Electronic health records (EHRs) are essential to a health services-oriented digital health framework1 that strengthens health systems and improves the access, equity, safety, and quality of health services. However, the uptake of EHRs has been limited, despite the World Health Organization (WHO) publishing an EHR manual for lower- and middle-income countries (LMICs) more than a decade ago.2 National EHRs are a high priority in high-income countries and there has been broad adoption of EHRs across different levels of healthcare service delivery in these countries. However, the development and use of modern EHR systems in LMICs are nascent or nonexistent.3 EHRs enable the capture, analysis, use, and exchange of patient-level data for both patient care and population health management.4,5 Yet, LMICs have limited capacity for health data exchange (HDX) across organizational boundaries.6 A recent report by the WHO and United Nations Children’s Fund highlights the limited or absence of data exchange capabilities in LMICs.7 International donors and governments are increasingly prioritizing investments to support the use of patient data captured in EHRs for patient care and their reuse in the aggregate form for program management. For example, the national digital health blueprint (NDHB) of the Government of India describes the vision for developing a digital infrastructure that will facilitate the collection, exchange, and use of patient and aggregate health data across the country.8 The World Bank’s World Development Report 2021 reiterates the importance of the use and reuse of data for development efforts, including for public health emergencies such as the COVID-19 pandemic.9 However, the evidence needed to enable HDX at national and subnational levels in India to support data use for healthcare service delivery and reuse for program management is lacking and is compounded by the scarcity of research evidence on the use and reuse of data (Figure 1).10
The objectives of this study were to propose an HDX model for improved maternal health service delivery and program management at hospital, state, and national levels. The study focused on two research questions, namely what are the essential design and development requirements, and how will the model enable HDX to support the use and reuse of data for improved maternal health service delivery and program management at hospital, state, and national levels?
METHODS
Study setting
A tertiary care state government hospital (TSGH) in India was selected as the case study site. State government hospitals are the foundational component of the expected HDX exchange envisioned at the national level in the country. National- and state-level health leadership offered their support for the study, which proved critical for data collection given the focus on a public health setting and in light of the COVID-19 pandemic.
Study design and ethics
A qualitative study design was used to document health data needs, systems, processes, roles, and responsibilities to enable HDX for improved maternal health service delivery (antenatal care, childbirth, and postnatal care) and program management at the hospital, state, and national levels. The study was designed to examine and document data systems and processes inside and outside the hospitals, with a primary focus on the TSGH. The study did not explore an individual event or cultural phenomenon or develop a theory11,12 as the case study design was applied.13–15 Moreover, the study did not compare the TSGH selected with another TSGH inside or outside the state in which the case study was conducted. Last, the study did not investigate HDX implementation or how HDX can support educational and research requirements of the TSGH. A single case study was adequate to collect the data required to answer the research questions and was feasible within the available time and funding constraints. The Institutional Review Board (IRB) of the University of North Carolina at Chapel Hill provided the study with a notification of exemption from further review (IRB number:19-3200).
Sampling plan
A total of 20 key informants were purposively selected for interviews based on their expertise, experience, and willingness to share insights and opinions relevant to the study objective. The selection process included creating a list of national-, state-, and hospital-level stakeholders following a review of organizational hierarchy documents and consultation with EHR and health systems experts at national, state, and hospital levels. These experts were not included in the study sample. When conducting an interview-based study that has specific research questions, the experience of most qualitative researchers has been that little new information is generated after interviewing more than 20 people.16 Because purposive sampling focuses on identifying “information-rich” key informants, a total of 20 participants were purposively selected for the key informant interviews (KIIs).17
Data collection instrument
A KII guide in English and Hindi was developed and tested with three informants other than the key informants to ensure questions were aligned with the research objectives and appropriate to the study setting in addition to aligning the terms and concepts used in the guide with how it was used in practice. The KII guide was administered to gather information on the essential design and development requirements for an HDX. KIIs are appropriate for collecting detailed information from key informants with diverse backgrounds and opinions, and they allow for in-depth and probing questions.14 The interviews created a favorable environment for open conversations about sensitive topics in a one-on-one setting.
Data collection and analysis
The KIIs were conducted virtually between April and July 2020 using the Microsoft Skype application to call interviewees on the telephone. The interactive data analysis model of Miles and Huberman (1994) was adapted to guide the qualitative data analysis.18 The model describes analysis as three concurrent flows of activity: data condensation, data display, and conclusion drawing/verification. The three concurrent activities indicate that qualitative data analysis is a continuous, iterative process. The qualitative data analysis used a combination of deductive and inductive analysis; general inductive analysis predominated. The deductive analysis was guided by key themes identified from the research questions. Two researchers independently reviewed and coded the 20 KII transcripts and identified appropriate themes and discrepancies were addressed through weekly consultations. They were not limited by predefined themes. The first researcher was the investigator and the second had experience and expertise in conducting qualitative research in the Indian state of Uttarakhand. The final data analysis was conducted using NVIVO 12.0 software.
RESULTS
The study findings are presented under the following subsections: HDX model development process; HDX barriers and enablers; HDX model; HDX to support the use and reuse of data; HDX for efficient data collection and reporting; integration with registries for clinical care; and integration with research registries.
HDX model development process
Model development followed a systematic and iterative design process. The steps involved the review of available literature, an initial exploration with key informants, and in-depth qualitative data collection to develop and draft the HDX model. The draft model was presented for review and feedback to two key stakeholders during a one-to-one video conference meeting. One meeting was conducted with a former government national maternal and child health program expert. The second stakeholder was a senior hospital administrator who also had clinical responsibilities.
HDX barriers and enablers
The case study findings showed that the systems, processes, and stakeholder roles and responsibilities associated with data collection, storage, reporting, and use were unclear and fragmented. Multiple government programs, such as the National Health Mission, a national health program, Janani Suraksha Yojana (JSY)—a safe-motherhood program—and Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (PMJAY), a national health insurance program, were collecting data from the TSGH in parallel. Moreover, the findings revealed duplication of effort in the collection, storage, and sharing of individual and aggregate data in the hospital and with outside government agencies and departments. Patient health records were captured in disparate systems during registration, admission, billing, and transfer (RADT); in inpatient care coordination and procedures; and in external interactions with providers and other healthcare stakeholders. The current EHR system and processes added to the burden of the clinical and administrative workforce. Patient health records were used by clinical providers to plan and deliver healthcare services, and patient data were used by administrators, insurance providers, and financial incentive programs to track the delivery of services (including financial incentives) and to measure health program coverage across different population groups. The aggregated patient and administrative data were used for operational, administrative, policy, and program management decisions. The results highlight the importance of standardizing clinical workflows, defining minimum EHR data requirements, and establishing data collection, reporting and exchange standards. As one key informant (K 1) mentioned:
“I use data to determine the clinical, research, and teaching workload and deploy the staff accordingly.”
Affirming the benefit of EHRs for both patients and providers, one key informant (K 5) said:
“It will be easy for them and will be easy for us. So, patient will not have to carry health records all the time. If there is a concern from [an]other hospital, they can easily see what happened. If there is a complication in delivery and the patient comes to you after two years, you have the record to see what happened and how it was treated. If they do not come, they can take the record wherever they want to go.”
The findings showed that that many different types of data were collected during a patient’s interactions with clinical providers and other healthcare professionals in the hospital. Table 1 shows that the EHRs included information on patient demographics, diagnosis, problem lists, family history, allergies, immunizations, medications, procedures, laboratory data, vital signs, past medical history, radiology reports, and utilization. Social data, such as income level and education, were also captured because they confirm a patient’s eligibility for health insurance.
HDX model
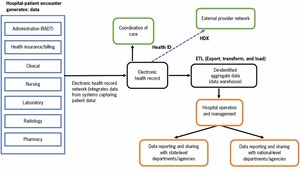
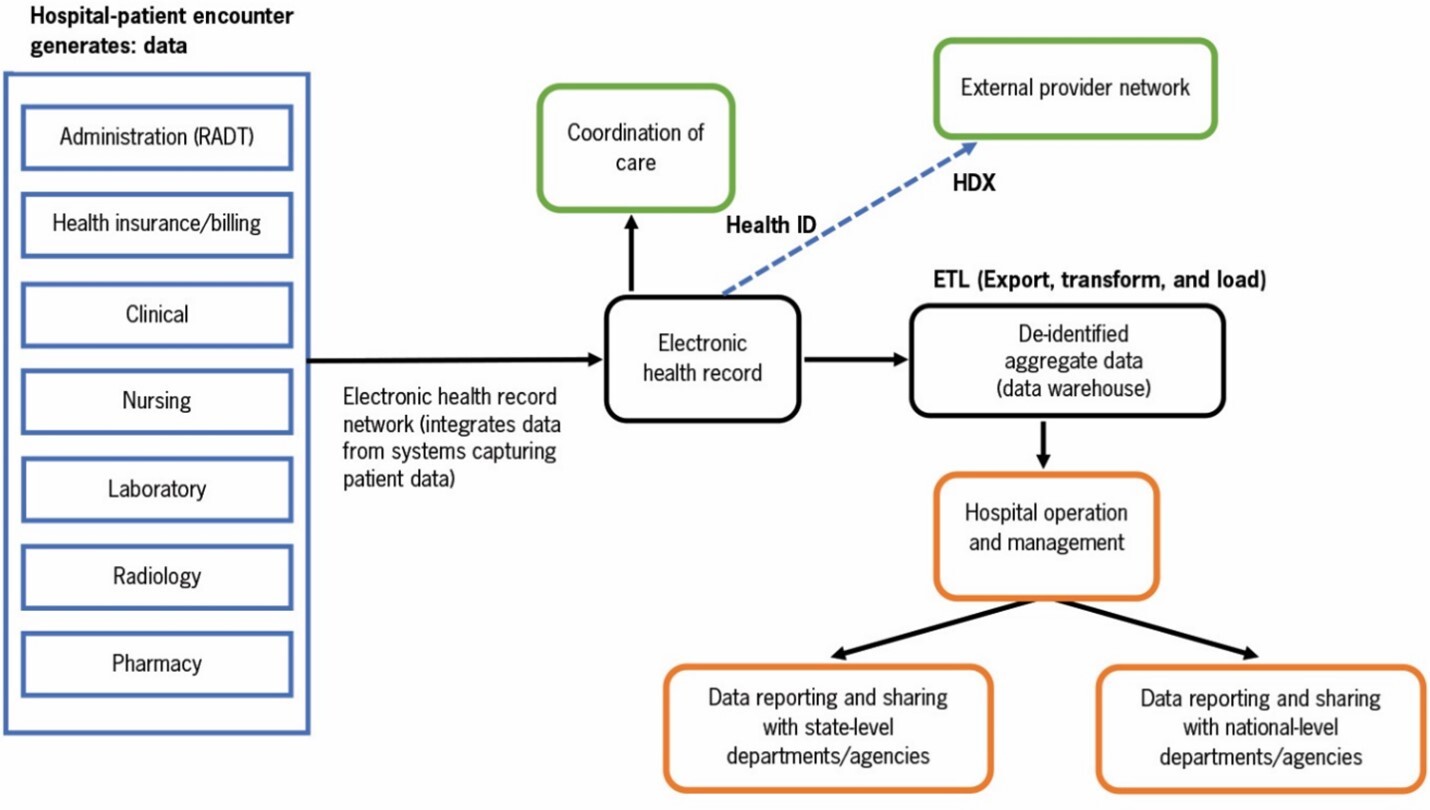
The model presented in Figure 2 shows how different workflows in the hospital can be connected through an EHR network to create an EHR for a patient by adopting and using standardization by design—from the beginning—as described in the Electronic Health Record (EHR) Standards for India (2016). As shown in Figure 2, the EHR network integrates data from administrative, billing, clinical, nursing, laboratory, pharmacy, and radiology systems in which patient data are captured. A key informant (K 8) said:
“So, the main thing is that the data are with us. We have all these data we can connect them. If you are patient 7273, all the labs that we have done, and CT-scan for that patient and other data are in our computers, we can connect them and the patient has the unique identification number, we can transfer them. We can do it systematically. So, for example, we start with pathology and then we start transferring the image in one system.”
The model also shows how de-identified aggregate data can be extracted from the EHRs using export, transform, and load (ETL) processes for reporting and different decision-making purposes in the hospital and at state and national levels. Aggregate data can be stored in a state-level data warehouse. In addition, the model shows how EHRs can be exchanged with other healthcare networks through a state HDX which is part of the national health information architecture. The HDX model discussed in this paper offers a bottom-up and user-centered (providers are the primary users) HDX development model. The hospital is the main focus, which can positively impact the adoption and use of EHRs. The model assumes that the EHR development process will adopt the standards recommended in the national EHR guidance document of India. The adoption of standards is critical for ensuring data quality, facilitating data harmonization and integration across different EHRs, and promoting the use of data for decision making. For example, Aadhar (Unique Identification) has become a de facto standard for accessing public services. A key informant (K 18) said:
“I mean everything in India, which has succeeded to any level, it has happened when the demand was created from [the] bottom. And I am not referring to iPhones. I am talking about Aadhar system. Why did I get my Aadhar done? Why should I stand in line and you will get this? One of this is benefits. The other one is that once I have Aadhar no more all this JHANJAT OF YE PAPER LAAO VO PAPER LAAO (trouble of bringing this paper and that paper document). I will just give my Aadhar ID, and I am done.”
HDX to support use and reuse of data
The HDX model is expected to facilitate the operationalization of the HDX vision proposed for the federated health information architecture of India. As a foundational component of the HDX, EHRs will enable the use of data for patient care and will support management and administrative decisions at the hospital, state, and national levels. Our findings show that interorganizational data exchange requirements were not well defined or well documented. They are often confounded with intraorganizational data exchange, which can result in report-led data collection and sharing rather than focusing on the use of data for decision making. The HDX model presents how to balance interorganizational and intraorganizational data exchange and the varying data use needs.
HDX for efficient data collection and reporting
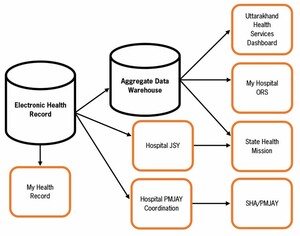
Figure 3 shows how the proposed interorganizational HDX can improve data collection and reporting efficiency, and enable patients to control and manage their health records. Data collected through patient encounters are accessed and used by hospital administrators, and by JSY and PMJAY teams. They also feed into the state health services dashboard, in addition to reporting to the state health agency and the state health mission. The EHR will allow individual patients to access their health records and store them in the MyHealth portal. Last, the hospital can allow patients to use the My Hospital Online Registration System (ORS) for scheduling appointments at the hospital once the TSGH completes the onboarding process.
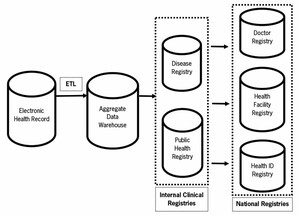
Integration with registries for clinical care
The findings highlight that the national government is working to create national registries, such as a doctor registry, a health facility registry, and a registry for unique health IDs. The model allows the linking, integration, and merging into relevant registries. In addition, the personal health records proposed under the National Digital Health Mission (NDHM), a national initiative to create the integrated digital health infrastructure of India, may leverage data contained in EHRs by integrating with the EHR to allow for real-time or near real-time data exchange, or by linking with the EHR to allow periodic transfers of data into the registries. The decision about whether and how to incorporate data from EHRs is complex and should be guided by many factors, including the purpose and scope of the registries and the availability of the necessary data elements in an EHR. The TSGH may also create internal registries for diseases and other public health purposes, which can leverage EHRs by deploying ETL processes. Figure 4 shows the proposed approach to integrating EHRs with internal and national registries to facilitate clinical care.
One of the shortcomings of this research was that the study did not focus on exploring and describing the perspectives of researchers and educators given the scope and time limitations. Therefore, use of EHR data for research did not emerge as an important theme. However, key informants did mention research because it is one of the responsibilities of clinicians who are involved in clinical research and practice, given that the hospital is associated with a medical college.
Highlighting the value of EHRs for research, a key informant (K 8) said:
“It takes more than a year for a resident doctor to collect data for research work, which is an important requirement of the post-graduate education. Availability of and access to electronic health data will make life easier.”
Integration with research registries
Figure 5 shows how EHR development at the TSGH can strengthen the use of clinical data for research purposes by facilitating the creation of a research registry. A research registry can harness available data systems for health insurance, drugs, and surveys (e.g., a national family and health survey), and it can integrate with lab and patient-generated data in the future.
To support the use of data captured in EHRs for clinical, administrative, and program management purposes, a health data governance framework is required. As one of the key informants (K 20) said:
“What we try to do before we digitize data, we created a legal framework for data privacy. So, we have drafted something called [the] digital information security bill. So, as per the act, the right of data resides with that person. So, if you are going to a hospital for consultation, lab test, etc., the data belong to that patient. Which means that if the hospital decides to do anything with the data other than providing care for that patient, it requires permission from the patient.”
The development of EHRs at the TSGH, and their potential implications for integration with research and clinical care registries, will be guided by appropriate data governance regulatory frameworks, such as the Digital Information Security in Health Care Act (DISHA) 2018. The purpose of the DISHA is to provide a regulatory framework for the generation, collection, storage, analysis, transmission, and ownership of patient health data and personally identifiable information. Once implemented, the DISHA will allow the extraction of data from EHRs for care coordination, program management, and research purposes in a safe and secure way.
DISCUSSION
Recent digital health strategy and guidance documents published by international organizations promote the adoption of digital health technologies, such as EHRs, to facilitate patient-centered care delivery and data exchange for program management and policy development.19,20 There is a global focus on the use and reuse of data, as highlighted in the World Bank’s World Development Report 2021. EHRs are one of the key pillars for achieving the vision of a national HDX that includes state- and facility-level HDX capacity. Although an effective and efficient electronic HDX is an important health system strengthening goal for most countries, there is wide variation in what countries have been able to achieve, especially in LMICs like India.21
The HDX model presented here shows how different workflows in hospitals can be connected through an EHR network to create an EHR for a patient. The EHR network can integrate patient data from administrative, billing, clinical, nursing, laboratory, pharmacy, and radiology systems. The model overcomes barriers associated with fragmented data collection systems and processes, care coordination, data quality, and access to patient health records. Moreover, it can reduce the data entry burden on hospital staff and enable clinical providers to plan and deliver healthcare services. The model also shows how de-identified aggregate data can be extracted from the EHR through ETL processes for reporting and different decision-making purposes in the hospital and at state and national levels. Aggregate data can be stored in a state-level data warehouse. In addition, the model presents how EHR data can be exchanged with other healthcare networks through a state-level HDX proposed in the federated health information architecture of India. The model allows the linking, integration, and merging into a registry because the NDHM has proposed the creation of a health ID, a doctor registry, and a facility registry. The personal health records proposed under the NDHM may leverage data contained in EHRs by integrating with the EHR network to allow for real-time or near real-time data exchange and by linking with the EHR network to allow the periodic transfers of data into the registry. The decision about whether and how to incorporate data from EHRs is complex and should be guided by many factors, including the purpose and scope of the registry and the availability of the necessary data elements in an EHR. The proposed model offers hospitals a focused EHR development model that can positively impact the adoption and use of EHRs by overcoming information system design barriers and contribute to improved data quality and data use.22
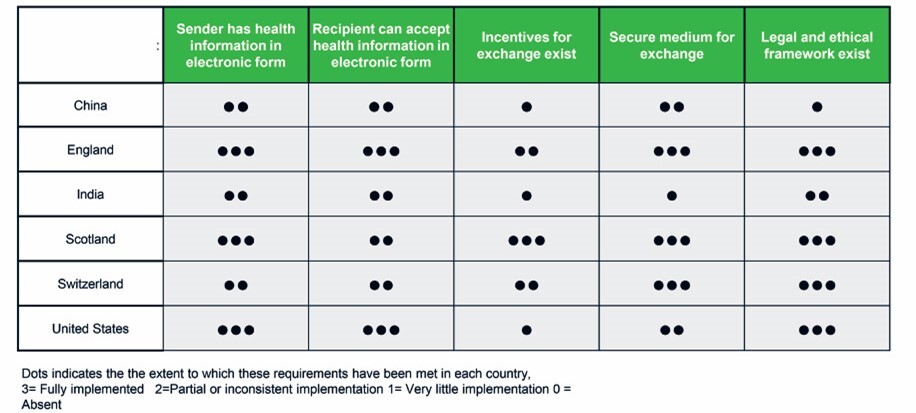
The study findings and the proposed HDX model fulfill the requirements for a health information exchange (HIE) outlined in a recent study,21 which compared the status of HIEs in six countries, including India. The study used exemplar HIE scenarios focusing on the transfer of care and referral, and mentioned that HIE requires electronic medical record systems or other systems to gather clinical information (at both the point of capture and at the recipient organizations), incentives, secure networks for HIE, and appropriate policy and regulatory environments. The study showed that India had partial or inconsistent implementation of systems and processes for capturing and sharing health information, legal and ethical frameworks, and that it had only minimally implemented incentives and secure networks for electronic HIE (Figure 6). Although the HDX model fulfills the requirements for an HIE, it is important to highlight that tertiary care hospitals in a state and across the states vary in their technical and financial capacity, healthcare priorities, patient demography and socioeconomic status, and data use cultures.23 The HDX implementation framework must address organizational, technological, cultural, social, economic, and political dimensions, which often drive or hamper the development, use, and governance of EHRs and HDX.24
The findings of our study are aligned with research studies that emphasize the importance of robust processes to generate functional requirements to design, deploy, and evaluate systems; functional issues are at the core of the success or failure of electronic medical record systems.24,25 Moreover, the proposed model showcases how to apply the principles of federated architecture, which requires that health data and applications at the state level hold patient data at the point of care in a system of record, and is reliant on state-level data fiduciaries and the exchange of health information through links with the facility and national levels.8
CONCLUSIONS
As India continues to expand its digital heath infrastructure to facilitate inter-organizational health data exchange, the development and implementation of an HDX must build efficiency in data management and support the use of data for quality healthcare delivery and continuous program improvement. The continuous quality improvement in patient care and programs will depend on how EHRs are understood, designed, governed, and scaled in the national HDX. Therefore, aligning EHR development strategies around a common HDX framework, as exemplified by the NDHB of India, will be valuable because it offers policy and financial incentives to achieve the goal of inter-organizational HDX at national, state, and facility levels. The results will also enable researchers to validate and/or modify the model when developing inter-organizational HDX and will guide future research in this domain.
Acknowledgments
The authors are thankful to the Ph.D. dissertation committee members for their guidance, support, and constructive feedback throughout the research study.
Funding
The study did not receive any funding.
Authorship contributions
The authors contributed substantially to the study, from conception and design through its conclusion. Their contributions include analysis and review of the resulting data, and the composition and critical review of the article to ensure the integrity of its intellectual content. The authors have provided final approval of the manuscript to be submitted.
Competing interests
The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author) and declare no competing or conflicts of interest with this study.
Correspondence to:
Manish Kumar, Ph.D.
Carolina Population Center | University of North Carolina-Chapel Hill
123 W Franklin St, Suite 330, 3rd Floor, Chapel Hill, North Carolina, United States of America 27516
Email: [email protected]