The rate of newly diagnosed cancer cases continues to rise worldwide, with a projected increase of 47% by 2040.1 Of the 19 million new cancer cases and 10 million deaths worldwide in 2020, GLOBOCAN reported an incidence and mortality rate of 5.7% and 7.2% respectively for Africa.1 The high share of cancer deaths in relation to incidence in Africa can be attributed to many factors such as lack of resources for screening, advanced stage at diagnosis, unavailability of the spectrum of adjuvant treatment options, low rates of health literacy and possibly higher incidence of aggressive histologic types of cancer.2 As the burden of disease in sub-Saharan Africa transitions from communicable to non-communicable diseases (NCD),3 it is imperative that clinicians adapt in communicating diagnosis, prognosis and treatment strategies with their patients and families. Telling patients about their cancer diagnosis allows them to make decisions about treatment options, plan their life affairs, and marshal appropriate resources for treatment.
Telling a patient about a cancer diagnosis can introduce enormous emotional problems, distrust and despair if not done well. Studies conducted in Western and Asian populations have shown that the overwhelming majority of people would like to know from their physician if they were diagnosed with cancer, along with concrete information about treatment options.4–9 A telephone survey of respondents in the general population in Hong Kong by Fielding et al. revealed that 95% of participants would like to know their diagnosis,9 while Sankar et al. found that 87% of patients with cancer at a single center in India either absolutely needed to know or would like to know if their diagnosis is cancer.8 In the cohort of Indian patients, 91% preferred to defer treatment decisions to their physician, which is contrary to results from previous studies in the US, UK and Hong Kong, where majority of participants indicated that they wanted a shared-decision making with their physician.4,5,7,9,10
Far less is known about the information preferences of individuals at risk for cancer in sub-Saharan Africa. In a society that is highly paternalistic, physicians exercise great autonomy in how, when, and to whom they disclose patients’ medical diagnosis and prognostic status.11,12 Often, diagnosis and prognosis are shared with family members but not the patients themselves.11,12 The objective of this study was to investigate the information preferences with regards to cancer diagnosis and prognosis of a cross-section of Ghanaians. Understanding the information needs and preferences of people in Ghana may help improve communication and quality of care for patients with cancer in sub-Saharan Africa with similar socio-cultural constructs.
METHODS
Survey design and setting
We conducted a survey of Ghanaians over the age of 18, living both in and outside of Ghana, using a questionnaire adapted from previously published work evaluating cancer information preferences of residents in the UK and India.6,8 The survey was divided into two parts: Part 1 included demographics and questions about personal experience with cancer, and Part 2 included questions about desire to know diagnosis and what specific information would be important to have (see Online Supplementary Document). The survey was piloted with a group of 10 Ghanaians living in Ghana and the US to ensure cultural relevancy. Informed consent was implied by completing the survey. Approval for this study was obtained from the institutional review board at the University of Michigan.
Survey distribution
A Qualtrics (https://www.qualtrics.com/, Provo, UT, USA) link was used to distribute the survey on WhatsApp (https://www.whatsapp.com/, Menlo Park, CA, USA). WhatsApp accounts for 90% of the information flow in Ghana,13,14 and is increasingly being used in the public health space for conducting long distance education, tracking medication adherence, and providing specialist support for both communicable and non-communicable diseases.15,16 Qualtrics provides for secure, reliable transfer of survey responses and HIPAA compliant health data.17,18 The initial links were distributed through established medical and social groups. Participants were subsequently asked to then forward the link to their social contacts.
Statistical analyses
The overall goal of our analysis was to understand the cancer information needs of Ghanaians living in and outside of Ghana, and to determine if there were any factors associated with reduced information needs. Reduced information needs was defined as answering “No” or “Not Sure” to wanting to know the diagnosis if diagnosed with cancer. Participant characteristics were compared using χ2 and t-tests as appropriate. Participant characteristics included age, gender, habitancy, marital status, highest education level, and past or current cancer diagnosis in self or a family member. To determine if these factors were associated with reduced information needs, we performed univariate logistic regression. All statistical analyses were performed using STATA, version 16 (STATA Corp, College Station, TX, USA). Statistical tests were two-tailed and used P < 0.05 as the threshold for significance.
RESULTS
A total of 426 participants responded to the survey. Of these 426 participants, 35.2% were male, 33.1% were female and 31.2% omitted gender information. Pertinent demographic data of participants is shown in Table 1. Three hundred and forty-eight (81.9%) participants were living in Ghana at the time of the survey. The majority of participants were between the ages of 21 and 40 years old (67.6%), were married (63.2%), and reported that their highest education level was Graduate/Professional school (60.8%). Few (4.0%) reported a past or current cancer diagnosis, but 29.9% reported a past or current cancer diagnosis in a family member. Overall, 412 (96.7%) reported that if they were diagnosed with cancer, they would want to know the diagnosis. Of note, all patients who reported a past or current diagnosis of cancer said they would want to know a cancer diagnosis.
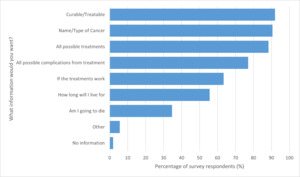
Participants who wanted to know their diagnosis were then asked what information they would want from their physician (Figure 1). The three most common responses were wanting to know if the cancer was curable/treatable (92.0%), the name/type of cancer (90.6%), and what all the possible treatments were (88.3%). Of note, 8 (1.9%) respondents said they would not want any information beyond knowing they had cancer. Figure 2 lists the reasons for not wanting further information. Worrying about impact on family was reported by 5 of these 8 respondents. Less commonly reported were not being able to pay for tests or treatment (n=1) and feeling scared (n=2). In univariate analysis, no factors were found to be significantly associated with reduced information needs (Table 2).
DISCUSSION
Little is known about the information needs of cancer patients in sub-Saharan Africa. Understanding of patients’ preferences with regards to diagnosis, prognosis and treatment is crucial to be able to provide optimal care. Our survey of a cross-section of Ghanaians living in and outside of Ghana showed that the overwhelming majority of participants would like to know if they were diagnosed with cancer. Most of our survey respondents also prefer to know about treatment options for their cancer. Unlike previous studies on cancer information needs of participants, we utilized mobile technology which allowed us to reach a greater cohort over a wider geographic region.
In a study of 133 patients with cancer treated at a single, tertiary hospital in India, Sankhar et al reported that 81% of patients absolutely wanted to know if their diagnosis was cancer.8 In terms of specific information needs, 18.7 % and 40.6% wanted to know the name of cancer and chance of cure respectively.8 In a telephone survey of 1136 Chinese in the general population of Hong Kong, Fielding et al found that 95% of patients would like to know if they were diagnosed with cancer, and 97% would want information on prognosis.9 Studies from the US, UK and Scotland showed that > 95% of patients wanted to know if their diagnosis was cancer.4,6,19 Our findings parallel the trend of the strong desire to know if one’s diagnosis is cancer, whether it is in the US, Europe, Asia or Africa. While the percentage of respondents in the Ghanaian cohort who wanted to know their diagnosis is comparable to cohorts from Hong Kong, US, UK and Scotland, it is substantially higher than the 81% reported in the cohort from India.8 Similar to the study from Hong Kong by Fielding et al., our survey respondents were individuals from the general population, while the participants in the other studies were patients with cancer.4,6,8,9,19 Only 4% of our survey participants had a current or previous diagnosis of cancer, although nearly 30% reported a history of cancer diagnosis in a family member. Given the similarity in percentage of respondents who desired to know their diagnosis of cancer between our study and other studies conducted in patients already receiving treatment for cancer, it does not appear that a personal history of cancer impacts the desire to know of a new or future diagnosis of cancer.
Three hundred and ninety-two (92%) survey respondents wanted to know if their cancer was curable while 376 (88.3%) wanted to know about all possible treatment options. These findings are encouraging as majority of the survey participants did not consider cancer diagnosis as an automatic death sentence as has been previously reported in some qualitative studies from sub-Saharan Africa.20,21 There seems to be an increase in awareness of cancer among Ghanaians22,23 and therefore, it is important that clinicians tell patients of their diagnosis so they can seek timely and appropriate treatment.
Nearly 70% of our respondents were between 21–40 years of age and 61% had a graduate or a professional degree. Others have shown that younger demographic group are more generally inclined to seek information about a cancer diagnosis, prognosis or treatment.5,9 The majority of our respondents are young, educated and have ready access to internet and therefore the pattern of cancer information seeking trend is not much different from other parts of the world with similar age and educational demographic. It is imperative that providers adapt to the new generation of patients in sub-Saharan Africa who desire more information about their cancer diagnosis, prognosis, and treatment options.
Among our survey respondents who did not desire any further information beyond the diagnosis of cancer, a worry about the impact of their diagnosis on their family was the reason reported by nearly 63% of respondents. Although it has not been studied in the Ghanaian context, other studies done in Europe and China have found that a significant number of parents are hesitant to disclose their diagnosis of cancer to their children due to their worry about the impact of diagnosis on the children.24,25 Our survey did not ascertain the parenthood status of respondents; however, we can extrapolate from the data on age and marital status that a significant proportion may be parents, hence their concern about impact of news of cancer diagnosis on their family. In a qualitative study by Iddrisu et al of 12 Ghanaian women with breast cancer, social stigma and ostracization emerged as one of the common reasons why people did not like to disclose their diagnosis.26 Iddrisu et al. also found beliefs to strongly influence patients perception of cancer. For example, some patients felt breast cancer was caused by “spiritual and evil forces or human enemies.”26 Contrary to the finding of strong impact of spiritual beliefs in the study by Iddrisu et. al, only 3 participants in our study did not want any information about their diagnosis because they felt “God was in control”. We did not identify any unique factors in our cohort of Ghanaians that was associated with decreased information needs.
Our study has some important limitations. While the use of mobile technology allowed us to have a wider geographic reach of Ghanaians, our study sample may be biased because only people with access to mobile phones and internet participated. Given the ubiquity of mobile phones in Ghana, we think that the impact of the above limitation on our study is very low. The higher educational achievement rate among our participants compared to the general population of Ghanaians suggests sampling bias as the index invitees were younger and more educated although our univariate analysis did not show any differences in information needs based on level of education. Additionally, local practices could influence the cancer information needs of Ghanaians who live outside of Ghana. However, 80% of participants were living in Ghana at the time of the survey and therefore, the impact of foreign influence is likely low. Finally, nearly a third of respondents did not indicate their gender. Gender was set to optional in the survey which means that participants were not required to complete it to proceed to subsequent questions. We elected to make participant disclosure of gender optional in an attempt to improve inclusivity while also not offending participants by attempting to list categories that may or may not be applicable to them.
CONCLUSIONS
Our survey of Ghanaians living in and outside of Ghana shows that the overwhelming majority would like to know from their physician if they were diagnosed with cancer. This finding is in line with previous studies done in the US, Europe and Asia. The results of this study should encourage medical practitioners in Ghana to tell patients about a cancer diagnosis and share other pertinent information on cancer with them. The paternalistic practice of withholding important medical information from patients is unethical. Our data suggests that individuals want their providers to talk to them about a cancer diagnosis and share practical information so that they can make the best decisions about care and treatment. Providers need continued training in how to communicate difficult news to patients, and to engage in shared decision making with patients around options for curative or palliative care. Future research should include qualitative studies to explore participants’ experiences and preferences regarding communication about a cancer diagnosis. Research on the attitudes and behaviors of medical practitioners in Ghana with regards to sharing a cancer diagnosis, prognostic and treatment information is also needed, in order to inform training programs. As cancer treatment programs expand globally,27,28 the importance of early, accurate diagnosis and sharing of diagnostic, prognostic, and treatment information with patients in sub-Saharan Africa should not be overlooked.
Acknowledgements
Approval for this study was granted by the Institutional Review Board of the University of Michigan
Funding
None.
Authorship contributions
E.A.A: study conception, study design, data collection, data interpretation, manuscript writing and revision; A.L: data analysis, data interpretation, manuscript writing and revision; M.H.W: study design, data interpretation, manuscript writing and revision; C.K.D: study design, data collection, data interpretation, manuscript revision; E.A.M: study design, data, collection, data interpretation, manuscript revision; G.K: study conception, study design, data collection, data interpretation, manuscript writing and revision.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.
Corresponding Author:
Elliot A. Asare, MD, MS, FACS
1950 Circle of Hope
Salt Lake City, UT, 84112
Tel: o:8012136090
Fax: 801-585-3749
E-mail: [email protected]