On March 11th of 2020, the World Health Organization (WHO) declared the novel ‘“coronavirus disease 2019”’ (COVID-19) a pandemic due to the distressing increase in its spread and severity world-wide.1 As of September of 2021, more than 200,000 individuals have been infected with COVID-19 disease in the State of Qatar.2
There is a fundamental gap in understanding the extent of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread in the community through asymptomatic individuals. Existing studies have established that transmission can occur during the asymptomatic period especially in family clusters.3–6 Early identification of patients unaware of the status of their disease is crucial to control the spread of the disease as they might unknowingly spread the infection to people around them.6
SARS-COV-2 screening and testing facilities face many challenges. One of them is how to achieve prompt testing of the population while minimising the risk of infection for health care workers considering the high infectivity and transmissibility of the SARS-CoV-2 virus itself.7–9 Although multiple Interventions have been established to identify infected persons and test them to contain the spread of the disease, most of the countries have prioritized testing of symptomatic patients.3 As the pandemic continues, more evidence supports the notion that asymptomatic spread is also an important driver of the epidemic.
Innovative screening models have been designed and implemented to optimise screening/testing capacity to face these challenges. These models include Drive-Through (DT) screening centres for people that have vehicles and Walk-Through (WT) screening centres for those who do not.10 The drive-through model was initially tested during the H1N1 Influenza outbreak in 200910,11 and Weiss E and colleagues, reported that the drive through testing models provided a social distancing strategy and were associated with rapid throughput times.10–12
COVID-19 drive through testing models have been implemented successfully in many countries around the world. South Korea pioneered the drive through testing, and they were able to test around ten people per hour which is double the capacity of their indoor clinics.13 In addition, drive though testing sites have been launched in the UAE, Saudi Arabia, and Bahrain.14–18
The State of Qatar have established stringent infection control measures for the COVID-19 to ensure safe and efficient testing system. It established extensive plans to identify, test and manage people with COVID-19 infection.19,20 Even though Qatar was testing many cases and covering a wide range of population groups, it was crucial to take tactical actions to expand community surveillance and active screening to reduce the potential risk of undetected community transmission.
In May of 2020, the Primary Health Care Corporation (PHCC) was commissioned by the Ministry of Public Health (MOPH) to establish COVID-19 drive through swabbing hubs.19,20 The primary health care corporation (PHCC) is the main provider of primary care in the State of Qatar. It provides health-related services through 27 local health centres distributed into three geographical regions, namely Central, Western , and Northern. At the beginning, the service targeted asymptomatic population and prioritised screening for groups with the following criteria: history of contact with COVID19 patients, older age group, or presence of underlying comorbidity.19,20 However, upon the relaxation of travel restrictions, around November of 2020, asymptomatic individuals who needed to obtain a ‘“fit to travel Covid-19 negative certificate”’19 to be able to travel outside Qatar were allowed to take RT-PCR test at drive through hubs.
It was initially established within three PHCC health centres namely Al-Thumama, Leabaib and Al-Waab health centres located in Central, Northern and Western regions, respectively, and was later expanded to include another nine health centres. Health centres operated drive through testing services within their respective car parks from 8am to 12am (16 hours) staffed by two 8 hours shifts (8am – 4pm; 4pm – 12am). People were invited to be tested at the health center they are registered at which is the nearest to their residence, Figure 1. All the testing of COVID-19 in Qatar was centralised and it was conducted at Hamad Medical Corporation’s (HMC) central laboratory. HMC is the main provider of secondary care in Qatar.20
METHODS
The aim of this study was to describe the outcomes of the COVID-19 RT-PCR tests among asymptomatic persons through estimating the COVID-19 point prevalence, calculating testing positivity rates, and Identifying risk factors associated with testing positive among asymptomatic people tested through the PHCC’s drive-through swabbing hubs.
The study was approved by the Institutional Review Board (IRB) of the Primary Health Care Corporation (PHCC) on 9/9/2020 with reference number PHCC/DCR/2020/07/075 and the requirement for informed consent was waived.
We have conducted a longitudinal retrospective identification of all adults ≥18 years of age who have not been previously diagnosed with SARS-CoV-2 infection or COVID-19 and were tested for SARS-CoV-2 through the PHCC’s drive-through swabbing hubs between June 1st , 2020 and May 31st of 2021. The testing data was extracted from the national SARS-CoV-2 PCR testing database. COVID-19 infections were confirmed through real-time reverse-transcription PCR (RT-qPCR) using the TaqPath COVID-19 Combo Kit (Termo Fisher Scientifc, USA). TaqPath™ COVID-19 Combo Kit. “Based on the melting temperature analysis, the TaqPath™ COVID-19 Combo Kit correctly identified (98.4%) of known SARS-CoV-2 strains/isolates in GISAID”21
Sociodemographic characteristics and pre-existing morbidities were extracted from the anonymised electronic medical records. Asymptomatic persons that self-reported recent contact as their reason for taking the test were excluded from the study. Our study defines asymptomatic carriers as people with positive RT-PCR tests but not showing any COVID-19 symptoms or signs at the screening point.
The outcome of interest was the testing outcome (testing positive vs testing negative)
Data analysis
Categorical variables were reported as frequencies and proportions. The difference between the persons who tested positive and those who tested negative in sociodemographic and clinical variables was evaluated using chi-squared test χ 2 and Fisher’s exact for categorical variables. Continuous variables were described using mean and standard deviation and differences were examined using paired sample t-test and one-way ANOVA as appropriate. The prevalence of SARS-CoV-2 infection was expressed as a point estimate with 95% confidence interval (CI) and was defined as the number of positive COVID-19 infections (identified by RT-PCR) over the total number of all people tested at the swabbing hubs.
Univariable analysis and multivariable binary logistic regression model were used to establish the difference in RT-PCR positivity outcome based on sociodemographic factors. We estimated Odds ratios (OR) and adjusted OR (aOR) with 95% confidence interval. All measured exposure variables (age, gender, nationality, place of test and comorbid conditions) were included in the model to control for potential confounding effect. We use a 1000 bootstrapping samples to estimate 95% confidence intervals. All statistical tests were two-tailed and a P value of < 0.05 was considered the cut-off level for statistical significance. All statistical data analysis was conducted using STATA/MP 15.1 (StataCorp LLC, College Station, TX, USA)
RESULTS
Between June 1st 2020, and May 31st 2021, a total of 148,735 subjects were tested for SARS-CoV-2. Testing sites conducted tests ranging from 1 to 2,293 tests per day with an average of 353 tests. Out of the cohort of tested people 31.2% (n=46,444) were in the age group (30-39), and the majority 73.6% (n= 109,514) were <50 years old. Ages ranged from 18 to 96 and mean age was 40.25 (standard deviation, SD=13.8) years. 53% (n=78,770) were males and 30.3% (n=45,016) were Qatari nationals. 63% (n=93,714) had no existing comorbidity, while 36.9% (n=55,621) reported having at least one chronic condition. 42.1% (n=62,663) were tested in the Western region of Qatar.
There were 5,848 positive subjects representing a point prevalence of 3.93 (95% confidence interval, CI=3.83-4.03). Overall, individuals who tested positive had a mean age of 38.51±11.6 with 83.2% (n=4,867) being in the age group of 18-40 years (Table 1).
Figure 2, shows the daily and monthly positivity trend in relation to Qatar’s government staged lifting of COVID-19 restrictions. The positivity rate increased steadily between June of 2020 and May of 2021 and it peaked in September of 2020 at 2.15 (95% CI=1.77-2.61) and started declining afterwards to increase again in February of 2021 and reached its highest in April of 2021 (16.97%). The rate also varied by nationality. The adjusted odds of positive RT-PCR were higher among Filipinos (adjusted odds ratio, aOR 2.61, 95% CI (2.39-2.86)) , Sri Lankans (aOR 2.54, 95% CI (2.21-3.04)), and Nepalese (aOR 2.03, 95% CI (1.68-2.45)). Qataris had the lowest positivity rate and adjusted odds of positivity with 2.8% being asymptomatic carriers (P<0.001). The RT-PCR test positivity rate was the highest among persons with no history of comorbid conditions 4.4 (95% CI=4.27-4.53) (Table 2).
Logistic regression analysis identified age, nationality, existence of chronic comorbidity, and testing centre geographical location to be significantly associated with a higher likelihood of asymptomatic infection, Table 3. There was no significant difference among groups based on gender. The most common comorbidities identified in persons who had a positive RT-PCR test for SARS-CoV-2 infection were hypertension (12.8%), diabetes (12.1%), dyslipidemia (11%), and obesity (7.5%).
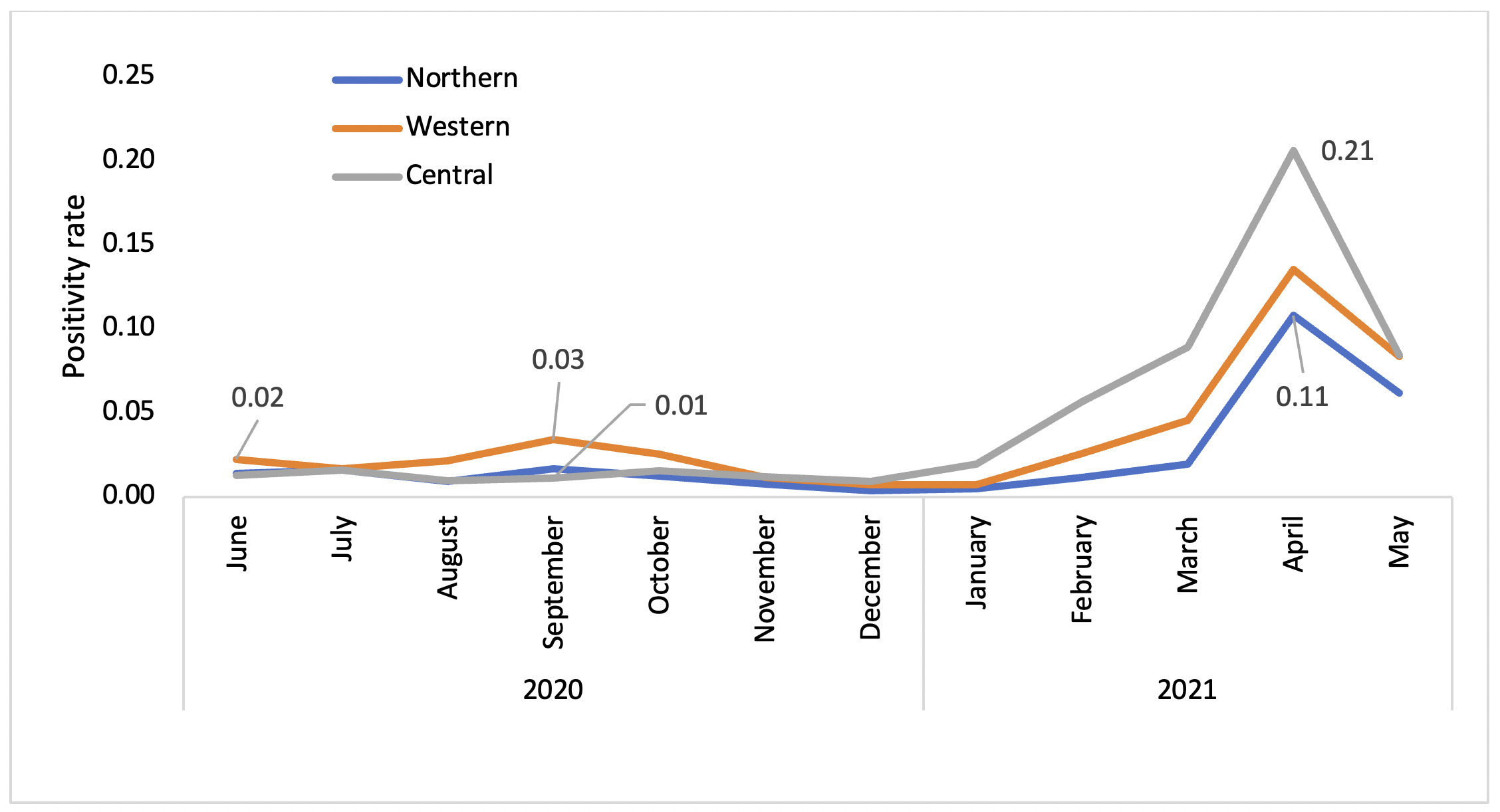
We observed geographic differences in numbers of SARS-CoV-2 positive cases as people were tested at the closest PHCC health centre to them in the Central, Northern, and Western regions of the PHCC. We noticed similar trends of infection in all regions. Yet, when compared to the Northern region, the prevalence RT-PCR positivity in the Central region was the highest at 6.01 (95% CI=5.82-6.21, P<0.001), followed by the Western region. People tested centrally were almost 4 times more likely to have a positive test (aOR=3.59, 95% CI=3.30-3.92, P<0.001) compared to those tested in the North. Figure 3 demonstrates the changes in the positivity rate of confirmed COVID-19 cases through time comparing the three geographical regions of PHCC.
DISCUSSION
The State of Qatar is a melting pot of many different cultures with 94 different nationalities and around 90% of its population being expatriates.22 Therefore, our study brings new insights into the COVID-19 pandemic in a unique sociodemographic background. There is limited data to inform the prevalence of infection among asymptomatic cases in Qatar as testing was heavily focused around symptomatic individuals or those with high risk-profile.23 The PHCC was successful in quickly setting up and implementing active testing of asymptomatic persons through drive-through testing hubs. The presented findings described asymptomatic cases according to their RT-PCR testing outcomes.
The process contributed to the detection of 5,484 asymptomatic COVID-19 cases between June of 2020 and May of 2021 corresponding to a point prevalence of 3.99%. Our findings are similar to the results of the ACORN study as they reported a prevalence of 3.1% among asymptomatic participants.23 A study in South Korea reported a 2.64% positivity rate among asymptomatic participants during the early months of the epidemic.24 In addition, globally the estimated percentage of asymptomatic individuals that contracted SARS-CoV-2 ranged between 1.2% to 12.9%.9
In Qatar, a PCR community survey was conducted, and it showed that around 58.5% of participants who had a positive RT-PCR SARS-CoV-2 test reported experiencing no symptoms.24 Higher levels of COVID-19 asymptomatic infections are expected in Qatar due to the availability of testing and active screening, not to mention that Qatar’s population has a younger age profile with less than 10% of the population being older than 50 years old.25,26 Mathematical modeling of the SARSCoV-2 epidemic in Qatar demonstrated that nine out of each ten COVID-19 infections were never diagnosed . All of this suggests that the pandemic in Qatar is uniquely driven by undetected asymptomatic or pre-symptomatic cases.27
One of the unique findings in our study is that it describes the epidemiology of COVID-19 based on geographical trends and regional differences. The time trend shows an increased prevalence of asymptomatic cases in all regions of Qatar towards the end of 2020 aligning with the start of the 4th phase of the controlled lifting of COVID-19 restrictions.28,29 These trends can reflect the surge of COVID cases in the community as Qatar entered its second wave of the infection. In addition, there was an expansion of the testing with more people being tested in 2021.
There was a clear regional difference in the prevalence of cases in the Central, Western and Northern regions. At the beginning of the pandemic infection trend was higher in the Western region. This can be explained by the fact that the first clusters of COVID-19 case in Qatar were among single male workers heavily residing the Western region of Qatar.25,29 Abu-Raddad et al. reported similar findings when they assessed PCR positivity in community surveys in May of 2020. They reported 17.5% SARS-CoV-2 positive cases in Al Waab health, 17.1% in Al-Thumama, and 6.5% in Leabaib health centres located in the Western, Central and Northern regions, respectively.25 As the pandemic progressed, we can see a change in the pattern with more people contracting the infection in the Central region. The biggest cities in Qatar, namely Doha and Al Wakra, are located in the Central region and around 39.25% of PHCC’s patients are residents of that region.30 Understanding the geographical trends will be crucial for anticipating the possible course of the pandemic and the potential for the virus resurgence in relation to easing of physical and social restrictions.
The study reinforces our understanding of the relationship between population demographics, especially age and existing comorbidities with the burden of COVID-19 disease. Our findings show a lower risk of positive SARS-CoV-2 PCR test among older people when compared to the younger, and among those with two or more chronic conditions. Anand et al. reported a similar observation it was attributed to the higher competing risk of severe symptomatic COVID-19, hospitalisations or even mortality after exposure to SARS-CoV-2 infection among older individuals.31 This could also explain the lower likelihood of positive test, noted in the study, among those with two or more chronic conditions. Hypertension, diabetes mellitus, dyslipidemia, and obesity were the most frequent chronic comorbidities reported among those who had a positive COVID-19 test. This is important as chronic comorbidities, particularly hypertension, are predictive factors for developing symptoms, severe COVID disease and death in individuals who were initially asymptomatic carriers.32
Finally, around 60% of Qatar’s population consists of manual workers33 working on construction projects predominantly males from South Asian nationalities (25). These workers typically live in large accommodations with shared rooms and bathrooms.25,34 This can explain the variability of the positivity proportions based on nationality which reflects the socioeconomic and employment structure in Qatar.34
STRENGTHS AND LIMITATIONS
There are limited studies in Qatar that investigated COVID-19 prevalence among asymptomatic persons especially at the primary care level. In addition to estimating the differences in SARS-CoV-2 prevalence by demographic characteristics and geographical region, our study provide evidence supporting the use of community surveillance of asymptomatic persons as a viable tool to track the changes in the disease in the community.
However, there are major limitations related to the study’s retrospective design that should be noted. The data used was collected as part of COVID-19 public health operations and contact tracing initiatives making it at risk for systematic sampling bias. In addition, all studies with voluntary participation are vulnerable to volunteer bias favoring those who might be more likely to take the test leading to over-estimation of prevalence. We tried to limit the impact of this bias by excluding individuals who self-reported recent contact as their reason for taking the test; however, we did not cross-check other databases for recent history of contact information. The large sample in our study is likely to reduce this bias.
Another limitation is that we did not have patient-level data on symptoms and participants were not followed up for symptoms development or disease progression.
CONCLUSIONS
Community testing of asymptomatic COVID-19 persons implemented through the PHCC’s drive-through swabbing hubs is a crucial part of the ongoing efforts to reduce the spread of the disease and minimise its impact on the vulnerable population. The increasing scale of active testing will offer more information about the true scale of COVID-19 asymptomatic infections in the population of Qatar. Further research is needed to comprehensively understand the symptom’s progression and long-term clinical outcomes of Covid-19 on asymptomatic individuals.
Acknowledgments
The requirement for informed consent was waived by the Ethics Committee. The research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
The study was approved by the Institutional Review Board (IRB) of the Primary Health Care Corporation (PHCC) with a reference number PHCC/DCR/2020/07/075.
Data availability statement
No additional data are available.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Authorship contributions
MG Al-Kuwari, M.Abdulmalik, and AM.Mohammed: Conceptualisation, methodology and design. MG Al-Kuwari, AM.Mohammed: Original draft writing and preparation. AM.Mohammed, M.Kandy: Data curation and formal analysis. S.Abushaikha: project administration. MG Al-Kuwari, M.Abdulmalik, AM.Mohammed: Critically review of the article and final approval of the version to be published. All authors agree to be accountable for all aspects of the work.
Competing interests
The authors report no conflicts of interest in this work. The authors completed the unified competing interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author).
Correspondence to:
Azza Mustafa Mohammed, MBBS,MPH.
Address: Primary Health Care Corporation, Al-Meena st., Doha. Qatar.
Email: [email protected]