, Malawi has been able to develop a national oral health policy supported by a good network that external partners fully funded. Nationally, Malawi developed a Health Sector Strategic Plan 2 (HSSP 2) as policy documentation to map the direction of the health sector, and an analysis of the policy was conducted and published utilizing the similar Walt and Gilson Policy analysis model.15 This research builds on that, introducing the oral health policy dimension. This is key because, after the introduction of HSSP 2, oral health services were included into the essential package of basic health services but did not have a guiding national policy.
Malawi’s National Oral Health Policy was finally launched in April 2022, and efforts have turned to the implementation of the policy. Now that the Bachelor of Dental Surgery degree has been established in Malawi, students are being taught policy implementation as part of their curriculum. Furthermore, to measure the impact of implementation, it is important to develop quantitative oral health assessments and indices. To that end, a National Child Oral Health Survey is planned for 2023, which will provide the baseline epidemiological data against which the effects of a proposed child oral health improvement intervention can be measured. Similar exercises about other policy components will be required and detailed in the Implementation Plan that the Ministry of Health has published. The blueprint has been provided – it is now the responsibility of the relevant stakeholders to take forward the requisite actions and move towards improved oral health for all Malawians.
Acknowledgements
The authors would like to acknowledge the support of the Malawi Government Ministry of Health and thank all those participants who agreed to be interviewed.
Funding
CM was the recipient of a Beit Trust Scholarship.
The MalDent Project partnership between the University of Glasgow and Kamuzu University of Health Sciences is funded by a grant (MAL/18/04 – UoG) from the Scottish Government International Development Programme.
One member of the task force was funded by the Borrow Foundation.
Authorship contributions
CM: The conception and design of the work; the acquisition, analysis, and interpretation of data for the work
SC: Critically revised the work for important intellectual content
JB: Multiple interactions to discuss the establishment and management of the study. Critically revised the manuscript for important intellectual content
PC: Final approval of the version to be published; ensured accuracy or integrity of any part of the work was appropriately investigated and resolved
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Dr Cleopatra Matanhire, BDS , MBA , MSc Global Health
Department of Oral Health
Faculty of Medicine and Health Sciences
University of Zimbabwe
P.O Box A178
Avondale
Harare
Zimbabwe
E-mail: [email protected]