According to the World Health Organization (WHO), mental health disorders affect one in five persons, representing 1.54 billion people worldwide.1 Globally, these disorders are estimated to account for 13% of disability-adjusted life years (DALYs).2 In low and middle-income countries, it is estimated that between 76% and 99% of people with mental health disorders have no access to any form of treatment due to chronic underfunding in mental health and a lack of health facilities offering psychiatric care.3,4 This translates into a significant lack of trained mental health workers. In sub-Saharan Africa, it is estimated that 0.7 health professionals specializing in mental health are available per 100 000 inhabitants,5 which is far below the global standard of 9 professionals per 100 000 inhabitants.6
Burkina Faso counts 134 mental health professionals (9 psychiatrists, 5 psychologists, 2 social workers and 114 psychiatric nurses), a ratio of 0.78 professional per 100 000 inhabitants.7 More than half of the qualified medical staff are practicing in urban centers (Ouagadougou and Bobo-Dioulasso) where are located the country’s only two psychiatric hospitals.7 There is no legislation offering protection to individuals suffering from mental disorders, no specific budget ensuring consistent funding of mental health facilities and no national database providing an overview of the mental health needs of the population.7 As it is documented in other countries in the region, this lack of knowledge, resources and standards in the organization of services puts a burden on the families of people suffering from mental health disorders, as they find themselves having to provide care and protection for their relatives.8–10 In Burkina Faso, as in many low and middle-income countries, very little information is available regarding the prevalence of mental health disorders. Aside from studies conducted in clinical settings highlighting that psychotic disorders are the primary reason for psychiatric consultation in Burkina Faso,11–13 only three studies provide information on the prevalence of psychiatric symptoms in the population.
First, a recent study conducted among a representative sample of the general population residing in the city of Ouagadougou, the capital, reveals a very high prevalence of mental health symptoms.14 Of the 2587 people who participated in the study, 41.4% reported at least one psychiatric symptom. This study points out that, among all the psychiatric symptoms assessed, depressive episode was the most frequently observed diagnosis with a prevalence of approximately 11%. In this study, women were more likely than men to suffer from it.
Second, a study conducted a few years earlier in the outlying neighborhoods of the city of Ouagadougou - in which 2187 people were questioned about the presence of psychiatric symptoms - revealed a lower prevalence.15 Nevertheless, the results of this study suggest a prevalence of 4.3% of major depressive episodes among the general population, which would be modulated according to the socio-economic level of the households; people with poor physical health and low incomes being the most vulnerable to experiencing a major depressive episode.
Finally, a study carried out in rural areas in four distinct regions of the country with a sample of 1652 people described as indigent by their community identified an alarming level of psychological distress.16 In this study, 40% of the people interviewed reported more than 10 symptoms of anxiety or depression in the last month and 25% reported at least one psychotic symptom in their lives. Similarly to the results of Duthé and colleagues,15 the people most at risk of experiencing some form of psychological distress were elderly women, without income, illiterate and with poor physical health.
These few studies suggest that economic insecurity may act as a risk factor for psychological distress and may be associated with the presence of psychiatric symptoms which is consistent with results from studies conducted in other sub-Saharan countries.17–19 These studies highlight that poverty is an important predictor for the development of mental health disorders such as anxious, depressive, psychotic and somatic disorders.
In Burkina Faso, like in other African countries, the mechanisms and the factors linking poverty to psychiatric symptoms remain poorly understood. Moreover, existing studies do not distinguish socio-economic determinants according to the type of mental health symptoms observed, particularly among poor and marginalized populations. In this west African country, it is estimated that 40% of the population is living under the poverty line, and 11% of the population is living under the extreme poverty line.20,21 The individuals living in this precarious chronic situation can be qualified as indigents and are mainly settled in rural areas. In addition to living in a situation of social exclusion, indigents find themselves with little access to electricity, potable water, education and primary health care.16,18,22 Even though this is a population at high risk of living with impaired mental health and with an important prevalence of psychiatric symptoms, their mental health needs remain unknown.
METHODS
Setting, aim and design
The aim of this study is to describe the prevalence of psychiatric symptoms and their determinants among an indigent population living in rural Burkina Faso. For this descriptive and correlational study, a cross-sectional design was chosen. Burkina Faso is a country in West Africa with a population of 19 632 147 inhabitants, 77% of whom live in rural areas.23 The country is divided into sixty-three health districts. Each district is subdivided into several communes, which are themselves made up of villages.23 The country’s economy is based mainly on agriculture, livestock and trade. Gross domestic product per capita is $642 in 2017, which places Burkina Faso among the least developed countries according to the United Nations (UN) classification.24 Nearly half (43.9%) of the population lives below poverty line.23
Sampling procedure
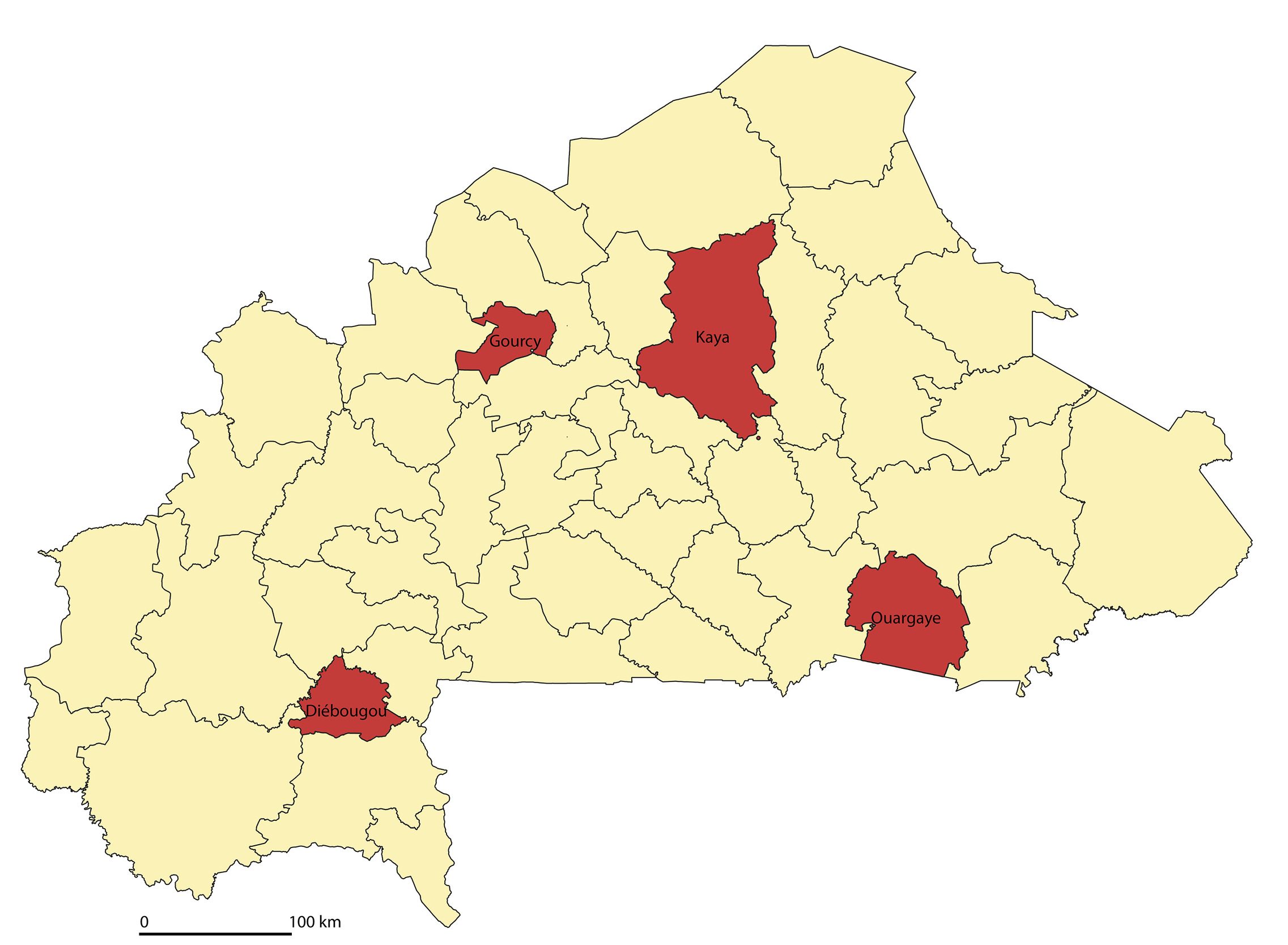
The results presented in this article are part of a larger study that was designed to evaluate the effectiveness of a community-based targeting process on access to healthcare of indigents implemented in 10 health districts in the country.25 Among the 10 districts where the intervention was implemented, 4 were randomly selected (Diebougou, Gourcy, Kaya, Ouargaye). The four health districts differ from one another (Table 1) in terms of the number of inhabitants and the main ethno-linguistic groups settled within their territory.20,26,27
For the current study, a stratified sampling procedure was employed. In the 4 health districts of the study (Figure 1), 26 municipalities were randomly selected, among which we randomly selected villages where at least 10 individuals (aged 18 and over) had been identified as indigents by a community committee according to their level of social and financial deprivation, their inability to take care of herself as well as their internal and external resources.16 This process led to the creation of a list of 51 267 individuals. This stratified procedure produced an original sample of 2000 indigents across the four districts. In total, 1599 people from the original 2000 sample were reached and constituted our sample for this study.
Data collection
The data was collected between February 15, 2017 and March 1rst, 2017. Trained interviewers visited indigents in their homes. After obtaining verbal consent, the interviewer questioned the individuals in local languages. Interviews lasted approximately 45 minutes and were conducted in the participant’s primary language. The interviewers had previously participated in the translation of the items into local language. In small groups, they were asked to find the best translation for the items so that the questions would be clearly understood by the participants. The translations selected were those for which the best inter-judge agreement was obtained. The questionnaire was administrated with ODK software on smartphones from which data was transferred daily to the main database for regular check-ups.
Instrument
The questionnaire contained 73 questions divided into five sections: socio-demographic information (10 questions), health status and service use (15 questions), financial situation (11 questions), functional capacity and support network (13 questions) and mental health status (24 questions). The questions on mental health included sub-questions on accessibility to care and help-seeking behaviors towards formal and informal resources.
Since no validated tool exists to assess the mental health status of indigent populations in West Africa, the questionnaire was built from three pre-existing instruments: the Refugee Health Screener (RHS-15), the Kessler Psychological Distress Scale (K-10) and the Composite International Diagnostic Interview (CIDI). Among these instruments, items that appeared relevant to the context under study were selected by all co-researchers. Once this selection was made, a workshop was held by members of the research team in collaboration with an anthropologist, a sociologist, a social worker, a psychologist, a psychiatric nurse. The participants were selected because of their good knowledge of the socio-cultural dynamics in the regions to be investigated and/or because they were working in the field of mental health in Burkina Faso for several years. The purpose of this workshop was to select relevant items and to formulate them considering the different cultural contexts. Participants selected items and their response options, reviewed and reformulated them to suit the indigent population. Some items were removed while others were added according to the local idioms of distress put forward by the panel members. The questionnaire was then pre-tested in an outlying neighborhood of Ouagadougou where the population shared many of the same socio-demographic characteristics as the study population. A final modification of the items was then made to ensure that the questions would be understood by respondents.
Variables
The socio-demographic variables used for this research were the followings: gender, age, geographic location of residence, literacy, marital status, number of children and cohabitation. The physical health variables contained in the questionnaire were: the presence of : an acute illness in the past six months, a chronic health condition, a disability and the perceived health status. Variables related to economic status were: the presence of an income-generating activity in the last week, the ability to meet daily food needs, the necessity to beg for food and the impossibility to receive medical assistance or to buy medication due to a lack of financial means.
Mental health variables
This section of the questionnaire contained 53 questions divided into six subsections: anxiodepressive (8 questions) and somatic (4 questions) symptomatology variables, including a question on the occurrence of a recent dramatic event (1 question); the individual’s general level of functioning (2 questions) and psychological distress (1 question); feeling of exclusion (7 question); psychotic symptomatology variables (4 questions), the frequency of these symptoms (2 questions) and restraint treatment (2 questions); the presence of stigmatized behaviours, such as drug use, public nudity and suicidal tendencies (6 questions) and help-seeking behaviours (16 questions).
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) 25 software. As the objective was to determine the prevalence of the three different types of symptoms and their determinants, only variables related to symptomatology were used as dependent variables, the others were used as independent variables. In order to assign an overall score for each symptom type to the participants, the questions related to one symptom type were grouped together, creating three overall variables. However, since the psychotic variable was not normally distributed, it was transformed into a dummy variable. As a result, participants were divided into the following two groups: those who had experienced at least one psychotic symptom in their lifetime and those who did not report any.
Since no research specifies how the symptoms of mental health disorders manifest themselves in an indigent population in Burkina Faso, an exploratory factor analysis was conducted to analyze the 8 items of anxiodepressive symptoms, the 4 items of somatic symptoms and the 4 items of psychotic symptoms. The goal was to observe how these items clustered together and thus identify the latent variable in each group of items. The maximum-likelihood method and an oblique rotation (direct oblimin) were used to perform this analysis.28
Two multiple regressions were used to identify sociodemographic variables related to anxiety and somatic symptoms (Table 4 and Table 5). Since the psychotic variable was dichotomous, a logistic regression was chosen to analyze the relationships between the sociodemographic variables and psychotic symptoms (Table 6).
RESULTS
Of the 1,599 indigent in the sample, 285 (17.8%) did not complete the questionnaire for the following reasons: absence from home (55.0%), death (32.6%) or illness (3.9%) and other reasons (8.5%). A total of 1314 questionnaires were completed, representing 82.2% of the initial sample. The sociodemographic data of the participants are shown in Table 2.
The results of the exploratory factor analysis show that the Kaiser-Meyer-Olkin Sampling Adequacy Measure is 0.84. Bartlett’s sphericity test is significant (χ2 (120) = 5847.35, P<0.001). The way the items are grouped indicates that the first latent variable includes anxiety symptoms, the second includes psychotic symptoms, and the third includes somatic symptoms. These three latent variables together account for 41.37% of the common variance, which indicates that almost half of the variance of the analyzed items is explained by these three variables. Table 3 presents the factor loading for the three latent variables.
Anxiodepressive symptoms
A total of 93.9% of participants responded having experienced at least one anxiodepressive symptom in the past month. The variables significantly correlated to this symptom are those presented in Table 4. Anxiodepressive symptoms were positively related to : health district, state of health, occurrence of a dramatic event, level of distress, level of overall functioning, feeling of exclusion, presence of somatic symptoms and stigmatized behaviours. These symptoms were negatively related to : age and the ability to fulfill one’s daily food needs. These variables explain 45.2% of the variance in anxiodepressive symptoms (R2 = 0.4552, F (28.1242) = 36.557, P<0.001).
Somatic symptoms
A total of 82.7% of participants responded having experienced at least one somatic symptom in the past month. The variables presented in Table 5 are related to somatic symptoms. Somatic symptoms were positively related to: health district, cohabitation, chronic health problem, health status, lack of financial means to obtain care, overall functioning, feeling of exclusion and anxiety symptoms. They are also negatively related to: having a disability. These variables explain 38.3% of the variance in somatic symptoms (R2 = 0.383, F (28.1242) = 27.50, P<0.001).
Psychotic symptoms
Finally, 19.5% of the sample responded having experienced at least one psychotic symptom in their lifetime. The variables related to psychotic symptoms are presented in Table 6. This table shows that psychotic symptoms were positively related to: health district, feeling of exclusion and stigmatized behaviours. These variables explain 13% of the variance in psychotic symptoms (R2 Nagelkerke = 0.130, χ2 (28) = 107.623, P<0.001).28,29
Here is a summary of the different determinants related to each of the symptoms (Table 7).
DISCUSSION
To our knowledge, the present study and its predecessor16 are the only ones to have explored how psychological distress is expressed in rural Burkina Faso and more specifically for a population of indigent people.
The results show the magnitude of a real problem considering that 96.8% of respondents reported at least one psychiatric symptom. In the past month, 93.9% of participants reported having experienced at least one symptom of anxiety or depression, 82.7% reported at least one somatic symptom, and 19.5% reported at least one psychotic symptom in their lifetime. The high prevalence of symptoms of mental health disorders shows that the indigent individuals experience psychological distress, although this problem is very little studied and health services are almost inexistent. This study suggests that psychological distress in this context is highly prevalent but expressed with great variation.
The results indicate that some determinants are specific to certain symptomatic profiles while others appear to be common. Among the common determinants, negative perceptions of physical health status are linked to anxiety and somatic symptoms.15,30 Several sources point out that depression is one of the risk factors for several physical health problems, such as cardiovascular disease, diabetes and human immunodeficiency virus (HIV).1,31 Inversely, these diseases also seem to contribute to the development of mental health problems.1,31,32 In addition, the results of this study show that several indicators of financial insecurity are related to anxiety and somatic symptoms, as has been demonstrated by others.15,33–35 In addition to the state of physical health and the level of financial insecurity that are related to the anxiodepressive and somatic manifestations of distress, the results reveal that two determinants are common to the three symptomatic profiles under study.
Geographic location of residence
The results showed variability in the psychological distress’s manifestations between the four regions studied. Among other things, they indicate that, compared to participants from Diebougou, participants from the Ouargaye region report more somatic symptoms, while those from Kaya are more likely to report psychotic symptoms. Beyond raising geographical differences in the symptomatology observed, our results do not allow us to conclude on the causality of such variations, nor on ethnic or cultural influence. There is, however, a large body of literature demonstrating the importance of these elements in manifestations of psychological distress.36–39 Qualitative research is therefore essential to better understand the factors influencing the observed differences.
The areas studied differ in several respects, including access to public services, regional poverty rates, social structure and family organization, to name just a few factors that may have an impact on symptomatological expression. For example, the territories of Gourcy and Kaya are predominantly composed of the Mossi cultural group, while the Yaana are the main cultural group in Ouargaye.40 Both the Mossi and the Yana have a patrilineal social structure. Within the Diebougou region, we find mainly the Lobi ethnic group, which have a bilinear social functioning, which means that some property is inherited from the mother and father.41
It is therefore possible that psychological distress manifests itself differently between ethno-linguistic groups. This geographic variability in the results illustrates a fundamental difference in the way in which this distress is experienced, perceived and expressed, which is reflected in the mental health symptoms observed.36–39 It is also possible that elements such as accessibility to certain types of care and social acceptability may partly explain the observed differences.36–38 Furthermore, beliefs related to the causes of a disorder and help-seeking behaviors have been shown to diverge according to the group to which one belongs and according to existing systems of care.36,39,42 These results therefore suggest that geographic region must be considered in the development of health policies in order to optimize the supply of mental health services. But obviously, these findings merit more in-depth qualitative research.
Exclusion and stigmatization
Respondents report feeling excluded from their community, regardless of the type of symptoms reported. Indeed, a feeling of exclusion is present for 54.6% of participants with anxiety symptoms, 56.9% for those reporting somatic symptoms and 69.1% for those reporting psychotic symptoms. This result is consistent with those of other studies conducted in sub-Saharan Africa, suggesting that mental health disorders are strongly associated with stigmatizing attitudes leading to significant discrimination.43–45
Studies in Nigeria and Uganda show that respondents perceive people with mental health disorders as, for example, harmful, dangerous or incompetent.42,46 Studies on the stigmatization of mental health disorders in the African context show that these attitudes are particularly pronounced for severe psychotic disorders, such as schizophrenia.17 However, people with depression and those around them also report being stigmatized in their communities.45,46
The results of the present study point in the same direction and confirm the presence of a feeling of exclusion among the various forms of psychological distress in rural Burkina Faso. Such a stigma surrounding mental health disorders has considerable negative impacts, for example by hindering help-seeking behavior.43 These discriminatory attitudes add a significant burden to an already marginalized and resourceless population, where the community may be the only possible support. Thus, considering the considerable prevalence of mental health symptoms and the social isolation they face, the indigent people surveyed are at risk of experiencing various forms of exclusion in their communities. This stigmatization must be perceived by leaders as a barrier to the use of services and must be the subject of sustained attention in the creation of health policies targeting mental health disorders.
Limitations
Since mental health disorders are stigmatized in the studied population, it is possible that some participants may have been reluctant to discuss the topic and may have denied the presence of symptoms, thereby underestimating the prevalence. This situation is obviously not unique to the population in this study in Burkina Faso and is found throughout the world. In addition, the questionnaire used is based on three Western tools. Despite consultation with local professionals, it is possible that certain modes of expression of psychological distress were not included in the questionnaire items. Finally, a bias could stem from the sequence in which the items were presented in the questionnaire, which was divided by construct. This non-random presentation of symptoms may potentially have enhanced the internal consistency of the items.
CONCLUSIONS
The mental health action plan 2014-2018 in Burkina Faso7 identified the lack of evidence in mental health as one of the most salient issues. This study contributes to addressing this limitation and participates in the Movement for Global Mental Health (MGMH) by providing knowledge on the prevalence of symptoms of mental health disorders in a vulnerable population living in rural areas. It demonstrates the presence of regional differences that should be considered in the development of future mental health policies and in the organization of health services. In order to comply with WHO standards,1 this study stresses the importance of training health workers within health structures as well as community-based health workers and increasing the number of mental health professionals in rural areas. Training should put emphasis on 1) detection and treatment of the most common mental health problems and disorders, and 2) development and implantation of mental health prevention activities specific to different socio-cultural contexts. These activities should focus on reducing the stigmatization and exclusion of people with mental health problems. Locally developed initiatives should consider the economic precariousness and social vulnerability of people in situations of indigence and tailor interventions to the specific needs of these people.
Acknowledgements
The authors would like to thank Maurice Yaogo for his contribution to this article, the AGIR team who participated of the data collection, Paul-André Somé for his collaboration with the design of the questionnaire, Emmanuel Bonnet for the design of the map as well as all the participants who made this research possible.
Funding
This work was supported by the Canadian Institutes of Health Research (CIHR) through the project “Community research studies and interventions for health equity in Burkina Faso” (Grant number ROH-115213).
Authorship contributions
LPM carried out the data analysis and wrote the manuscript. EPG conceptualized the project, monitored the data collection, supported the data analysis and was a major contributor in writing the manuscript. VR conceptualized the project, obtained funding for the project and provided support in writing the manuscript. CD supported the data analysis, provided support in writing the manuscript and was the research director of the main author. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests (includes financial and non-financial). The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author) and declare no conflicts of interest.
Correspondence to:
Lyann Porfilio-Mathieu, Speech and Langage Pathology and Audiology Department, Université de Montréal, Canada.
[email protected]