Globally, advancements have been made to improve maternal and child survival in recent years.1 Between 1990 and 2015, maternal mortality worldwide reduced to 216 deaths per 100,000 live births, representing a 44% decline.2 During the same period, substantial improvement was made towards the Millennium Development Goal (MDG) target of reducing under-five mortality by 75%. The under-five mortality rate declined from an estimated 91 deaths per 1,000 live births in 1990 to 43 deaths per 1,000 live births in 2015.3 However, neonatal mortality declined at a slower pace than child mortality and progress was uneven. Neonatal mortality rates remain unacceptably high in many parts of the world.1,3 Annually, an estimated 2.4 million newborns die within the first 28 days of birth, which is approximately 6,700 neonatal deaths occurring per day.4 Accounting for more than 40% of deaths in children under-five, the major causes of neonatal mortality are preterm birth complications, intrapartum related events and infections.5 Most of these deaths are preventable with timely health interventions.5 In the Sustainable Development Goals (SDGs), the global community has committed to reduce neonatal mortality to less than 12 neonatal deaths per 1,000 live births by 2030.6
Due to the inconsistent progress in ending preventable neonatal deaths during the MDG era, only some countries are positioned to achieve accelerated progress in the SDG era.7 To date, there is limited understanding of the factors that may have driven the declines in neonatal mortality rates in the MDG era. Given the challenges with assigning attribution, few studies have attempted to identify the high impact interventions at the sub-national level or examined the social, policy, and programmatic factors that contributed to reductions in neonatal mortality.8–11 As national estimates often hide sub-national disparities, studies that focus on the sub-national level are urgently needed to inform local strategic planning and programming committees to reduce inequity and set subnational regions on the trajectory to end preventable neonatal deaths.12
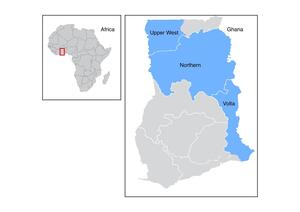
The Northern, Volta, and Upper West Regions of Ghana present an ideal case study to understand sub-national variation in factors that led to declines in neonatal mortality in the MDG era in Ghana. According to the Ghana Demographic and Health Survey, from 1993 to 2014, the neonatal mortality rate (NMR) in Ghana declined by 44%, while the Northern region, the largest in the country, documented a 67% reduction. By contrast, the declines in NMR in the Volta Region and the Upper West Region were well below the national average, 25% and 10%, respectively.11
The Northern Region is the largest of the ten regions in Ghana, with a population of 2.86 million.13 The region has seen a rise in the number of health professionals and an influx of nongovernmental organizations (NGOs) in the past decade. For example, in 2003, there were only 27 doctors and 831 nurses that were working in the Northern Region, but by 2014, these numbers increased to 117 and 4,438, respectively.14 Additionally, a total of 181 government health facilities, including 83 Community-Based Health Planning and Services (CHPS) compounds were established or expanded to serve the population.15 The Volta Region, despite having a smaller population than the Northern Region (2.39 million) had more CHPS compounds, district hospitals, midwife/maternity centers and better doctor-to and nurse-to patient ratios.16 The Upper West region is far less populated than the Northern Region, with a population of 771,394.16 Between 2003 to 2014, the number of doctors in the region increased from 11 to 21.16,17 Nevertheless, in 2014, it had the lowest number of midwife/maternity centers, district hospitals, clinics, and CHPS compounds in the country.16 Understanding the differences in local policies, program strategies, availability of resources, and intervention coverage at the sub-national level is crucial to accelerating progress towards ending preventable neonatal deaths by 2030.10,18
The objectives of this study were two-fold. First, we assessed how coverage of proven newborn interventions contributed to the patterns of decline in neonatal mortality in the Northern, Volta, and Upper West Regions of Ghana during the MDG era. Second, qualitative interviews were carried out in the Northern Region to understand the program strategies and community actions that likely led to the drastic declines in the NMR in the MDG era. The findings of this study provide evidence to support the identification, prioritization and scale-up of high-impact, evidence-based neonatal interventions to attain the SDG target and increase the equity of health gains across geographical strata.
METHODS
This mixed-methods study considered three regions of Ghana: Northern, Volta, and Upper West Regions (Figure 1). Taken together these three regions represent 21.5% of the country’s population.19
Quantitative component
The Lives Saved Tool (LiST) was used to estimate changes in mortality between the years 2003 and 2014 to determine the extent to which each intervention resulted in a reduction of NMR. LiST is a multi-cause probabilistic model that estimates changes in various indicators, including: under-five and neonatal mortality rates and deaths, maternal mortality ratios and deaths, stillbirth rates and deaths, and causes of death based on changes in coverage of maternal, newborn and child health interventions.18,20 Based on the health interventions modelled in LiST, 30 had an impact on all-cause neonatal mortality (Figure 2).
Coverage of interventions and measures of the health status of the population were obtained from the Ghana Demographic and Health Surveys (DHS) for 2003, 2008, and 2014,21–23 and the Multiple Indicator Cluster Surveys (MICS) for 200624 and 2011.25 Subnational coverage data were available for 11 of the 30 neonatal health interventions in LiST. In cases where neither subnational nor national estimates were available, no changes in intervention coverage were modeled (e.g., kangaroo mother care). Population estimates at the subnational level were obtained from the 2010 Ghana Census.19 Default values for intervention efficacies and population affected fractions as presented in the current LiST model were applied. The number of lives saved (i.e., additional deaths averted) as well as changes in mortality rates overall, by cause and by intervention, were extracted as outputs from LiST. All LiST analyses were conducted using Spectrum version 5.70 (released June 27, 2018).
Qualitative component
The qualitative component of the study sought to gain contextual understanding of the factors that contributed to the significant decline in neonatal mortality in the Northern Region. The analysis sought to address two primary research questions: Based on experience, how do healthcare workers, policymakers, and community representatives believe that changes in intervention coverage have impacted neonatal mortality rates at the subnational level? Thinking toward the future, which high impact interventions do these stakeholders believe will drive further reductions in neonatal mortality rates during the SDG era?
In-depth interviews (IDIs) were conducted with 38 participants: 3 government health officials, 12 health workers, 7 staff from non-government organizations, and 16 community leaders, including traditional birth attendants and local chiefs. Key informants who could provide historical information about programs, policies, and activities that were implemented in the Northern Region between 1993 and 2014 were purposively selected. Participants were recruited through snowball and maximum variation sampling approaches.
Interviews were conducted in English and the local languages, Dagbani and Twi. The main topics of the interviews included: program history, policies, policy implementation, programmatic inputs, community engagement, best practices, strategies, and success stories that relate to neonatal mortality. Each interview lasted between 25 and 60 minutes. Participants also completed a background questionnaire that captured their demographic and professional information. All interviews were audio-recorded and transcribed verbatim by the research team after each interview. The research team met daily to discuss the themes of each interview. Consensus on data saturation by the research team was used to determine the final sample size of 38 interviews.
Interview transcripts were analyzed thematically, using an inductive approach to develop a codebook. Three research assistants individually used a line-by-line coding approach for the first five interviews. The team met to discuss the codes and resolved differences through discussion. A codebook was then created to define the boundaries of each code. The codebook was systematically applied to the transcripts. From the codes, the research team identified common themes about interventions that contributed to reductions in neonatal mortality and around persistent health challenges that need to be addressed to reach the SDG goals.
Ethical approvals
The study was approved by the Ghana Health Services Ethical Review Board [GHS-ERC:15/05/17]. All in-depth interview participants signed a written informed consent.
RESULTS
Trends in intervention coverage and neonatal mortality rates, 2003-2014
Overall, patterns of coverage for the period 2003 to 2014 showed dramatic variation by intervention (See Figure 3). From 2003 to 2014, improvements in the coverage of insecticide treated bed nets (ITNs) outpaced all other interventions examined. Changes in the coverage of health facility deliveries, iron supplementation, intermittent preventive treatment (IPTp), oral rehydration solution (ORS), and clean postnatal practices occurred at a much slower pace. Coverage of improved sanitation, tetanus toxoid vaccination and use of piped water remained stagnant during the period.
Neonatal mortality rates (NMR) in the three regions exceeded the national rate of 34 deaths per 1,000 live births in 2003 (Northern Region: 43 deaths per 1000 live births; Volta Region: 39 deaths per 1000 live births; and Upper West: 35 deaths per 1000 live births) (Table 1). By 2014, the NMR varied by region, with the highest NMR in the Northern Region, 36 deaths per 1,000 live births, and the lowest in the Volta region, 21 deaths per 1,000 live births. The reductions in NMR were in large part attributable to increases in the coverage of case management of sepsis and pneumonia in neonates, improvements in labor and delivery management, neonatal resuscitation, clean postnatal practices, and malaria interventions (ITNs and IPTp) (Table 2). Overall, the scale-up of these interventions between 2003 and 2014 led to annual rates of reduction of greater magnitude than the national average for the Volta Region. By contrast, the annual rate of reduction was lower than or at the national average for the Northern and Upper West Regions. Notably, the Volta Region started with an NMR exceeding the national average in 2003, and by 2014, the NMR in the Volta Region was substantially lower than the national average.
Qualitative
The qualitative analysis shows that the contextual factors that contributed to NMR reduction in the Northern Region included multiple strategies, which focused on implementing known effective interventions. Findings were organized around three themes: (1) health care access and quality (2) health education and (3) prioritizing neonatal health. They included health facility, community, and policy level interventions.
Health care access and quality
Increased health care access was cited as a key contributor to neonatal mortality reduction. More public hospitals and health facilities (including compounds at the community level) were built across the Northern Region. This increase in the number of health facilities was mentioned by many informants as helping to eliminate geographic barriers in accessing care. A number of these facilities, particularly government hospitals, invested in neonatal intensive care units (NICUs) to better care for ill or preterm newborns. The greater presence of NICUs in the region was also felt to have significantly reduced neonatal mortality.
"Before 2011, there was only one newborn care unit in the whole Northern Region, which was in this hospital. But beyond 2011, we now have a minimum of six in the Northern Region." -Health worker
Improvements in quality occurred at all levels, from health clinics offering primary care to the regional hospital offering tertiary level care. Policymakers stated that facilities without NICUs focused on keeping preterm newborns warm through the promotion of Kangaroo Mother Care. Both policymakers and health workers discussed that facilities placed a heavy emphasis on resuscitation practices, with increased training for health workers and increased availability of supplies for neonatal resuscitation. NGO staff reported developing workshops to train doctors, nurses, and midwives involved in labor and delivery.
“[The most important was] the training on Helping Babies Breathe… And when the baby is small, there is a way you should care for the baby, including those that can be put on kangaroo mother care. [So we emphasized] those kinds of things.” -Government policymaker
In addition to the hospitals, many respondents mentioned the establishment of the CHPS zones, which are community-based health centers designed to bring nurses closer to the community. The expanded number of CHPS zones provided the opportunity for new mothers to bring in their newborns for necessary routine check-up appointments, enabling health workers to promptly identify any potential danger signs or health problems.
“I think the CHPS program [is the most important factor], where we have sent services closer to the people… which made it more accessible geographically.” -Government policymaker
Government policymakers claimed that the existing transport system had also been strengthened enough to impact mortality in districts across the Northern Region. They stated that “community emergency transport systems”, in which ambulances were driven and maintained by community members, had been established for people living in communities farther away from urban centers, and were more readily available to transport women in labor to health facilities.
“And then we have a community transport system in place when you easily call and then they transport so they don’t delay.” -Government policymaker
However, community leaders and some health workers did not believe the community transport system was functional. Many felt that the community emergency transport system would be more functional with the use of motorcycles, which would greatly alleviate the burden of travel on pregnant women who are often forced to navigate poor roads, rivers, and the consequences of the rainy season, to access care at the facility level.
“Some of the communities are far from the health centers and hospitals … they don’t visit the hospitals unless they are seriously sick.” -Community health nurse
Community respondents identified the main driver of improvement in neonatal mortality as the increase in health care access, partly due to the ongoing expansion of CHPS facilities. Community members discussed the need for health care access when complications arise, feeling that many mothers recognized danger signs but were unable to quickly access care. Some community members were vaguely aware of improvements at the facilities, especially when there were shipments of equipment or medications, but were generally not aware of specific improvements for advanced medical care.
Health workers and policymakers saw the main difference as the recent improvements in quality of care, including the provision of more specialized care (such as NICUs), and improvements in infection prevention and control. Many facility staff members believed that the initiatives around Essential Newborn Care, including the basic training on newborn resuscitation, had an impact on reducing immediate postpartum neonatal mortality.
“We have the teaching hospital too, that has a bigger newborn care unit with a specialist. So at the district hospital… if they cannot manage, then they refer these cases to the teaching hospital where we have a specialist.” -Government policymaker
“So far, what we have done mostly has been to look at essential newborn care in this first strategy, we concentrated a lot on essential newborn care that is immediately after the child is born.” -Government policymaker
“Handwashing has been encouraged, how to clean the baby, the things used to clean the baby after delivery, and how to treat cord care.” - NGO worker
Health education
Health education was a key focus named by respondents at every level. The community level strategy developed by the Ghana Health Service targeted volunteers, community health nurses, and community participants to educate community members on newborn care and the benefits of facility delivery. In an effort to reduce the number of home deliveries, Ghana Health Service specifically trained traditional birth attendants (TBAs) on the dangers of conducting deliveries outside of the institutional setting and established a system that positioned them as link providers between pregnant women and health facilities.
“At the community, what we did was we also trained community-based agents, volunteers…TBAs, and mother-to-mother support groups.” -Government policymaker
While most respondents agreed that health education was a main driver of neonatal mortality reduction, there were some differences in how the strategies were viewed. Community respondents emphasized the importance of the inclusion of the entire family, the identification of local champions, and the need for buy-in from the entire community. Health care workers and government policymakers focused almost entirely on the need for pregnant women and new mothers to know danger signs and have access to health care centers.
“Even if a mother delivers in the community… they [the family members] bring the person [to the facility] and apologize for the reasons why they could not bring to the clinic and why the woman delivered in the house.” - Community leader
“There are a lot of vibrant groups in the community, like we have the market women who form groups, you have the women who form mother-to-mother support groups so that if one mother has a problem then maybe she could use the support group.” -Health care worker
Increased national attention on newborns
Government policymakers noted that earlier initiatives to achieve the MDG of reducing child mortality failed to adequately address the issue of neonatal health, leaving newborns in a particularly vulnerable position. In the context of the Northern Region, this oversight translated into an insufficient amount of data on neonatal mortality, a limited understanding of the barriers to positive neonatal health outcomes, and deficiencies in the amount of personnel and resources invested into neonatal health-related capacity building.
“[We need] to build capacity and provider resources for newborn care right from the healthcare level right to the community level.” -Health worker
From 2007-2015, the country implemented the Ghana Under-5 Child Health Policy and began discussions around the need for a newborn-specific strategy (which was officially launched in 2014). Many respondents felt that this was the reason that there was a stronger focus on facility-level interventions including delivery management, postnatal care, and neonatal resuscitation. Life-saving maternal and newborn commodities were also added to the Essential Medicines list.
“Logistics, oxygen, newborn care instruments – if we are able to sustain them and continue with the good work, I think we should be able to achieve the SDGs.” -Senior community health nurse
Both policymakers and health workers stated that as they became increasingly aware of the need to treat neonates as a separate entity, a series of neonatal health-related interventions were implemented in the Northern Region.
“One of the key things that has actually changed was now we realize that we need to focus on the newborn as a separate entity, … because the things that worked for the older child don’t necessarily work for the newborn.” -Health worker
“So one of the things I really think contributed to this change is … the change in policy in the whole country is in the way we look at the newborn.” -Health worker
DISCUSSION
Multiple interventions and strategies contributed to declines in neonatal mortality in all three regions. Of significance were interventions that focused on increasing access to skilled attendance at birth. For the Volta and Upper West Regions, labor and delivery management accounted for about a third of the decline in the newborn deaths. In the Northern Region, the decline was largely attributed to control and management of infections in newborns (sepsis and pneumonia). Additionally, there were variations in the interventions that led to the decline in NMR across the three regions. For example, malaria prevention using insecticide mosquito nets and intermittent preventive treatment of malaria during pregnancy were important contributors to the decline in mortality in the Upper West Region, but not in the Northern or Volta Regions.
The findings of the study contribute to the global discourse on how to further drive down NMR and increase access to life-saving neonatal interventions in low- and middle-income countries (LMICs). Several studies, including systematic reviews and meta-analyses, show that skilled attendants at birth, case management of sepsis and pneumonia, improvements in obstructed labor management, clean birth and postnatal practices, and malaria interventions save newborn lives in LMICs.26–31 One mathematical model of neonatal health interventions in sub-Saharan Africa estimated that clean delivery practices, clean cord care, and antibiotics alone could prevent 88.4% of neonatal deaths.32 We identified similar interventions; however, different interventions may need to be prioritized at sub-national levels.
One persistent challenge in neonatal health is how to increase access to existing life-saving interventions.33 Overcoming inadequate coverage requires partnership across multiple sectors, engagement with health care workers and caregivers, strong support from local and national leadership, and strengthening all levels of the health facility.33 We found that the Northern Region of Ghana significantly benefited from national and local prioritization of newborn health. The creation of the country’s Under 5 Child Health Policy and beginning discussions around a national Every Newborn Action Plan34 contributed to an increase in neonatal-focused training for health workers, such as neonatal resuscitation and management of sepsis. Health care infrastructure was strengthened by increasing the number of health facilities and establishing NICUs for very sick infants, which was coupled with facility-based infection prevention measures. Additionally, non-profit organizations actively participated to address barriers to accessing health facility births, through partnerships with local chiefs and female leaders, engagement with families, and behavior change communication. Thus, the strategy that increased coverage of life-saving interventions involved policy, prioritization, partnerships, prevention, and provision of infrastructure.35–37 These actions targeted all aspects of the ecological level-individual, family, community, organizational, and policy- and can be implemented to maximize coverage of evidenced-based interventions in similar settings and countries.33
The results of the LiST analysis in this study are difficult to compare with other studies, as LiST is a deterministic model. Thus, different inputs into the model (e.g. year, baseline coverage levels, coverage targets) will produce different results. In addition, most of the LiST analysis focused on sub-Saharan Africa countries have concentrated on forecast models of under-5 mortality broadly.38–42 Moreover, many studies do not disaggregate the neonatal period from the post neonatal period,38–42 nor have they explored factors responsible for historical declines in neonatal mortality in different contexts.43–46
In a forecast LiST analysis in the KwaZulu-Natal province of South Africa, McGee et al found that improved labor and delivery management would save the most newborn lives over a 15-year period, compared to other interventions.44 Our work provides evidence to support scaling up effective labor and delivery management strategies. We found that improved access to and quality of labor and delivery management contributed the most (about a third) to the decline in neonatal mortality in the Volta and Upper West Region of Ghana. In the Northern Region of Ghana, it was the second leading contributor to neonatal lives saved.
The policies, programs, and other contextual factors that accelerated the neonatal mortality decline in the Northern Region of Ghana are consistent with findings from several other studies in LMICs, and point to the need for effective community engagement.47 One comprehensive review evaluated 93 community-based primary health care interventions to determine their effectiveness in reducing neonatal health in LMICs, including Ghana. Similar to our findings, they found that participatory women’s groups, reducing barriers to skilled attendants at birth, improving knowledge of newborn danger signs, and promoting better cord care, reduced neonatal mortality.47 In Rwanda, Khurmi and colleagues48 found that strong political commitment, provision of quality health services, healthcare performance-based incentives, and improving care-seeking behaviors among mothers significantly reduced maternal mortality over 15 years, but had minimal effect on neonatal mortality .Our qualitative results suggest that to achieve significant reductions in neonatal mortality, active community engagement, such as promoting women support groups, bolstering community knowledge about neonatal health, and including community leaders may be critical. These efforts should be implemented in tandem with political commitment, resource investment, and improvement in quality of services.
There are several limitations worth noting. Due to the unavailability of sub-national coverage data, the potential impacts of several key interventions (such as chlorhexidine and kangaroo mother care) were not modelled in the LiST analysis. The qualitative component was designed to understand the context and progress in the Northern Region, and thus the findings may not be generalizable to other regions. Further, mothers and families were not directly interviewed about their experiences, and it is possible that they may have different perceptions about the most effective interventions. However, this analysis highlights important components of newborn care programs that could be supported and scaled to accelerate progress towards improving neonatal survival.
CONCLUSIONS
By highlighting successful strategies and interventions, these results provide several opportunities for Ghana to further reduce neonatal mortality. The strategies that supported the reductions in neonatal mortality can be continued and strengthened, and the challenges identified can be addressed. Understanding what has worked and what has not can help effectively plan to save more newborn lives in the future.
Acknowledgements
The authors wish to thank Leonie Akofio-Sowah and Elizabeth Amoliga for supporting data collection. They are also grateful to Dr. Isabella Sagoe-Moses and Dr. Linda Vanotoo for connecting the research team to relevant stakeholders.
Funding
The funding for this project was through Global Affairs Canada via Savanna Signatures. CO, LA, BS were supported with funding for Brown University Minority Health International Research Training Grant [T37MD008655 ]. KW was supported by Oakland University Provost Graduate Student Award. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authorship contributions
KS, MK, AL, PO conceptualized the study. MK performed the LIST analysis and wrote the quantitative results. ES, CO, LA, KW performed the qualitative data analysis and participated in the writing. KS and PO supervised data collection and qualitative analysis. ES and KS wrote the first draft of the manuscript. CZ performed the literature review. All authors critically reviewed and edited the manuscript.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/disclosure-of-interest/ (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Kwame Sakyi, PhD, MSPH
Center for Learning and Childhood Development-Ghana
A.F 3190, Accra, Ghana.
Oakland University
Department of Public and Environmental Wellness
School of Health Sciences
403 Meadow Brook Rd, Rochester, MI, USA
Email: [email protected].

.png)


.png)
