In early December 2019, pneumonia with an unknown etiology was reported among a cluster of patients in a hospital in Wuhan, Hubei Province, China.1 One month later, the World Health Organization (WHO) declared COVID-19, the disease caused by a novel coronavirus (SARS-CoV-2), a Public Health Emergency of International Concern.2 After realization of the rapidly increasing number of confirmed cases and the growing number of affected countries, COVID-19 was declared a global pandemic on 11th March 2020.3 By 19th July, there were more than 14 million confirmed cases and near 600 thousand deaths reported globally.4 The United Stated of America and Europe were most affected, reporting around 7.3 million deaths and more than 3 million cases which accounted for nearly three quarters of the total cases globally.4
Vietnam was among the first countries to be affected by the virus, however, the country responded promptly in order to gain early control of the COVID-19 epidemic. The first two cases reported in the country were two Chinese men who had traveled from Wuhan on 23rd January.5,6 Subsequently, the number of confirmed cases in Vietnam increased steadily, and by 30th June, the nation had recorded 355 cases without a single lethal outcome; 325 patients recovered completely and were discharged from hospitals.7 As a final result, Vietnam, a low-income country, has been internationally recognized for its effective control measures which resulted in zero deaths and 99 uninterrupted days without a single community case by 19th July.7
Currently, information about the COVID-19 outbreak and control measures in Vietnam is available in various governmental websites, local newspapers and experts’ analyses. To the best of our knowledge, a limited number of academic papers discussed the spread and management of COVID-19 in Vietnam. Of these articles, some published reviews highlighted that an early response, governmental preparedness, strong political figures, the operational readiness of grassroots health system and roles of social media all contributed substantially to the successful control of COVID-19 in Vietnam.8–11 However, there has been little discussion of the details of these policies and how they have been implemented systematically. This is important as it may provide some insight for other countries.8–11
How society-wide approach and systemic response is achieved in a centralized government like Vietnam remains unclear. Some studies overlook the importance of the Vietnamese health system’s infection prevention and control measures when discussing control of the outbreak. Of further importance is an understanding of how a lower-middle-income country with limited resources such as Vietnam was able to effectively manage the outbreak that cost thousands of lives in many developed countries.
This paper aims to overview the key Vietnamese state-led responses for controlling the COVID-19 pandemic in the context of social structure, politics and the public health system. This analysis will inform the general public, public health experts and policymakers about contextualized responses to a global health crisis and discuss valuable lessons learned for future reference. Specifically, this study uses the WHO’s strategic response plan that was released on 14th April as a framework to analyze Vietnam’s responses and policies during the first wave of the pandemic (up to 19th July).12
This paper begins with a review on the context of the COVID-19 outbreak in Vietnam, followed by the analysis of the governmental response, and finally concludes with a discussion of how the responses contributed to containing the spread of the disease both domestically and globally.
Methods
This paper is a narrative review of Vietnam’s policy response to COVID-19. We reviewed the governmental documents and technical guidelines issued by the state government and the Ministry of Health (MoH), a national body responsible for the management and coordination of COVID-19 related activities . Documents including a timeline of the spread of COVID-19 within Vietnam were digitally collected. The inclusion criteria for this review were COVID-19 policy response letters or technical guidelines issued by the Prime Minister, the Ministry of Health and other ministries where relevant between December 2019 to 19th July.
Official COVID-19 response documents issued by local governments, academic articles, official reports from technical agencies and official newspapers’ articles were used to provide insight into the country’s outbreak, and to illustrate how policies were implemented. Vietnam’s COVID-19 statistics provided in this paper were collected from the website of the General Department of Preventative Medicine, the Ministry of Health (https://ncov.vncdc.gov.vn/).
This paper excludes articles from non-official websites and social media posts. Additionally, we did not provide a detailed discussion of policy implementation or economic COVID-19 relief packages.
This paper uses the WHO’s updated strategic response plan, released on 14th April, as a framework from which to analyze responses and policies. The framework comprises of five sections: (1) coordination and planning, (2) engagement and mobilization of communities to limit exposure, (3) implementation of context-appropriate public health measures, (4) provision of clinical care and maintenance of essential health services to reduce mortality and (5) adapting strategies based on risk, capacity and vulnerability. The Vietnamese government’s COVID-19 response policies were first selected and then analyzed. As this study was a review of publicly available reports and studies, no additional ethical approval was sought.
Results
An overview of the COVID-19 situation in Vietnam
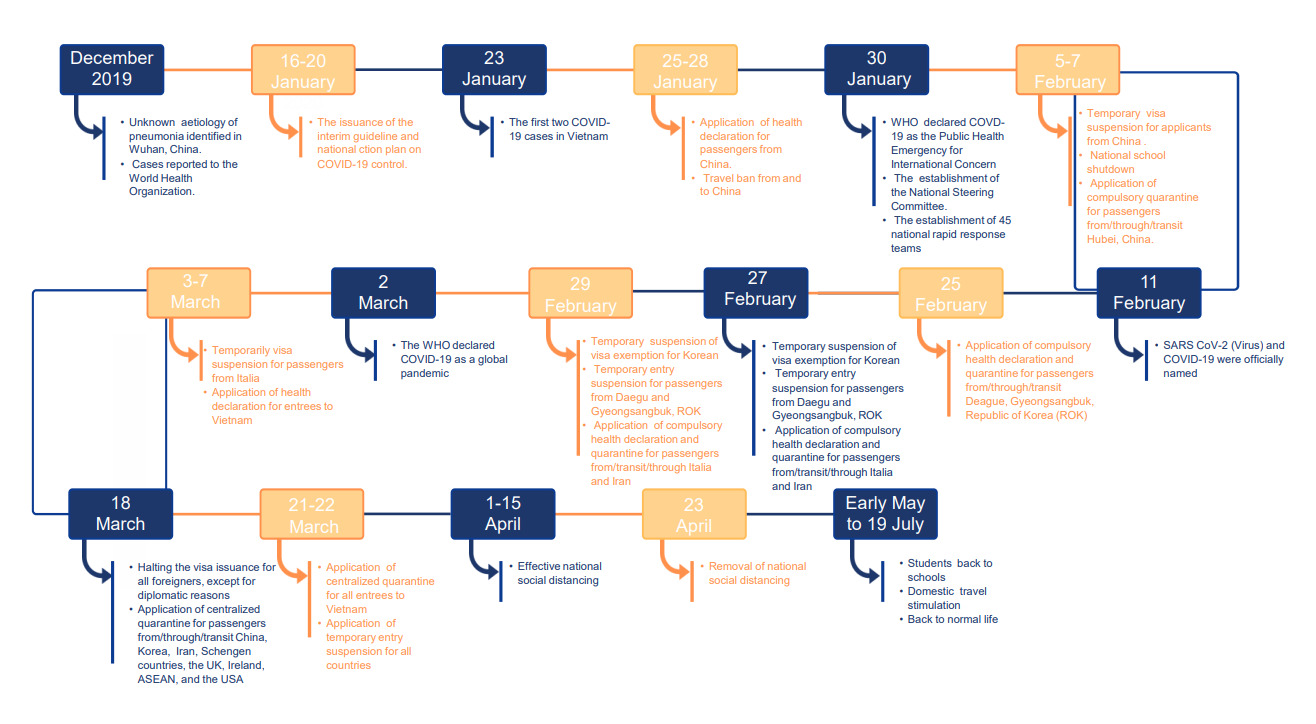
Vietnam has a GDP of approximately USD 2,700 per capita. Total health expenditure was estimated at approximately 6.6% of the total GDPand up to 31.3% of health care costs are out-of-pocket.13–15 Vietnam is one of the five countries including Japan, the Republic of Korea, Thailand and the United States of America (USA) where COVID-19 cases were first confirmed outside of China; however, Vietnam was fast to implement impressive and effective control measures against COVID-19.16 The first two cases in Vietnam were identified on 23rd January. By the end of the first wave of the pandemic (19th July), Vietnam declared that 70.1% of cases were imported and there had been no fatalities.7 A summary of the distribution of COVID-19 cases across the country by 30th June is presented in Figure 1. The majority of cases were concentrated in the two largest cities – Ha Noi and Ho Chi Minh. The first wave of the pandemic can be temporarily divided into three sub-stages: epidemiological linkage, the government responses and the presence of community transmission cases (Figure 2).
The first stage of the first wave began when the first case was declared and lasted until 6th March. This stage reflects patients who were epidemiologically linked to Wuhan, China (16/16 cases), of which 50% were imported cases.7 On 1st February, the Prime Minister announced the outbreak following the first recorded occurrence of local transmission in Vietnam. The country immediately deployed tight measures against the pandemic including travel restrictions and bans, visa suspensions, compulsory quarantine and health declarations for heavily affected countries (China, Republic of Korea, Iran and Italy), as well as a nationwide school shutdown.17–19 From 14th February to 6th March, there were no recorded cases.7 Consequently, the government began to stimulate international tourism from countries less affected by COVID-19, and Vietnamese citizens living abroad were repatriated. However, a lapse in COVID-19 control caused by poor screening of potentially ill travelers from less-affected countries sparked an infection in a hospital, which led to the second stage of the COVID-19 outbreak.
The second stage of the outbreak was from 7th March to 22nd April, when new cases were linked to a history of visiting, transitioning or returning from Europe, the USA and the Republic of Korea.20 A total of 252 cases over 22 provinces and cities were reported, of which 154 were imported cases (61.1%).7 This time, the state deployed even stricter responses including border shutdown, an international travel ban to all countries, domestic travel restrictions, compulsory facemask use and national social distancing at work and public places. The Prime Minister declared the nationwide COVID-19 pandemic on 1st April.21 According to the WHO’s classification on COVID-19 transmission, Vietnam was classified as clusters of COVID-19 cases. Public health measures, therefore, were to “slow transmission and prevent the spread”.22
The third stage of the outbreak was from 23rd April until 19th July when Vietnam managed to control the COVID-19 pandemic by eliminating community transmission. In this period, all cases (116) were imported and there were no deaths reported. The country gradually returned to normal as the strict regulations and curfews including social distancing, lockdown and domestic travel restrictions were lifted. The country re-opened the internal economy by the end of April 2020 (Figure 3).
The Vietnamese government responses to COVID-19
Coordination of national and sub-national responses
The Vietnamese government provided strong leadership in response to COVID-19 by establishing the National Steering Committee (NSC) led by Deputy Prime Minister – Vu Duc Dam. The NSC is a multi-ministerial and multisectoral committee, established on 30th January – within a week of the first few cases being reported.23 The committee works to direct pandemic control and assessment on behalf of the government. The presence of key ministers and parties in the NSC enables it to make crucial decisions and systemically coordinate the implementation of containment measures. At local levels, 63 provincial and 707 district steering committees were established.
The Prime Minister promulgated the first Directive (No. 05/CT-TTg) on COVID-19 prevention and responses when Vietnam had only two imported COVID-19 cases. Importantly, the government initially chose a multi-sectoral approach and systemic response with careful risk assessment.5 Given that China and Vietnam share a long border and have a high flow of daily traffic, this initial step dramatically helped to control the potential spread of the virus to Vietnam. Further, to curb the local transmission, Vietnam immediately ordered rigid contact tracing and quarantine, cancellation of tours to and from COVID-19 affected regions and tight monitoring of incomers at all points of entry.5 By 30th June, seven Directives on COVID-19 prevention and control (No. 05, 06, 11, 13, 15, 16 and 19/CT-TTg in sequence) were issued in alignment with the COVID-19 situation within the country.
The MoH is the key player in the effort to coordinate COVID-19 containment measures among its sub-agencies and other ministries. It provides technical guidelines for prevention, treatment, surveillance and monitoring. The coordination of activities is mainly through official guidelines, letters or meetings led by the NSC. Noticeably, the MoH issued the first national interim guidelines for the diagnosis and treatment of COVID-19, and the national response plan with the four-plus COVID-19 response scenarios when Vietnam had no COVID-19 cases. The four-plus scenarios include - level 1: the disease penetrates the country; level 2: the infection is transmitted within the country; level 3: there are more than 20 cases identified within the country; and level 4: the disease is transmitted in the community with more than 1000 cases.23–25 The roles and responsibilities of other ministries in responding to COVID-19 were discussed elsewhere.8–10
Engagement and mobilization of affected and at-risk communities
Amidst the COVID-19 pandemic, effective risk communication is crucial to help at-risk people understand the situation and make informed decisions. This requires the provision of accurate information early and through channels and languages that people trust and understand.26
With regard to emergency risk communication, the MoH provided the comprehensive information on the COVID-19 situation internationally, nationally and regionally, and delivered information on preventative measures via official websites and various other means of media.7 Most of the key public health messages provided by the MoH were consistent with WHO’s recommendations i.e. practicing personal hygiene and respiratory etiquette.27,28 The only difference was the compulsory use of a facemask. While the WHO did not recommend wearing a mask for healthy people or people without respiratory symptoms,29 the MoH took a more cautious approach, which saw the requirement escalate from optional to compulsory use to align with the rapidly changing COVID-19 situation. People were mandated to cover their faces in public places from 16th March and when they went out during the social distancing period from 1st to 30th April.1,30,31 Financial penalties of 100,000 VND (USD 4.5) to 300,000 VND (USD 13) were applied to ensure adherence to the regulations.
Risk communication was a key strength of the Vietnamese response, as it leveraged both traditional media and new communication outlets such as mobile applications. Wide coverage of television, smartphone and mobile users (200 million mobile subscribers per 90 million population) made it easy for the Vietnamese government to reach out to its citizens.31 On 3rd February, when Vietnam just had eight confirmed COVID-19 cases, SMS were sent to mobile users.6 Additionally, four mobile apps, namely SuckhoeVietnam, COVID-19, NCOVI and VietnamHealth, were developed during this period to serve the COVID-19 prevention strategy (Online Supplementary Document, Appendix 1).32–34
Vietnam’s successful communication strategy catalyzes the active participation of both governmental and private sectors as well as communities. The government centers its people in an active role with the slogan translated as “every citizen is a soldier”. In addition, nongovernment-led initiatives including the donation of funds and personal protection equipment by entrepreneurs and individuals have contributed positively to social stability. For example, “the rice ATM” - a free rice dispenser reserved for the most vulnerable people, including those who lost income due to the pandemic, the elderly, students and disabled people.35–37 Students have been mobilized to assist in epidemic control by engaging them in various roles such as data entry, sample collection or provision of phone counseling for COVID-19 suspected people. However, the number of students who joined the COVID-19 taskforce was very small (124 volunteer medical students) compared to its capacity.38 At the central level, a relief bill of approximately 80,600 VND billion was signed by the government to address the financial burden resulting from the COVID-19 pandemic. Nearly 62,000 VND billion of these funds were allocated to individuals who were poor, near poor, with meritorious services or under social protection schemes. The remaining funds were allocated to support small to medium production and business establishments.39
Implementation of context-appropriate public health measures to slow transmission and control sporadic cases
Consistent with WHO’s recommendations, Vietnam administered contextualized critical public health measures to slow transmission of COVID-19 including strengthening the disease surveillance system, establishing a rapid response team, rigid monitoring at points of entry, strengthening of infection prevention and control strategies, applying mandatory health regulations, lockdown and movement restrictions (Figure 3).
Surveillance
Due to its limited resources, Vietnam deployed a strategy of early detection, isolation, contact tracing and quarantine instead of pursuing an extensive testing system. Rigorous investigation of epidemiological sources of patients and tracing of contacts has been employed from as early as 23rd January. An initiative of voluntary and compulsory declaration of health at points of entry was promptly introduced. It was first applied on 26th January for travelers from China, but was subsequently extended to all people entering Vietnam from 7th March.40,41 This regulation was further expanded to domestic travelers travelling either by airplane or other public transport from 21st March.42 The general public was encouraged to submit a voluntary health declaration, either online or via a mobile application named VietnamHealth to provide data for risk assessment and management.42 In April 2020, the WHO included this step in its guidelines.11 Vietnam produced COVID-19 rapid test, however, the country did not deploy mass testing as its capacity to produce only up to 10,000 test kits per day.43,44
To ease the process of case investigation, contact tracing and quarantine, Vietnam re-classified the definition of cases, suspected cases and close contacts (risk-carriers) with an application of the ‘four rings of quarantine’ system (Figure 4).27,45 People who carried a risk of coronavirus contamination were denoted as an “F” and the length of quarantine varied from 14 to 28 days. F0 signified a confirmed positive case, while F1 was a close contact of a positive case, F2 was a close contact of F1 and F3 was a close contact of F2.27,46
The other significant contributor to effective COVID-19 surveillance was the success in combining both in vitro real-time reverse transcription-polymerase chain reaction (RT-PCR) to confirm virus infection and serological test kits for the quick detection of SARS-CoV-2.47 These tests were developed by Vietnam Military Medical Institute and Viet A Joint Stock Company, which have widely used within the country to screen potential virus carriers.48 The test kit passed the Emergency Use Listing Procedure and was approved by the WHO in late April.48
To prepare for the potential spread of COVID-19, a total of 45 rapid response teams (RRT) were established on 30th January. The RRT’s missions included providing quick response and technical support for hospitals on the treatment of patients and control of infection at health facilities.49 At the local level, each Department of Health established two RRTs. Each RRT comprised a hospital leader, emergency resuscitation specialized doctor, infectious disease specialist, infectious disease control officer, emergency resuscitation or an infectious disease specialized nurse and a driver.49
Border control measures
Vietnam applied strict measures to control the spread of infection at all points of entry (PoE) (land crossing points, seaports and airports). Three key authorities were involved in COVID-19 control at PoE including immigration officers (airports), soldiers (land crossing points or borders) and health officers who are trained appropriately on infection prevention and control (IPC) by relevant health authorities.
Regarding international travel restrictions or bans, the WHO produced inconsistent advice; on the 3rd of February, the WHO initially suggested that travel restrictions may be useful to prevent the international spread of COVID-19, but later changed its guidance to “against an application of travel or trade restriction to COVID-19 affected countries” on 29th February.50,51 In contrast, Vietnam maintained that the international travel restrictions from severely affected countries were a vital measure to curb the COVID-19. These restrictions were then extended to all countries on 22nd March (Figure 3).52 At this point in time, Vietnam had only 94 cases and no reported deaths.53
Infection prevention and control (IPC)
IPC measures are essential to prevent cross-infection, not just for healthcare staff, but for others who are a part of the COVID-19 human resources. IPC should therefore be applied sufficiently at healthcare facilities at all levels, PoE and quarantine centers.11,12 Vietnam employed IPC measures effectively, with only two cross-infection cases reported in hospitals. Several guidelines to prevent infection and set up COVID-19 isolation units (in health facilities, at homes, quarantine centers and in hotels) were issued accordingly at an early stage of the pandemic.54–59 At PoE, IPC additionally followed the Law on infectious disease prevention and control (Decree 101/ND-CP).60 The government responded quickly to fill gaps in IPC when the first cases linked to malpractice in screening and triaging patients in hospitals were recorded by promptly issuing Letter 1385/BCDQG on strengthening IPC in hospitals.61 Since then, hospitals have generally had separate routes for patients with and without epidemiological factors and respiratory symptoms.61 IPC principles, in general, were consistent between the WHO guidelines and the MoH’s response, except for their guidance on the use of facemasks. At the early stage of the outbreak, the WHO interim guidelines recommended that health workers at in-patient facilities were not required to use PPE if physical distancing was achieved, and that the use of a facemask was not necessary for patients without suspected COVID-19 symptoms.29 In contrast, these measures were mandated in Vietnam.
Curfews, restrictions, and lockdown
There are no universal guidelines for the application of curfews, restrictions, and lockdown measures from the WHO. Individual countries were to decide the level and scope of these measures based on their own situations and priorities. Of these measures, compulsory quarantine, visa suspension, border closure and social distancing were commonplace and were critical COVID-19 measures in Vietnam.
Apart from human international travel restrictions (PoE control section), Vietnam ordered restrictive domestic movement in March 2020, during the peak period of the first wave. For example, the tourism industry was closed in some areas from 9th March and then nationally in April during the national social distancing period.62,63 Another strict measure was the school shutdown from 6th February until early May.64 National social distancing was ordered on 28th March when the country had a total of 171 cases and 8 new cases and was removed on 22nd April when no new cases were reported within a week.7 Like many other countries, the social distancing order restricted most ordinary activities including un-serviced public transport and non-essential business activities. People were required to stay at home and work from home and going out was only allowed for essential activities such as buying food or medicine.19
Compared to social distancing, lockdown was more restrictive and people were not allowed to leave quarantine areas, which were defined and maintained by the Vietnam armed forces (full name here please), accompanied by the health teams. Health teams performed temperature checks twice a day and provided other urgent healthcare. Police ensured the safety of quarantine areas. The duration of quarantine varied by location but ranged between 14 and 28 days. Lockdown was normally ordered if a case was identified, and a lockdown could be applied regardless of the size of the area, from the smallest residential management unit (a building) to an entire district.27
Provision of clinical care and maintaining of essential health services to reduce mortality
Per WHO’s recommendations, Vietnam strengthened preventative measures at all levels and initially used telemedicine to monitor patients while reducing the risks of infection with COVID-19 for patients.12
According to the 2018 national census conducted by the General Statistics Office of Vietnam, there were 295,800 patient-beds (equivalent to 28/10,000 inhabitants) and 84,800 doctors (equivalent to 8,6/10,000 inhabitants).65 Thus, Vietnam applied rigorous public health measures (public health measure section) to reduce the burden on clinical care. Further, Vietnam’s existing health system enabled the government to decentralize treatment for COVID-19 while maintaining its effectiveness.66–68
Provincial Centers for Disease Control (CDC) are focal points for the preventative medicine system. Vietnam has 47 central hospitals, 430 provincial or municipal hospitals, 1,030 district hospitals, 63 CDCs, 500 district health centers and 11,100 commune health stations.66 The private curative system has 231 hospitals at the central level and 35,000 health facilities at the local level. Hospitals are larger and more technologically advanced than health centers and health facilities. Central hospitals conduct research and have more advanced treatments available in key areas, and provide guidance and technical assistance to the local level.66 Currently, only the public health system provides COVID-19 treatments.
This decentralization of treatment reduces the unnecessary patient referrals and potential infection. It means that district hospitals are involved in the treatment of COVID-19 patients with a mild prognosis. Referral of patients were only applied for complicated COVID-19 cases.68 Treatment of patients followed the national guidelines in direct consultation with the rapid response teams.24 As per the WHO’s recommendation, Vietnam postponed non-prioritized health services such as physiotherapy, immunization and health screening during the peak of the pandemic.69 Activities targeting the high-risk groups were implemented, including home-based medical examination, telemedicine and health management for the elderly and those with chronic health conditions.70,71
Adoption of strategies based on risk, capacity and vulnerability
Vietnam adopted strategies suitable for its economic circumstances, social structure and administrative management and health system. The country decentralized COVID-19 case management, treatment and IPC to reduce the burden on the clinical system (Figure 5). Control of sources of infection was contextualized in line with the functions of professional departments with cross-sectoral participation. Policies that directly targeted vulnerable groups made important contributions to ensuring the trust of the population and maintaining social stability. This is one of the likely reasons that contributed why the country’s citizens responded simultaneously to government appeals and COVID-19 preventive measures.
A comparison of the COVID-19 control strategies used by the Vietnamese government and the WHO is described in Online Supplementary Document, Appendix 2.
Discussion
To the best of our knowledge, this is among the first studiy to review the policies and state-led responses to COVID-19 in Vietnam, with reference to the WHO’s recommended national strategies. We found that most measures were in compliance with the WHO guidelines. Notably, additional measures beyond the WHO’s recommendations were also implemented, such as the introduction of travel restrictions and the mandated use of facemasks in public. We underlined four key factors that contributed strategically to slowing the spread of COVID-19 including strong leadership, timely responses, effective risk communication, community engagement, successful infection prevention and control, surveillance and rapid-test kit production. These factors worked collaboratively to ensure better outcomes.
Although some articles highlighted the early response and strong leadership of the Vietnamese government in responding to COVID-19, details of what these early responses were and the actions indicating the firm leadership seem to have been overlooked.8–11 Our study fills this gap by reviewing the actions and timelines of policies that the government deployed. It strengthens the view that strong leadership and early responses are the keys to successful COVID-19 control.8–11 This paper also found that the decisiveness of the government led to a quick and society-wide response, enabling the health system to prevent a health crisis. Taiwan and New Zealand shared a similar approach and both countries showed initial success.72,73 It took New Zealand only ten days to order a nationwide lockdown once the government observed an increasing trend of COVID-19 community transmission within the country.73 Swift actions and preparation for the predicted pandemic trend helped Vietnam to slow and contain the widespread of COVID-19. Slowing the disease outbreak is essential to prevent the surge and overwhelming of health facilities, where the demand for health care outweighs supply; a circumstance associated with increased mortality and morbidity.74 One of the factors that probably had substantial effect towards such a favorable response was experience from the SARS pandemic in 2003. This is of special importance as the Vietnamese healthcare system is improving, but it still has a limited capacity with an average of 8.6 doctors per 10,000 inhabitants and 28 patient beds per 10,000 inhabitants.65 Thus, a nationwide outbreak would certainly have challenged the country’s health care system.66
Vietnam has also benefited from its policy of mandatory facemask use and the application of travel restrictions, which were not a part of the WHO’s recommendations. The WHO changed its recommendations on face masks at crowded places for the general public where maintaining physical distancing is unachievable in June.75 A recent systemic review and meta-analysis indicated that physical distancing, face masks and eye protection are effective in preventing person-to-person transmission of COVID-19.76 The Center for Disease Control (CDC) in the USA recognized that wearing a mask prevents asymptomatic patients to transmit the virus to others.77 Given the successful evidence of mandatory mask use in Vietnam and China, around 50 countries around the world have since required people to “cover their faces when they leave homes” .78 Although studies on the effectiveness of the early international travel restrictions are limited, results from our study and that of Chinazzi et al on the effect of travel restriction on mitigation of COVID-19, suggest that travel restriction combined with rigorous public measures and behavioral change can reduce the transmissibility of the coronavirus.79 Currently, many countries around the world have travel restrictions and travel bans in place.
Our findings suggest that the “fierce responses” of the Vietnamese government from the time of the outbreak in China inspired trust in the populous country of Vietnam. This is a cornerstone in enabling high-ranking leaders to make strategic decisions without major objections. Additionally, the one-party political institutions of Vietnam and its administrative management regime ensure that COVID-19 control orders and preventative measures are implemented systemically from the central to grassroots levels. For instance, the government decided that the need to combat the disease outweighed the economic costs of shutting down internal tourism, schools and international travel despite a relatively low number of cases identified within the country. Instead of drawing criticism, the government gained widespread support from its citizens, despite a huge projected economic loss due to the travel ban; between $5.9 and $7 billion was lost within three months (from March).80,81 Furthermore, the first nationwide partial lockdown showed impacts on individual life and work. Up to 61.6% of respondents reported their incomes were reduced, with the rate being higher among women.80 Both quality and quantity of work were drastically reduced while fear of stigmatization increased.82 The issues of anxiety and depression among people under the lockdown were reported in many countries including Vietnam.83–86
Effective emergency risk communication and community participation were an essential element of Vietnam’s strategy against the pandemic. The aggressive communication campaign through official and non-official channels proved effective, though no studies were conducted to assess the awareness and practice of the general population regarding risk communication launched by the government. However, the country ranked top of 45 countries with regard to public trust in COVID-19 responses worldwide, based on an online survey conducted by Dalia.87 As opposed to China, which used an orthodox authoritarian style, Vietnam applied more transparent approaches in battling this pandemic. This is reflected in the way in which the government recognized the power of social networks and media to spread information and the transparency of the data while screening misleading information.88,89
Although there is insufficient evidence to conclude the relationship between public trust and its contribution to controlling COVID-19 based on this data, looking at the phenomenon in other Southeast Asian countries, there is an indication that transparent information led to better public trust and response to COVID-19. For example, public trust in COVID-19 information provided by the Vietnamese and Thai governments differed. Despite both countries recording their first cases at a similar time (January), at the time of writing this paper the number of COVID-19 cases in Thailand was almost seven times greater than in Vietnam.90 Similarly, Indonesians criticized their government for a lack of transparency and required more information and stronger responses against the COVID-19 crisis.91 The first case in Indonesia was confirmed on 2nd March but escalated to 686 cases and 55 fatal cases within three weeks.90,91 This emphasizes that effective risk communication combined with strong risk management support is required to control COVID-19.
The involvement of communities in anti- pandemic work with the slogan “every citizen is a soldier” was a wise choice for the Vietnamese government.92 While the slogan may seem to be “propaganda”, it had a positive effect. Without voluntary adherence to the recommended personal protection measures, the government would have struggled to reach its goals. Once again, media was the catalyst to promote community participation. Thus, to end the pandemic, the community must be a part of the solution and behavior change is key to stopping the spreading of the disease.26,91
Regarding medical supply assistance, it is worthy to note that Vietnam has a stable supply of masks from its garment industry, which strongly supports the mandatory facemask policy. Like many countries, Vietnam is also developing its own vaccines against COVID-19. Developed by Nanogen company, Vietnam Military Medical Academy, Nano Covax is the most promising candidate to date and is in the first stage of a trial.93 Without a vaccine, zero deaths in Vietnam by the end of the first wave of the pandemic is attributed to a successful formula combining effective IPC, surveillance and disease treatment. Successful IPC and surveillance, subsequently, contribute tremendously to reduce contact to COVID-19 risk bearers. The low number of infected cases minimized the burden on health facilities and frontline health staff in hospitals. During the first wave of the pandemic, vaccines had not approved for use on human, widespread testing was necessary to ease quarantine and isolation restrictions.94 With a high infection rate, a resurgence can happen in a matter of weeks.95 However, if a country can administer tests to detect COVID-19, process tests, track positive cases and conduct contact tracing rapidly, they have a good chance of gaining control of the pandemic. Timing is exceedingly important since many countries are “buying time” whilst waiting for a vaccine to battle the virus.96 The combination of both Real-time PCR test and quick serological test enabled Vietnam to suppress infection quickly.
By April, only five countries succeeded in manufacturing COVID-19 rapid tests, with the Republic of Korea leading the list. Korea deployed a massive testing system and aggressive approaching methods, with the test showing results in only ten minutes.43,96 This allowed life in Korea to return to normal. If Vietnam is a cost-effective model for low-middle income countries, Korea on the other hand is a promising model in dealing COVID-19 crisis for more open societies.
Limitations
As this study was a critical analysis of the responses of the Vietnamese government to the COVID pandemic up to 19th July, the analysis is undertaken to the best knowledge of the authors according to the information gathered. This paper did not cover responses from the second wave of COVID-19 from 20 July with hotspots in Da Nang and Quang Nam since the governmental response strategies changed slightly with a focus on the local level. A separate review paper dedicated to this period will be needed. The authors acknowledge that trends and resources are likely to change with time, beyond the publication of this article. Further, as this analysis focused on health policy and overall health systems, other components of the health system that are not covered may also be important, such as health financing and quality of health services.
Conclusions
Our findings suggest that with limited resources, the adapted health system in Vietnam contributed to the successful containment of COVID-19 within the country. The firm leadership and political will of the government enabled the whole-society approach, which was critical to gain control of the pandemic. We recommend the application of travel restrictions and rigorous infection prevention and control should be put in place at the early stages of the pandemic. Travel restrictions may be eased once a country has successfully managed to control the spread of COVID-19.
Acknowledgments
We would like to thank Mr. Philip Degenhardt, Rosa Luxemburg Stiftung, who gave valuable contributions in reviewing the draft of this manuscript.
Funding
This research project is financially supported by Rosa Luxemburg Stiftung. The content of the publication is the sole responsibility of authors (independent researchers) and does not necessarily reflect the position of Rosa Luxemburg Stiftung and their organizational affiliations.
Authorship contributions
LTTT: Conceptualization, Methodology, Writing: original draft, review & editing. EOM: visualization, Writing: original draft, review & editing. DPV: Writing: review & editing and visualization. MP: Visualization, Writing: review & editing. RC: Writing: review & editing. HN: Writing: review & editing. DB: Writing: review & editing, supervision.
Competing interests
The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Luong Tran
Migrant Health Project Officer
International Organization for Migration (IOM) Viet Nam
304 Kim Ma, Ba Dinh, Ha Noi, Viet Nam
[email protected]