Neonatal mortality rates (NMR) in Somaliland were 42 per 1000 live-born in 2011—among the highest in the world.1 More recent estimates are projections with large uncertainties.2 The latest Levels & Trends in Child Mortality states an NMR of 37 in the wider Somalia, down from 45 in 1990.3 Such slow decline is often seen in fragile states.4 Compared with the previous 30 years, a ten-fold improvement in yearly mortality reduction will be needed to reach the third Sustainable Development Goal (SDG) NMR of 12 by 2030.5
The Ministry of Health (MoH) in Somaliland has previously identified neonatal healthcare as one of several areas that need particular attention. By the end of 2021, the national development plan targets an NMR of less than 35/1000.6,7
Neonatal health interventions can be grouped into a) preventive and community-based interventions, including antenatal care; b) improved immediate peripartum care for mother and baby; and c) curative and supportive care for sick and small/premature newborns. All components seem necessary to reach the NMR target.8 In low- and lower middle-income countries (LLMIC), curative care by itself can save 20–30% additional lives.9,10 Inpatient treatment of small and sick newborns is currently facing the largest implementation challenges among all maternal and newborn interventions in African countries and has received too little attention in newborn health programming in conflict areas.11,12 Somaliland is no exception. There is a huge need to scale up quality neonatal inpatient care to bridge the necessary continuum of care (Figure 1). Leaning on estimates from Kenya and India, there should be as many inpatient neonatal beds and neonatal nurses in a hospital as there are deliveries per day.13,14 At present, a crude birth rate of 37.4/1000 population, an estimate of 4 million Somalilanders, and a facility delivery coverage of 33% translates to 136 births per day – and needed number of NSCU beds and nurses.15 Full delivery coverage would require about 400 beds and nurses.16
With this grand challenge at hand, a neonatal special care unit (NSCU) with second-level care capacity was established in the top referral chain of Somaliland in the year 2013.10
This article describes the process and output of a broad package of interventions framed within the six WHO health system building blocks.17 We characterize the neonatal ward population and the level and quality of care for the purpose of comparison. We also present challenges and lessons learned along the way. We hope that hard-won experiences can be valuable for health workers, program managers, and governmental officers, especially in fragile states with little progress in NMR reduction.4
METHODS
Setting
Somaliland is the breakaway republic in the North-Western corner of Somalia, bordering Djibouti and Eastern Ethiopia. Hargeisa Group Hospital (HGH), Somaliland’s only governmental tertiary hospital, was built in 1953. Today it has a capacity of about 450 beds, including medical and surgical wards, radiology department, and lab services. Several medical and nursing schools utilize HGH for practical teaching and training. Three maternity wards serve about 5500 deliveries a year.18 Vacuum and Caesarean Sections (CS) are performed on strict indications, contingent on the families’ consent.
Until 2012, sick neonates were treated alongside the mother or in the pediatric wards of the hospital with no specific allocated staff, management guidelines, resuscitation protocol, or registration of neonatal outcomes. Premature and small for gestational age (SGA) children were usually discharged as soon as the mother was fit to leave. From the perspective of the neonate, service readiness and quality were sparse and reflected the neonatal service in the public hospitals of the country at large.
Data
A mixed-methods approach is presented in this article. We assessed administrative documents from Jan 2013 to Dec 2014 and obtained information from key staff involved in the NSCU for the qualitative descriptions. We also performed a retrospective, structural assessment of labor and newborn readiness for care in August 2013, using data collection forms and standard operating procedures from the Nairobi Newborn Study.19,20 An observational, retrospective cohort study of 164 patients admitted to the NSCU from June to October 2013 (the first 5 months of regular NSCU activity) provides the quantitative characterization of the neonates. After ward discharge, research assistants phone-interviewed primary caretakers in Somali. We assessed the families’ experience with the NSCU-care using a 5-point Likert scale and translated a final, open response into English. Further details about the cohort study with the outcome of the intervention on neonatal mortality and morbidity have been published elsewhere.18
We plotted the quantitative data in EpiData v.4.0. Descriptive analyses were performed in Microsoft Excel v.15.32 and IBM SPSS Statistics 25. We recoded birthweight and gestational age into ordinal variables. Birth, admission, and discharge dates were the basis for temporal variables.
Ethics
All the caregivers provided informed consent for the phone interview. The database was de-identified before statistical analyses. All work was conducted following the declaration of Helsinki ethical principles for research.
PROCESS, OUTPUT, AND EXPERIENCES
The hospital director initiated the NSCU program and involved international stakeholders already providing mother-child health (MCH) in Hargeisa city. Health Poverty Action (HPA), which supported the city’s primary MCH clinics, the referral system, and the maternal wards in HGH, provided funds for infrastructure and equipment. In addition, NNM - a regional nongovernmental organization - was ready to provide technical, logistical, and capacity-building expertise.
In light of previous disruptions of international health operations and limited financial and technical resources in the community, the partners identified 6 overarching principles in the inception phase:
-
Focus on doing basic activities well before moving on to more advanced activities.
-
Local sustainability of furniture, equipment, and consumables.
-
Modeling quality care, derived from every woman and child’s inherent equal value, uniqueness, and dignity.
-
“Training the trainer’s” philosophy in all educational components.
-
Conceptualize the maternal and neonatal wards as 1 entity where integration and capacity building should flow in both directions.
-
Stepping up all necessary interventions simultaneously.
The partners undertook a needs assessment within the framework of the 6 WHO health system building blocks, identifying necessary activities and interventions for establishing facility-based care of small and sick newborns.17 We repeated the assessment as the ward developed. Table 1 describes the final, comprehensive package of interventions.
We searched for a comprehensive guide that could support the identified principles, training, and work and chose the Integrated Management of Pregnancy and Childbirth (IMPAC) guideline Managing Newborn Problems: a Guide for Doctors, Nurses and Midwives, supplemented with Kangaroo mother care, a practical guide for the management of premature and small for gestational age (SGA) babies. Both are published by the WHO.21,22
1. Infrastructure
HPA erected the NSCU inside the maternity ward as a 4x4-m, wall-protected cubicle about 15 m from the labor room (Photo A). The cubicle was able to host 4 critically ill neonates within its boundaries at a time. Neonates with minor health issues were monitored and treated alongside their mothers in the maternal wards close to the labor ward. Table 2 summarizes how we equipped the unit.
Often, adjustments of new equipment were necessary, and the local manufacturing processes could take several months. Phototherapy machines were made in a metal workshop using regular “white” fluorescent tubes following principles described elsewhere.23 We placed resuscitation tables and warming lamps with infrared exchange bulbs in the labor room and outside the cesarean section operation theatre. Continuous Positive Airway Pressure (CPAP) was provided by modifying adult oxygen prongs in half-filled water bottles (Bubble-CPAP) using guidelines from the Kijabe Hospital in Kenya (Photo B).
Reliable electric power was a continuous challenge. Under-dimensioned electrical wiring and regular power-cuts put heaters, monitoring devices, and oxygen concentrators out of service. Infrared bulbs, extension cables, and fuses of regulators had to be changed more often than expected. Battery-powered electrical equipment and backup oxygen cylinders helped us maintain continuous treatment in most situations. Although several up-to-date incubators had been donated to the hospital, challenges with power, cleanliness, and sustainability kept us from using them. The staff gradually learned to calibrate and maintain most of the unit’s equipment, but major repairs were still a challenge: We were not able to train local technical maintenance staff.
2. Medical products and technologies
Several necessities were not available in Somaliland at the time of implementation (Table S1 in the Online Supplementary Document). We had to import Phenobarbitone iv, Cefotaxime iv, and 10% glucose despite all being on the WHO Model List of Essential Medicines for Children.24 Even so, finding the appropriate medical disposables was a bigger challenge than medicines. Dialogue with a pharmaceutical whole-seller company to stock the items in-country did not materialize. Instead, the ward developed a lockable store for items that international hospital staff brought from Kenya at irregular intervals. We used a simple stocking system with “in and out” signing to ensure accountability.
At the time of the cohort study, vaccination was not a routine activity of the NSCU. The provision of OPV, BCG, and Tetanus was incorporated during 2014 in collaboration with the local WHO office.
Although Somaliland is a hot country, winters and nights may be chilly. With a little tradition for baby clothes and diapers, hypothermia is a common challenge. A sub-project called Ilmo Dugsoon (Keeping Babies Warm) provided 2 diapers and locally tailored newborn jackets, socks, and hats in cotton and fleece (Photo C). Small, premature, and hypothermic newborns were clad in knitted wool sweaters and blankets, if not kangaroo cared, or under infrared warming lamps.
3. Health workforce
NSCU staff
Eligibility criteria for neonatal nurse training were diploma or BSc and fluency in English since trainers would have to be international. We developed a 3 months intensive training course followed by 9 months internship. Managing Newborn Problems: a guide…21 was the core curriculum of the study, delivered by 40 hours of didactic teaching, 300 hours assisting in the NSCU and labor ward, and 40 hours of trainee-to-mentor practice of necessary skills.21 We standardized skills and procedures using the free videos from the Global Health Media Project category “small baby, newborn and breastfeeding”.25 A supervision-signed logbook ensured that every skill was performed correctly and independently a sufficient number of times. Students had to pass exams with MCQ and short answers, neonatal resuscitation OSCE, case scenarios, and medicine calculations (Appendix S1 in the Online Supplementary Document).
A pediatrician, a nurse specialist in neonatal intensive care, and a bi-lingual BSc nurse trained the first 6 neonatal nurses between February and May 2013. A second course, utilizing the first batch as assistant trainers, was run from October 2013 to have 12 fully trained neonatal nurses in the unit after 1 year. This course ran into a number of recruitment disagreements and was delayed for several months. Furthermore, 2 trainees left the course despite receiving a salary, the prospect of losing a new degree, and the contractual obligation of reimbursing the training cost incurred.
Two motivated junior doctors signed a one-year training contract. They were trained in the same curriculum as the neonatal nurses and received further lecturing and supervision from the pediatrician over the next 9 months. Several internet resources and books were identified and made available in the ward (Appendix S1 in the Online Supplementary Document).
At the end of 2014, the neonatal nurse course was approved by the Ministry of Health and National Health Professions Commission as a one-year postgraduate diploma in neonatal nursing
Training and integration of undergraduate curriculums
All neonatal trainees, most midwives, operation theatre staff, and medical students in GYN/OBS/PED rotation were trained in basic neonatal resuscitation through the Helping Babies Breathe simulation course in collaboration with the Kenya Paediatric Association (KPA).26 The accreditation ratio was above 90%. To help the staff transition from resuscitating a mannequin to confidently resuscitating a newborn, the 3 international trainers spent considerable time encouraging and supervising in the labor room. Mannequins were available in the wards for weekly re-training under the supervision of 3 hospital staff, who had become trainers in the HBB course. As the HBB skills spread across hospital staff and medical students, we saw a massive increase in resuscitation efforts and positive newborn outcomes.
Medical students in pediatric rotation received training in basic neonatal assessment and followed the medical doctors in clinical work. The skills obtained were integrated with their clinical logbook and the final pediatric OSCE exam.
4. Information systems and monitoring
Identification, registration, diagnosis, and treatment
Admission criteria for the NSCU are presented in Table 3. The neonatal register book utilized the hardware of the general national in-patient ward book, but provided new headings glued on top of the existing, expanding the number of variables from 1 to 2 pages (Table S2 in the Online Supplementary Document). In this way, the hospital Health Management Information System (HMIS) was upheld, whereas additional and necessary information was recorded and stored systematically in anticipation of an MoH-approved neonatal HMIS.
With the need for accurate vital signs monitoring and medicines/fluid provision, the existing hospital charts for pediatric patients were abandoned and new charts developed: The most important was the admission chart with clinical findings, medicine administration, monitoring of vital signs, and feeds chart. Evaluation of their usability was an ongoing process, and all charts underwent minor modifications.
Because there were no nationally approved treatment protocols for small and sick neonates, we developed NSCU protocols for resuscitation, sepsis, fluid requirements, hypoglycemia, seizures, phototherapy, and HIV prophylaxis from the 2 essential guidelines,21,22 adding elements from new evidence.27–30 Regular death audits based on the principle “no name, no blame, no shame” were modeled with guest teachers from the KPA, but were not incorporated routinely.
The HBB trainers supervised maintenance of resuscitation equipment and did weekly registration of availability, functionality, and cleanliness. This type of ongoing vigilance was unfamiliar to the hospital staff and not possible to sustain over time.
The mean missing information ratio from the NSCU register book was 10% across 19 variables during the cohort study. Apgar score (1–5min), minutes of resuscitation, discharge diagnosis, and weight were missing in 77%, 42%, 16%, and 9% of cases, respectively. The most recorded variable was delivery type with 98%. To uphold the quality of the register, we implemented weekly assessments followed by reminders and clarifications.
Inpatient characteristics
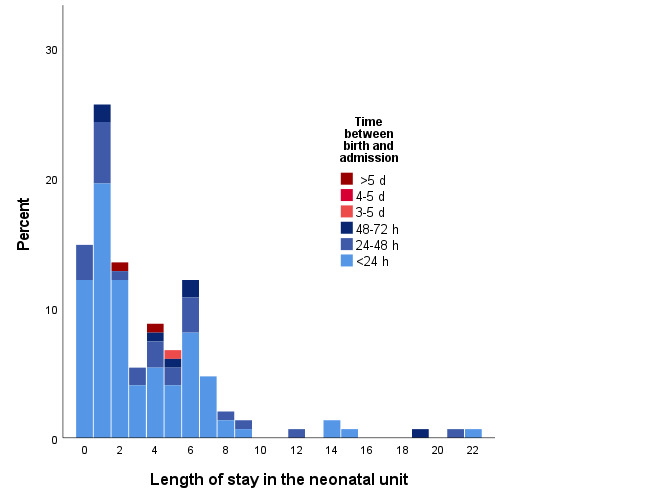
Of the 72 neonates that received ventilation with bag-valve-mask (PPV), median, 75, and 90 percentile ventilation times were 3, 5, and 10 minutes, respectively (Table 4). Birthweight below 2500g affected 32%. The distribution of gestational age by birthweight in clinical categories is presented in Figure S1 in the Online Supplementary Document. Seventy-four percent were admitted between birth and 24 hours of life, and 75% of children were discharged within 5 days (Figure 2). The overall self-discharge rate was 29%, and 25 out of 164 (15%) died during the hospital stay.18 In 16% of cases, at least 1 main diagnosis was revised between admission and discharge (Table 5). At discharge, there was also an increase in more mature pathophysiological diagnoses from 50 to 69%. There was a tendency of “lumping” of identical diagnoses within certain weeks. The data revealed that 79% of the neonates received K-vitamin soon after birth, whereas tetracycline eye treatment and BCG were not provided at all.
User satisfaction
We asked the caregivers how they found the stay and care at the neonatal unit. Of the 90 respondents, 11 were never present in the neonatal unit. Among the remaining caretakers—mainly mothers— 8 (10%) rated the stay as very poor or poor, 10 (13%) found it acceptable, 28 (35%) good, and 33 (42%) excellent, with an average mean /median score of 4.0, 5 being the maximum score.
The women were encouraged to elaborate on the rating. Three caretakers had negative experiences related to absent staff, poor thermal control, and lack of oxygen. A thematic grouping of the positive comments indicated that the staff was caring, hardworking, supporting, competent, and available around the clock. The emphasis was on “well cared for” and “good staff.” Many respondents underscored the importance of providing oxygen, medicines, feeds, warm clothes, and diapers.
Structural assessment
A systematic inventory of equipment, consumables, and medicines for labor and newborn care provided an overall score of 66%. Readiness of care required a score higher than 80% (Table S3 in the Online Supplementary Document).19
5. Leadership, governance and task distribution
Training contracts for neonatal trainees and work contracts for staff were put in place. We agreed about salary with the hospital administration and the MoH, trying to find a level that honored their additional competency and yet locally sustainable.
A practically-oriented job description was instrumental in communicating expectations and setting a standard in areas where improvement was desirable (Appendix S2 in the Online Supplementary Document). Supervision of new trainees, and medical and nursing students, was part of this description (Photo D). We developed standard operating procedures that guided admission, treatment, care, handling of equipment, and shift reports.
The 2 medical doctors worked 4 hours in the morning, 6 days a week, and otherwise shared on call. Together they provided about 80 hours of active work per week during the cohort study.
One of the neonatal nurses was appointed head of the ward with extended responsibilities, including making rotas. Two or 3 nurses usually covered the ward at all times, divided into morning, afternoon, and night shifts with short overlaps for oral shift reports. With fixed times for hospital staff transport, this overlap was challenging.
We trained mothers with their families to be actively involved in caring for their sick newborns: They should be able to administer feeding and warming/KMC and discover danger signs.
Families living close to the hospital were encouraged to return for follow-up after discharge. We followed some small/premature children for months; others were never seen again.
As the NSCU developed a positive reputation, private hospitals also wanted to improve care for sick newborns. During 2014, some of the nurses were recruited to other hospitals in addition to, or instead of (when contracts expired), forcing the hospital to employ nurses without neonatal training for work in the NSCU.
Coordinative meetings between the NSCU and the maternity wards, hospital administration, the MoH, INGOs, and UN stakeholders became essential in ensuring that efforts were moving in the same direction.
6. Health care financing
Budgeting was incomplete at the outset because the running cost was challenging to predict. In retrospect, with about 50 patients and an average of 200 bed days per month, the running cost was approximately US$140 per patient and US$35 per bed day (Table 6). The average price of medicines, feeds, and disposables in treatment of 1 neonate per 24 hours in 2013 were US$10–15. Of this, 2–5 were out of pocket. The group of implementers covered 80–90% of the total running cost. Few families declined admission for financial reasons.
Additional costs in the package of interventions were the training courses themselves, 2 short-term teams from the KPA, the 3 international clinicians, and a full-time intervention/program manager employed by NNM.
Several INGOs and national institutions shared the financial responsibility for establishing and running the NSCU. It soon became apparent that multiparty contracts, including budgets, were necessary for assessing commitment and fostering transparency. Still, financial constraints and payment delays were common.
Community awareness and advocacy
There had been a widespread perception among health workers at the hospital that nonbreathing, small, and sick neonates were beyond treatment. A few months into the package of interventions, this attitude started to change, as staff eye-witnessed blue-tinged, nonfeeding, fast-breathing, and convulsing newborns stabilized and beginning to thrive. Families arriving home with live children from the newborn unit were the best ambassadors for spreading this new expectation of newborn treatment to the community. Albeit not in our initial plans, we realized that the NSCU could create a community expectation for better newborn healthcare in general. The graduation of the neonatal nurses was broadcast on national television, and later, the President’s wife made an official visit to the neonatal ward. A short documentary about the unit, with the aim of community awareness and crowdfunding, was also developed and spread on social media (https://www.youtube.com/watch?v=0IZOJPFbdz8).
Overwhelming needs
Towards the end of 2013, the NSCU was overwhelmed with an increasing number of sick neonates referred from other hospitals and MCH’s. With the momentum now created, a new neonatal ward of more than 100 m2 was designed, built, and equipped close to the labor room through funds from several stakeholders. The ward was officially opened in September 2014. Six key staff visited 2 neonatal intensive care units in Addis Ababa, Ethiopia, in preparation for establishing and managing the new and larger ward.
DISCUSSION
We have described the implementation of a broad package of interventions aimed at improving survival and reducing morbidity in small and sick newborns at the top referral hospital in Somaliland.18 The implementation process and output have been analyzed within the framework of the 6 health system building blocks.
Infrastructure
We had positive experiences with inviting the local crafts community to tailor the main components of the NSCU. The benefits were easy access to repairs and duplication and increased community involvement. The trade-off was less accurate and efficient equipment, but not important enough to discourage this strategy for the future.
Medical products and technologies
There are several whole-sellers of medical consumables and medicines in Somaliland. We assumed that at least one would be willing to import necessities on our behalf. However, apparent demand or an expectation of a growing consumer volume is necessary before commercial import becomes attractive. If not a governmental activity, a possibility in the future could be to ensure a long-term monopoly contract for such items, making it more likely that initial financial loss will be covered in the long run.
Health Workforce and Training
In light of the critical shortage of health workers in many LLMIC, there is an ongoing exploration of how to create the needed neonatal staff.31,32 We opted for recruiting BSc nurses because we were restricted to train and supervise in English. We also hoped they would be instructors in later neonatal nurse courses. Meanwhile, long term, the question remains: Shall neonatal staff be trained from BSc or auxiliary midwife/nurses? In our experience, the general ability to learn, specific mathematical skills, and a caring and thorough attitude are more important than a broad health professional training, similar to suggestions from India33,34 and Malawi.35
The importance of ensuring that a new training program is appropriately integrated with the national health staffing plans from the outset cannot be overemphasized; similarly, to ensure a seamless transition from trainee to hospital employee when finances for new permanent positions are restricted and need political negotiation.
The neonatal nurse curriculum of 3 months duration was trimmed to the bone: Integrating didactic teaching with the relevant protocols in the ward secured a short way from learning to implementation. Practically all opportunities were used to teach and mentor “as we worked.” The skills logbook ensured proficiency and experience before performing critical skills alone. Developing and getting approval for a postgraduate course is resource-demanding, and we strongly support the call for better coordination and resource availability across LLMIC.32
Every health worker involved in labor with newborns needs the skills of basic newborn resuscitation and care. Nurses and midwives in Somaliland were exposed to several different neonatal life-saving skills courses run by various programs in 2012–14. Having the hospital—or, even better—the country sticking to 1 training course and resuscitation protocol is beneficial in collaboration, staff deployment, re-trainings, and monitoring of performance and outcome.
Twelve neonatal nurses soon became fewer, and the remaining were overloaded. We should have trained between 18–24 to absorb trainee dropout, absenteeism, sick and maternity leave, and holidays. Likewise, doubling the number of doctors trained would make their on-call duties sustainable, bearing in mind that they also did work in other departments or hospitals.
Information systems and monitoring
In our experience, it takes time to develop a culture of documentation, information flow, and monitoring, and even longer to start using these data for quality improvement (QI). Register book completeness was at the level of a similar assessment in Kenya, but the recording of vital information needs further improvement compared with hospitals in other LLMIC.36,37 In places where mortality audits are implemented well, it turns out to be a critical learning and QI tool.38 We wonder if a lack of confidence in the “no blame” policy made implementation difficult.
Our leading guide for NSCU development, diagnosis, and treatment, the Managing Newborn Problems: a guide…, fitted our needs.21 Focused on clinical symptoms and signs as the basis for management and treatment, it was well suited for a hospital with limited diagnostic capabilities and did not even require the correct diagnosis for proper case management. The book is used in numerous LLMIC across the world. Published in 2003, it is now in dire need of a slight expansion and inclusion of new evidence. We believe an improved layout and more use of flow charts would improve usability further. Turning the book into a smartphone app may increase the potential for use and ease regular updates.
More than half of the neonates needed support and monitoring less than 72 hours. Seventy-five percent were discharged within 5 days, almost identical to 76% in a comparable Ethiopian study,39 but shorter than the average of NSCUs in India.16 The findings demonstrate a high turnover in the NSCU and the potential to prevent disability and death with modest investments.
A self-discharge rate of 29% warrants further investigation, viewed in contrast to the low self-discharge rate of 2.7 and 1.7% in a Nigerian and South Sudanese study.40,41 So also with the admission of only 35% girls, less than in Kenya (45%), but equal to findings in rural Ethiopia (35%) and North–Central Nigeria (38%).36,39,40
Comparing the distribution of diagnoses, birthweight, gestational age, and mortality outcome in the NSCU, 15% mortality is quite similar to achievements from NSCUs in neighboring countries, detailed elsewhere.18
“High-quality health services use evidence-based practices; are well-organized, accessible, and adequately resourced; are safe, efficient, timely, and people-centered”.10 When asked, mothers in our study generally indicated high service satisfaction. Their answers were quite similar to other women across the globe who prioritize affordable, respectful, and dignified care; water, sanitation, and hygiene; medicines and supplies; and an increased number of competent and well-supported midwives and nurses.4,42
The structural assessment showed a need for further improvement of the availability of medicines, disposables, and equipment: A score of 66% corresponds to the lowest quartile of hospitals with neonatal services in Nairobi County.
Ward activities
Despite all the evidence-grounded work in the NSCU, we acknowledge several possibilities for improvements. First, we had too little focus on the prevention of retinopathy of prematurity (ROP). ROP is a growing challenge in LMIC and is now estimated to constitute 10% of all childhood blindness on the African continent.43 Second, we did not develop protocols on clustering care, proper positioning, and pain management, partly because it was unrealistic to pay attention to “soft” targets when the staff capacity was limited, and the focus was on skills to increase survival. Third, KMC was an unfamiliar concept in Somaliland and, for reasons that need further qualitative exploration, was challenging to implement on a broad scale. Some families, however, embraced the idea, and even a few fathers did kangaroo care. Last, our post-discharge follow-up for premature babies was not systematic. In light of the widespread, long-term problems documented after a stay in neonatal units in LMIC, follow-up needs further specialized development, including outreach services for rural and nomadic families.44–46
Leadership and governance
Modeling efficient and respectful supervision is necessary for skills building and QI, another to incorporate such supervision into everyone’s job description. We had positive experiences with including the expectation in the position title, like “assistant trainer” and adding a small bonus to the monthly salary. Envisioning the country’s long-term goals may help individuals view themselves as part of something bigger and create a desire for change.
Like a clockwork, an NSCU is more than the sum of the individual components, and the quality never better than the weakest building block. To excel, the staff need to conceptualize how a complete NSCU or NICU is meant to function. In the transition from the smaller to the larger NSCU, it was helpful to visit several larger NICUs in Ethiopia and discuss and process strengths and weaknesses in what we experienced. When the staff realized that our “infant” NSCU, in some aspects, was performing at the level of reputable institutions in the region, it created a sense of pride and eagerness to develop further.
The Somali people have a strong oral tradition, and written agreements and documents cannot enforce compliance. We found that flexibility and consensus seeking, as new challenges arose, were necessary for something to work well. A too rigid program in its methods, implementation, or timeline is almost bound to fail in a Somali context.
Although the packages of interventions touched peripartum care through close collaboration with the labor ward and HBB training of midwives, there was never a programmatic integration of the two intersections of maternal and newborn health (MNH), and conflicts of interest were inevitable. If possible, we believe care of laboring mothers and small and sick newborns should be administratively under the same head, with shared responsibility for survival and disabilities.
We experienced that training and clinical work challenges often originated at the administrative and regulatory level, and it was necessary to engage at all levels, simultaneously or consecutively, to find solutions. As supported by research, we gradually realized the importance of top-down, well-coordinated policies, targets, programs, funding, protocols, HMIS, and training manuals.4
Health care financing
The implementation model of this NSCU required considerable funds, mainly for infrastructure, major technical equipment, and the cost of hosting an international team during the first year. Such a “kick-start” will probably also in the future require international support; most of the public funds for health care in Somaliland are vested in local staff salaries. However, financial sustainability will increase as the national staff become the new program managers and trainers. Somaliland has a growing private-for-profit health care segment, also covering MNH. Competition for highly skilled health staff necessitates a strong focus on retention within the public health system. Collaboration with local communities in the recruitment of trainees may create stronger social expectations of and support for continued service within the public MNH system.
CONCLUSIONS
Starting a public hospital NSCU in a Somali context is feasible when implementers are able to bridge gaps on all health system building blocks simultaneously. The major challenges in implementing quality service for small and sick newborns were poor availability of medicines and other neonatal disposables, lack of a national regulatory framework and funding allocation, and staff unfamiliarity with detailed protocols, standard operating procedures, and job descriptions. Public demand for facility-based newborn care is present and may grow quickly with awareness campaigns and proof of concept. Without a continuous overcapacity in neonatal nurse training courses and a firm retention policy, neonatal nurses will soon be absorbed by other parts of the health system. We believe this broad package of interventions has a potential for further scale-up to district hospitals in Somaliland, possibly using the NSCU at HGH as a national training hub, but a long-term sustainability assessment of this first NSCU is yet to be done.
Acknowledgments
The Somaliland Health Minister and the hospital director of HGH gave the ethical approval for utilizing the data (Ref: MoH/DG/2014). The Norwegian center for research data (NSD) approved the handling of sensitive data.
We want to thank the former hospital director Faduma Kahin who initiated the NSCU at HGH and later hospital directors for continued support. We want to thank Mohamed Mosa, Faduma Hassan, Pia Fagerholm, and Ingjerd Heen for their tireless work towards the NSCU and help in data collection and manuscript revision. We commend the essential contributions of Kenya Paediatric Association. Finally, we want to acknowledge the neonatal doctors and nurses in the NSCU, some of which have dedicated their lives and careers to save the lives of small and sick newborns in Somaliland.
Funding
EH, KML, AA, and FVW have been supported by grants from the Norwegian Agency for Development Cooperation (Norad/Digni). Norad was not involved in any other parts of the research project.
Authorship contributions
EH, KS and KML were responsible for the study design. EH, KML, AA, and FVW collected the data. EH wrote the draft. All authors contributed to the interpretation of data and revision and approval of the final manuscript.
Competing Interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.
Corresponding author
Espen Heen, MD, MPhil, DTMH.
Helsam, Pobox 1130 Blindern; 0318 Oslo, Norway.
[email protected].



.jpg)


.jpg)


.jpg)

.jpg)