Back pain (BP) and musculoskeletal pain (MSP) are the commonest causes of long term pain, disability and health care expenditure world over.1–3 They are an important cause of loss of productivity, with back pain alone causing an estimated loss of 800,000 Disability Adjusted Life Years (DALY) globally every year4 and a substantial number of visits to health care providers, adding to the economic burden on individual and health systems.5 As musculoskeletal conditions are the commonest cause of chronic disability globally, 2000–10 was recognized as the Bone and Joint Decade by the World Health Organization.6
Heavy physical work is a known risk factor for pain in the back and extremities (PBE),7 and hence rural agrarian communities are at high risk of PBE.8–10 In a country like India, where a majority of the population lives in rural areas11 and depends on physical labour for their livelihood, the high prevalence of PBE, apart from causing suffering, might be resulting in a significant hidden economic burden too. This may happen by way of the cost of medical care for PBE and the loss of wages due to the work-days lost. However, there are no population-based studies from rural India estimating the economic burden of PBE.
We aimed to estimate the economic burden of PBE over 12 months including the cost due to work-days lost, medical consultation, and purchasing medications among adults (≥ 20 years of age) in rural Gadchiroli.
Methods
Study setting and study population
The study was conducted in rural Gadchiroli in India. Gadchiroli district is situated on the eastern border of Maharashtra state. 30% of the district’s population lives below the poverty line making it one of the poorest and least developed districts in India.12 The Human Development Index (HDI) for this district was the lowest in the state, at 0.21, as compared to the HDI of 0.58 for the state of Maharashtra and 1 for the city of Mumbai.13 The district is heavily forested (79%) and the main source of livelihood is paddy cultivation and collection of forest produce.14 The district has 38% tribal population. The adult literacy rate is 70%. Health care is provided primarily through the public health system comprising 1 district hospital, 3 sub-district hospitals, 9 community health centers (CHC), 45 primary health centers (PHC) and 376 sub-centers (SC).15 In addition, traditional healers, unregistered doctors, private registered practitioners and a few non-government organizations also provide health care.
Society for Education, Action and Research in Community Health (SEARCH) is a non-governmental organization that has been working in Gadchiroli district since 1986. It has a field practice area of 86 villages, in which community health workers (CHWs) regularly collect population-based information and provide health care for selected ailments to the villagers.16
Study design and sample
This study of economic burden was nested in a population-based, cross-sectional, interview-based survey of the prevalence of PBE in rural Gadchiroli. The primary outcome for sample size estimation of the main study was point prevalence of non-specific low back pain in adults (≥20 years of age), based on which a sample of a minimum of 1800 adults was calculated.
We conducted this study in 2 agrarian villages, selected from the 39 villages in the Gadchiroli block by a two-stage procedure. First, villages were identified by applying certain eligibility criteria. The aim was to include typical Indian villages of medium size (population 1200 to 2000), not very near urban areas (>5 km), without a PHC located in them, and where a house-to-house survey was feasible by the presence of male and female CHWs of SEARCH. Based on these criteria, 7 villages were first identified as eligible villages from the 39 villages. From these, villages were randomly selected till the required sample size (1800 adults) was met. Two villages (Mudza and Bamhani) were thus selected. The study population consisted of all the resident adults (age ≥20 years) from these two villages, as recorded in the population register with the CHWs, recruited through household survey by the CHWs.
Study implementation and assessment of the economic cost of PBE
Questionnaire development
A standardized questionnaire in the local language (Marathi) was developed to interview participants and record the following information about the immediate past 12 months from January 2009 to January 2010: (i) episode of PBE, (ii) intensity of pain, (iii) whether treatment was sought for the pain, (iv) whether medical consultation was sought from a provider, (v) expenditure on medical consultation, (vi) expenditure on purchasing medications, (vi) whether occupational work had to be stopped, and (viii) the number of work-days lost due to pain. This questionnaire was pilot-tested in the rural clinic of SEARCH and in other villages, and modified appropriately before use in the survey.
Training and quality control
The male and female CHWs (four) from the two selected villages and the four supervisors of SEARCH were trained for 3 days by a training team consisting of a physician (AAB), statistician (MD) and public health researcher (TY) using standard guidelines in administering the questionnaire and recording. The supervisors were additionally trained for 2 days in using check-lists for field data quality control and supervision. The CHWs and supervisors were rigorously evaluated and allowed to participate in the study only when they scored >85% in the post-training evaluation. Any mistakes noted during evaluation were rectified by re-training the CHWs.
Data collection
As a nested part of the main study to estimate the period prevalence of PBE, we collected data from 1st January 2010 to 25th January 2010. Using the updated population register of SEARCH and unique identification numbers given to every resident in the village, a list of all the participants from the selected villages was generated. Male and female CHWs conducted a door-to-door survey and collected data using the study questionnaire in a face-to-face interview from the eligible male and female participants. During data collection, the supervisors checked the quality and completeness of each filled questionnaire using a data quality check-list. Questionnaires with incomplete information were returned back to the CHWs to collect the missing information.
We classified pain in the back and extremities as acute if the pain duration was up to 42 days (6 weeks), sub-acute if the pain was for 43 days to 84 days (>6 weeks to 12 weeks), and chronic if the pain was for more than 84 days (>12 weeks).17
The information on the money spent excluded the cost of travel or diagnostics. Similarly, the information provided by the participants was not verified from the documents due to unavailability of the same. The work-days lost were recorded but not the nature of the work. The days lost were recorded as full days. The information about the expenditure on two Central Government schemes in the district, the National Rural Health Mission (NRHM) and the National Rural Employment Guarantee Scheme (NREGS), was obtained through personal communication from the concerned district officers from the Revenue Headquarter and Health Division of the Zilla Parishad (District Council) of Gadchiroli.
Statistical methods
A database was constructed using Fox Pro Version 2.0. The data were double-entered and inconsistencies were checked. Descriptive statistics including means were estimated with range for continuous variables and with the associated 95% confidence intervals (CI). Student’s t-test was used to assess difference between group means after checking for normality. Differences between percentages were assessed using Chi-squared test. We used two-sided tests with a significance level of 5%. We performed multivariate analysis using an ordinal logistic regression model for days of work lost due to PBE and out-of-pocket expenditure by appropriate categorization, as both the outcomes did not follow a normal distribution but did have a natural ordering. Analyses were conducted using Stata 10.0 (StataCorp, College Station, Texas, USA).
Ethics approval
The research followed the tenets of the Declaration of Helsinki. Ethics approval for this nested study was granted as part of the main study, by the institutional ethical committee of SEARCH formed according to the guidelines by the Indian Council for Medical Research. Consent was obtained first at the cluster level in the study villages 15 days before starting the survey. The purpose and scope of the study, including the benefits to the villagers (availability of referral care at the SEARCH clinic and care through a village clinic), were explained to community leaders (village council members and leaders, school teachers, and presidents of microfinance self-help groups). Informed written consent in the vernacular language in a standard format was obtained from individual participants after explaining the nature and benefits of the study. The benefits provided during the study included free consultation by spine surgeons and rheumatologists in a clinic conducted in the same village at a later date. For those who needed further evaluation, laboratory investigations, as well as imaging with magnetic resonance imaging (MRI) and X-ray including transport were provided free of cost. For patients needing pharmacotherapy and physiotherapy, these services were also provided free of cost, and for those needing surgical interventions, such services were provided at significantly subsidized costs. The CHWs discussed these benefits using a printed pamphlet.
Results
Study design and sampled population
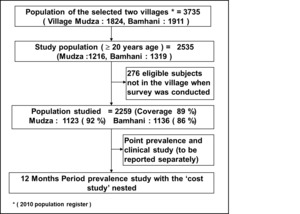
The total population of the two villages was 3735 (1824 in Mudza and 1911 in Bamhani) out of which 2535 (67.9%) were adults ≥20 years of age (1216 in Mudza and 1319 in Bamhani) and were eligible to participate in the study. Of these, 2259 (89%) were interviewed, while 276 (11%) were either absent from the village (migrated for work) or unable to communicate due to very old age or disability. The response rate was higher in Mudza (92%) than Bamhani (86%), and for women (91.3%) than men (87.5%). See Figure 1 and Table 1.
The age, caste, education and occupation distribution of the population studied are presented in table 1. The mean age of the participants was 41.7 years (standard deviation, SD 15.6). 51% of the study participants were women. The primary occupations were farming and farm labour (78%). While about 70% of the study participants were literate, only 10% of the participants had schooling beyond 10 years.
Of the 2259 individuals screened, 1876 had an episode of musculoskeletal back and/or extremity pain in the preceding 12 months, giving an overall 12-month period prevalence of 83% (95% CI=82-85). The 12-month period prevalence of back (including lower back, thoracic and neck) pain was 76% (95% CI=74–78), and that of extremity pain was 71% (95% CI=69–73).
In a year, the mean duration of BP was 171 (95% CI=165–178) days per symptomatic individual and 142 (95% CI=136–149) days in the total study population. Any extremity pain was present for a mean 144 (95% CI=137–151) days in symptomatic individuals and for 120 (95% CI=114–126) days in the total population studied. The mean duration of any pain in back and/or extremity in the 12-month study period was 166 (95% CI=160–173) days. The pain was chronic in 48% individuals with back pain, in 41% of the individuals with pain in the extremities, and in 55% of individuals with pain in back and/or extremities.
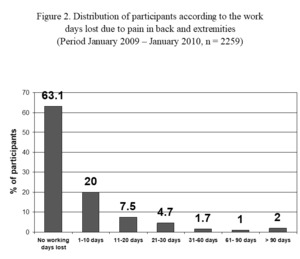
Distribution of participants according to work-days lost due to PBE in 12 months
Of the study participants (2259), 833 (37.9%) had to stop their occupational work at some time during the preceding 12-month period. Out of these, 45 (2%) participants stopped work for more than three months, 60 (2.7%) stopped work for 1 month to 3 months, 728 (32.2%) stopped work for up to 1 month and 451 (20%) lost 1 to 10 days due to pain. The total work-days lost over the 12-month period due to any pain were 24,205. The mean work-days lost due to pain were 11 per participant (Figure 2).
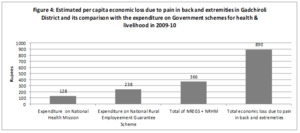
Distribution of participants according to amount of money spent on treatment for pain in back and extremities in 12 months
The money spent on medical treatment is presented in Table 2. Of the total participants, 17% did not have pain and 287 (13%) did not spend any money on either medical consultation or purchasing medications despite pain. 62% participants spent between 1 to 1000 INR and 8.5% spent more than 1000 INR (Figure 3).
Cost of medical treatment and ttotal economic cost of pain in back and extremities in two villages in 12-months (2009-10)
Of the study participants, 617 (27%) sought medical consultation (fees of the care giver) from a health care provider and 1535 purchased medications, either as prescribed by the health care provider or purchased over the counter (Table 3). The medications were generally analgesics, massage oils, liniments and ointments. Overall, 70% of the study participants either sought medical consultation or purchased medications. The total expenditure on medical consultation for pain over 12 months was 62,880 INR and on medications was 8,55,203 INR. Total expenditure for PBE on medical care was 9,18,083 INR in the two villages. The cost of medical expenditure per capita (adult study participant) over 12 months was 379 INR.
The minimum daily wages in year 2009–10 according to the guidelines by the Government of India under the NREGS, a program providing cash for manual labour was 100 INR per day.18 At this rate, the estimated total wages lost were 24,20,500 INR in 12 months, or 1100 INR per adult in the study population.
The total economic cost borne by the study population due to PBE was sum total of the out-of-pocket medical care cost and the indirect cost of wages lost due to inability to work. Based on this, the cost of PBE for 2 villages over 12-months was 33,38,583 INR or 1317 INR per adult participant, and 1789 INR ($36.94) per symptomatic adult, which was 4.9% of the annual per capita income of 36,286 INR for Gadchiroli in 2009-10.19
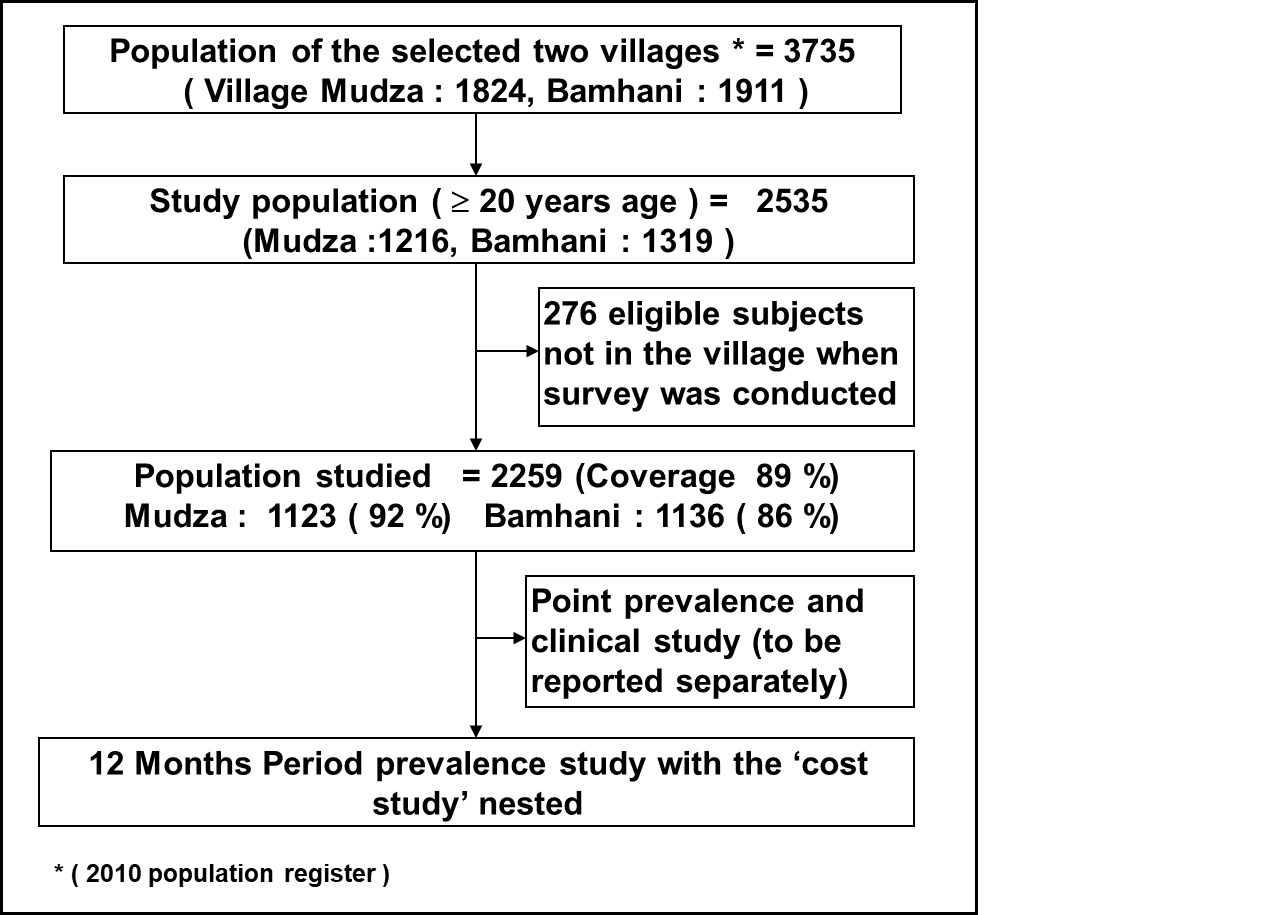
Per capita economic loss due to pain in back and extremities compared with the per capita government’s spending on national schemes for health and livelihood
The population of Gadchiroli district was 9,700,294 according to the 2001 Census.20 The annual population growth rate of Maharashtra was 2.1%.19 Assuming the annual population growth rate of only 1.5%, the conservative estimate of the projected population of Gadchiroli district in 2009 was 1.09 million. The expenditure in the district in 2009–10 on the national scheme by the Central Government to improve health under the NRHM and increase the income by providing livelihood through manual labour work under the NREGS was 13,98,85,000 INR (139 million INR) and 25,92,10,000 INR (259 million INR) respectively.21,22 The total expenditure on these 2 schemes was 39,90,95,000 INR (399 million INR). Hence, the per capita expenditure on NREGS was 238 INR ($4.91), on NRHM was 128 INR ($2.64) and the combined per capita expenditure was 366 INR ($7.56). Hence the estimated annual economic loss due to PBE by the population of Gadchiroli was 2.36 times more than the combined annual (2009-10) expenditure on schemes to improve health and provide livelihood by the Government (Figure 4).
Factors associated with Days Lost at Work due to PBE and out-of-pocket expenditure (table 4 and 5)
We categorized the days of work lost due to PBE as no days lost, 1-15 days lost, and more than 15 days lost. Women were 1.38 times more likely to lose more days at work due to PBE compared to men. Compared to the participants with education of more than 10 years, illiterates were 1.78 times, participants with education of 1-4 years 2.24 times and those with education of 5-7 years were 1.94 times more likely to lose work-days due to PBE. Compared to the youngest age group of 20-30 years, participants aged 31-40 years, 41-50 years, 51-60 years and more than 60 years were 1.35 times, 1.64 times, 1.84 times and 2.45 times more likely to lose more work-days respectively. Compared to the participants with occupations of business or salaried jobs, farmers were 1.56 times more likely to lose work-days due to PBE.
We categorized the out-of-pocket expenditure on treatment of PBE (in INR) as 0, 1-100, 101-200, 201-300, 301-400, 401-500, 501-1000, 1001-2000 and >2000. As in the case of work-days lost due to PBE, women were 1.57 times more likely to have more out-of-pocket expenditure on treatment of PBE than men. Similarly, compared to the participants aged 20-30 years, participants with ages 31-40, 41-50, 51-60 and more than 60 years were respectively 1.54, 2.03, 2.83, and 3.52 times more likely to have higher out-of-pocket expenditure on treatment of PBE. Another factor significantly associated with out-of-pocket expenditure was caste, with Scheduled Castes (SCs) 27% less likely to spend compared to participants from other castes.
Discussion
This cost of illness study, conducted in two villages in Gadchiroli found that 83% of the adult population suffered back and extremity pain at some time or the other in a period of 12 months. Out of these, 27% participants sought medical consultation for pain relief spending 62,880 INR, and a higher proportion, 68% purchased medications, spending 337 INR per adult in the population annually. A considerable proportion of the participants (37%) had to stop work due to pain. The 24,205 work-days lost over 12 months, or the 11 work-days lost per adult participant, caused enormous economic and productivity losses. The total cost of PBE was 33,38,583 INR or 1506 INR per adult participant.
Many studies have estimated the direct and indirect costs associated with back pain and musculoskeletal pain in developed countries and are found to be a substantial burden on society.23 In the United States (US), all forms of musculoskeletal conditions lead to a combined medical care expenditures of about US$240 billion, or about 2.9% of Gross Domestic Product (GDP).7 Low back pain alone is one of the top ten physical and mental health conditions affecting US employers in 19998 with the total direct and indirect costs of low back pain around $24 billion per year.9 Similarly, in the United Kingdom (UK) the total estimated cost of back pain is ₤12.3 billion,10 while in the Netherlands it is €3.5 billion, or 0.6% of the Gross National Product (GNP) in 2007.24 Overall, the economic impact of pain is enormous and according to a study, the cost of back pain alone is equivalent to more than one-fifth of a country’s total health expenditure and 1.5% of its annual GDP.21
To the best of our knowledge, this is the first population-based study from rural India involving an agrarian community which has systematically estimated the private spending on PBE for medical care, the work-days lost due to PBE, and the resulting economic loss.
The average annual economic loss due to PBE per symptomatic participant in this study was 1789 INR. Given the annual per capita income for the district of Gadchiroli estimated at 36,286 INR in 2009-10,19 a person with PBE lost about 4.9% of the annual per capita income due to PBE.
In a predominantly rural and backward society, the proportional economic loss due to PBE could be higher due to the lower per capita income and possibly higher prevalence of PBE compared to the urban setting.
Importantly though, the indirect cost contributed a larger fraction (72.5%) of the total economic burden than the direct cost per adult (Figure S1). This corroborates many other studies and systematic reviews done in the developed countries, where the indirect cost due to informal care and work-days lost constituted around 84% to 88% of the total economic loss.10,22,24 Considering the high prevalence of PBE in rural population such as ours, the negative economic impact of BP and MSP is likely to be disproportionately more, resulting in a worsening of poverty.
Interestingly, the expenditure by the studied population on purchasing medications (8,55,203 INR) was more than 13 times that on the fees of health care providers (62,880 INR), underlining the high out-of-pocket expenditure on purchasing medicines in India.25 Nevertheless, the expenditure on medical consultation may increase if various diagnostic and imaging facilities as well as physiotherapy and occupational therapy, which were completely absent in the study villages, were to be made available by the private sector in villages, or people had access to such services in the nearest towns.
The association of older age groups and female sex with more work-days lost due to PBE, as well as higher out-of-pocket expenditure on treatment of PBE, may be due to difference between the comparative physical resilience of men and women as well as between younger and older age groups. Farmers experiencing more work-days loss and higher out-of-pocket expenditure compared to participants with occupations involving no manual labour, especially those involved in business or salaried jobs, would be due to the effect of manual labour, which is an integral part of the farmer’s work. Why the out-of-pocket expenditure does not change across different educational levels or jobs needs further exploration, as well as why SCs have a lower probability of out-of-pocket expenditure on treating PBE than other castes.
The study had several strengths, which lend confidence to the estimates obtained. The two study villages were randomly selected from a list of villages after excluding atypical (too large, too small, periurban, with PHC) villages. Most of adults in the villages were recruited, with high overall coverage (89%). Information bias was also unlikely, as data collection was done by experienced CHWs using a well pre-tested and structured questionnaire. The sample size was quite adequate for estimating the economic burden, as revealed by the narrow CI of the estimated costs.
The limitations are that Gadchiroli is a poor district and may not be representative of the other district in the Maharashtra State. Similarly, the selected villages excluded some categories of villages (as described in the inclusion and exclusion criteria) and hence the results may be limited to certain types of communities. A possibility of recall bias for the duration of pains, work-days lost and the actual amount of expenditure over 12 months cannot be ruled out. The other limitation is the complete dependence on self-reported information by the participants and inability to verify the expenditure from the bills of medicines purchased due to unavailability of the same in the rural setting. Similarly, the villages where the study was conducted had male and female CHWs providing subsidized treatment for pains with aspirin tablets for the past 20 years. This might reduce the duration of episodes of pain due to better availability of painkillers as compared to other villages, and reduce the work-days lost as well as the cost of treatment. Also, indirect costs due to loss of wages of relatives, loss of wages due to inability to perform household work in women, and expenditures due to reduced duration/quality of work leading to economic losses, were not included, but an argument can be made that we would have thus underestimated the costs.
Though this study was conducted in rural Gadchiroli, the findings of this study may reflect the situation in many rural agrarian communities considering the similar overall socioeconomic and work profile. Nevertheless, we suggest that more population-based studies should be conducted in different parts of rural India, possibly employing larger sample sizes, to identify the regional estimates and any differences in the estimates of medical cost and work-days lost. The distribution of the cost of medical consultation amongst different health care providers such as private doctors, public health care centres and informal providers should also be studied. If only a certain section of the symptomatic population was responsible for a substantial fraction of the economic loss, as in one study,26 the intervention strategy can be more specifically designed.
Conclusions
In conclusion, this study found a significant economic burden due to PBE in a rural community in Gadchiroli, which is likely to be a problem in other rural societies involved in manual labour. The economic loss, equal to 4.9% of annual per capita income can contribute to worsening of poverty and adverse health consequences. PBE appears to be a public health priority, which needs prevention as well as pain relief for reducing out-of-pocket expenditure. Increasing the availability of generic analgesics, physiotherapy, and occupational therapy in the community to reduce the work-days lost may be attempted. It may improve the economic status as well as the health of the population.
Acknowledgements
We thank the study participants, community health workers, volunteers and leaders of the village Mudza and Bamhani who participated in the study and made all the arrangements. We thank the community health workers of SEARCH. We thank Dr. Rani Bang, SEARCH, Gadchiroli for her support in conducting the study and conceiving the idea. We thank Dr Yogesh Kalkonde for comments on the manuscript.
Funding
The study was funded by Sir Dorabji Tata Trust, the Spine Foundation, Mumbai, and SEARCH, Gadchiroli, India
Authorship contributions
Conceived and designed the study: AAB, ATB, SYB, SK, MD, VRJ. Conducted the study: AAB, MD, TY, ATB. Analyzed the data: MD, AAB, ATB. Contributed materials / analysis tools: ATB, SYB, SK, VRJ. Wrote the draft manuscript: AAB. Reviewed the manuscript: ATB.
Competing interests
The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf, and declare no conflicts of interest.
Correspondence to:
Dr. Abhay Bang, MD, M.P.H.
Director, SEARCH, Shodhgram, PO Gadchiroli, Maharashtra, India 422605;
[email protected]