The World Health Report 20061 demonstrated the uneven distribution of health professionals among countries and regionally within the countries, pointing out the negative consequences of this scenario for universal health services coverage. This imbalance is characterized by the concentration of professionals in urban areas and lack thereof in rural areas. Ono et al.2 found a similar scenario in virtually all Organization for Economic Co-operation and Development (OECD) countries, with a lack of professionals not only in rural areas but also in poor urban and suburban regions. Universal health coverage thus depends on strategies to allocate more health professionals in these deprived areas.
Brazil also presents significant inequality in the distribution of doctors. Although data indicate an increase in density of doctors’ ratio in the period from 1980 to 2015, from 1.15 to 2.11 doctors per thousand inhabitants, specific data from 2018 show that this density varied from 1.16 in the Northern Region to 2.81 in the Southeast Region. There was an even more significant discrepancy: the density of doctors in the capitals was 5.07 and in the other towns was 1.28 doctors per 1000 inhabitants. Furthermore, cities with up to 50 thousand residents had less than one doctor per thousand inhabitants, while the 42 largest Brazilian cities had 4.33 doctors per thousand inhabitants. Thus, 30.2% of the population in large cities is served by 60.2% of physicians working in the country.3 This highlights the need to further improve policies for the management of human resources in healthcare in Brazil.
The healthcare workforce’s quality, profile, and distribution are crucial determinants for the performance of the health system. Therefore, public policies must privilege planning the development and allocation of the health workforce in order to guarantee the population’s right to health and universal health coverage.4 According to the model by Campbell et al.,5 this planning should consider four dimensions: (i) availability, with sufficient supply, and stock of health professionals; (ii) accessibility, with equitable access to health professionals, close to the communities served; (iii) acceptability, i.e., the ability of health professionals to treat people with dignity and create trust; and (iv) quality, or the knowledge and technical skills of health workers.
The World Health Organization6 supports the strengthening of primary health care (PHC) as a means to achieve universal health coverage. According to the organization, it is essential to prepare and motivate healthcare workers, place them where they are needed, and offer resources, materials, and equipment to perform their function. Quality PHC services prevent and treat various acute and chronic diseases. It is the first line of defense for global health security.7 Studies on the impact of PHC organizational models, such as the Family Health Strategy (Estratégia Saúde da Família – ESF, in Portuguese), are essential to contribute to the expansion of these services.
In Brazil, the ESF influenced the expansion of the PHC, since municipalities received financial incentives to improve PHC, conditioned to the implementation of the ESF. The number of ESF teams increased from 2,054 in July 1998 to 42,893 in October 2019.8 However, the systematic difficulty in hiring physicians to work in ESF teams in some locations has led to the implementation of supplementary policies at a national level: Programa de Interiorização do Trabalho em Saúde (PITS),9 Fundo de Financiamento Estudantil (Fies),10 Programa de Valorização dos Profissionais da Atenção Básica (Provab),11 and Programa Mais Médicos (PMM).12
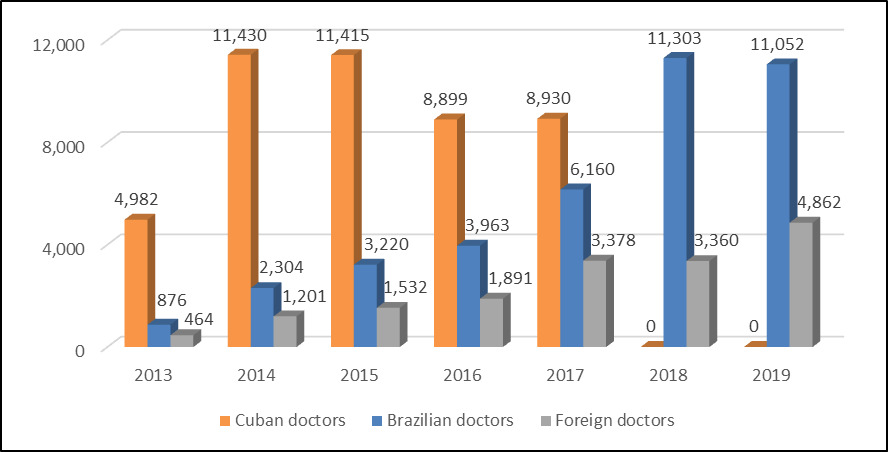
PITS, Provab, and PMM shared similar approaches, combining financial incentives for training, and professional and personal support to doctors.13 PMM accepts physicians trained abroad and does not require validating the degree in Brazil, so-called ‘foreign doctors,’ and professionals from Cuba, appointed within the scope of Brazil’s agreement with the Pan American Health Organization (PAHO).14 When doctors are hired in the scope of an international agreement, after the contract between countries is terminated, it is not always possible to replace all of them.15 In 2018, physicians from Cuba have occupied more than 60% of the PMM positions, which represented a risk to the program. The risk was materialized on November 12, 2018, with the Cuban government’s decision to terminate its participation in the PMM, and 8,300 doctors departed from Brazil within a month.16
In this context of difficulties to retain health workers to be rural and poor urban regions, the main objective of this study is to analyze the policies of the Brazilian federal government to provide health professionals in underprivileged areas. The research observes the strategies of the programs PITS, FIES, Provab, and the PMM to attract workers to act in PHC of the national health system (SUS), with a perspective of reaching universal health coverage. In addition, the study offers recommendations to contribute to future policies. The specific objectives of this research are: (i) to perform a comparative analysis of the strategies implemented by each program; (ii) verify the effect of these programs on the availability of doctors working in PHC; (iii) analyze the participation of Brazilian physicians in the PMM; and (iv) provide input and recommendations to allocate and maintain physicians in rural areas and underprivileged neighborhoods of large cities.
METHODS
The research combined a scoping review, based on official documents of the Brazilian federal government, and analysis of secondary data made available by the Brazilian Ministry of Health and official Brazilian government websites.
The literature and document review examined the incentives used in Brazilian government programs, at the federal level, to attract and retain doctors in primary health care (PHC) in the Brazilian health system (SUS). Articles, dissertation, and thesis were found on online academic databases, using descriptors named after the Brazilian medical supply programs analyzed in this study. The official documents of the Brazilian federal government consisted of legal norms (e.g., laws, decrees, and ordinances).
The following indicators were used to identify the expansion of the supply of doctors in PHC in recent years: (i) number of doctors on ESF teams, (ii) number of doctors in PHC, not linked to ESF; and (iii) population coverage by PHC. The historical series of these indicators, from 2007 to 2019, were accessed on the website of the Ministry of Health’s PHC Secretariat (SAPS/MS).17
The number of doctors on ESF teams was calculated based on the number of teams (each team requires the presence of a doctor, with a medical workload of 40 hours per week). The number of doctors in PHC, but not linked to ESF, was calculated based on the number of other teams working in the primary health teams, and the weekly hours of PHC doctors (40 hours’ medical workload was considered the doctor’s workload, fractions were also considered). The indicator population coverage by PHC used was available on the SAPS/MS website.18
For the analysis of the registered doctors working in PHC of SUS, the study collected data from the number of existing positions per municipality (occupied and vacant in July 2019), along with data from professionals participating in the PMM, obtained from the database of the Program Management System (SGP), made available by the Ministry of Health through the Brazilian freedom of information law.19 This database contains the dates of entry and exit in the program, the municipality of the health center of professionals, from the beginning of the program until October 15, 2019.
The database of professionals in the program had 45,288 records. A first analysis was carried out, proceeding with the exclusion of 43 records with a date of entry into the program prior to August 2013 (the month when the PMM started to recruit); exclusion of 152 records of professionals who had three or more records in the database, identified by name and date of birth, that were not in accordance with the data available in the National Registry System of Health Facilities;20 exclusion of 36 records with an entry date later than the exit date; attribution of an exit date for 1,153 records of duplicate entries of professionals whose exit date from the municipality with the oldest entry date, was later than the entry date of the municipality with the most recent entry date, considering the impossibility of the program awarding two stipends at the same time to the same doctor; and attribution of an exit date of November 30, 2018, in 416 records of Cuban doctors with exit date in 2019 or who were registered as active in the program, considering the end of the agreement with the Cuban government in 2018. After this exclusion, 45,057 records were considered for this study.
RESULTS
Programs to expand the supply of doctors in PHC of SUS
The Programa de Interiorização do Trabalho em Saúde (PITS), established in 2001, sought to attract doctors to underprivileged and remote municipalities through incentives such as (i) financial compensation, in the form of a contract signed with the municipality and a supplementary stipend paid by the federal government for up to two years, (ii) professional education, including a specialization program in family health with mentoring and supervision, (iii) professional support and adequate working conditions in the health unit, and (iv) personal support, through housing, food, and transportation. Therefore, despite efforts to select and retain these professionals, the high percentage of dropouts and dismissals led to the end of the program in 2004.9
The strategy of the Fundo de Financiamento Estudantil (Fies), provided by Law 12202/2010,10 focuses on financial incentives. The newly graduated doctors who accessed the subsidized loans offered by Fies may request a reduction of 1% of the debt balance per month of participation in a team operating the family health strategy in regions appointed by the Ministry of Health, based on the shortage of health professionals. Under these conditions, until November 2018, only 711 doctors who took loans from the Fies requested the debt reduction.21
The Programa de Valorização dos Profissionais da Atenção Básica (Provab), established in by the Inter-Ministerial Ordinance MS/MEC 2087/2011,11 presented a similar strategy to the PITS, combining financial incentives and training, in addition to professional and personal support for the doctors. Besides that, the professionals selected started to be hired and paid through a stipend by the federal government, and receive an extra score in competitive selection processes of medical residency, after evaluation and accomplishing the program’s goals. In 2015, the selection of doctors for Provab was integrated into the selection of the Programa Mais Médicos (PMM), and the applicants could choose between the additional score in the medical residency selection processes or having a guaranteed stipend for three years.22
PMM, regulated by Law 12871/2013,12 was designed to tackle the demand of doctors in PHC, which was not met by the previous programs. In the first axis, focused on the emergency supply of doctors, after opening the positions for doctors registered in Brazil, the remaining vacancies were made available to (1) professionals trained abroad without a validated qualification in Brazil (foreign doctors); and (2) Cuban doctors appointed within the scope of Brazil’s agreement with the Pan American Health Organization (PAHO).10 By attracting health workers from abroad, the PMM addressed not only the dimension of accessibility or adequate distribution of doctors but also the dimension of availability of health workers in the country, adopting a short-term strategy, according to the model proposed by Campbell et al..5
In the second axis focused on investment in infrastructure, the federal government assumes part of the municipalities’ responsibilities regarding the provision of adequate conditions in the health unit, which includes the construction, renovation, and expansion of basic health units, as well as computerization and implementation of a new PHC information system. The third axis, focused in medical training, included a long-term strategy to guarantee the availability of physicians in the model proposed by Campbell et al.,5 ensuring the supply and stock of health workers in the country, in addition to reorienting the training of doctors, at the undergraduate and residency level, to work in SUS and PHC.
Effects of programs to expand the supply of doctors in PHC
Figure 1 shows the number of doctors in ESF teams (ESF doctors), the number of doctors in PHC, not working in the family health strategy (PHC doctors), and the percentage of the population covered by PHC (PHC coverage), in the period from 2007 to 2019.
The increase in the number of ESF doctors suggests an effect of the federal policy to encourage the establishment and maintenance of this strategy within the organization model of PHC. This trend is accompanied by a reduction in the number of doctors not working in the ESF, in most years, probably because of the conversion of the traditional health care model to the ESF. However, the PHC financing model has recently changed,23 and the effects of this reform are yet unknown . The new model extinguished the financial incentives conditioned to the implantation and maintenance of ESF teams and equaled them to PHC teams. For the latter, the physicians’ and nurses’ workload are more flexible, and the presence of community health agents is not required.24
The growth in the number of doctors in the ESF, however, does not reflect the total number of doctors who joined Provab and the PMM, mainly from 2013 onwards. According to the management report by SGETS/MS, these two programs, together, hired around 18,000 new doctors between 2013 and 2015.22 However, the increase in the number of doctors in ESF teams was 6,866 in these three years, which represents only 37.6% of the total number of doctors hired.
Miranda et al.25 suggest that this divergence occurs because the physicians join existing teams. However, it is possible that some doctors were assigned to basic health units in a traditional health care model. This explanation is supported by the increase in the number of doctors not working in ESF in 2013 and 2014. The option of hiring professionals through PMM to work outside the ESF was later authorized by Ordinance MS/SAS 1143 of October 2014.26
The reduction in the total number of physicians in PHC from 2014 to 2015 shows that Provab and the PMM were not able to guarantee an increase in the availability of doctors. The total number of doctors increased above the thresholds previously observed, only in 2017. There was a reduction in the total number of doctors in 2018, possibly because of the end of the agreement with the Cuban government for the PMM. In September 2019, the total number of doctors in PHC was still less than that presented in December 2018; therefore, the medical workforce was not entirely restored.
Although there were fluctuations in the total number of doctors in PHC, the percentage of the population covered increased from 2007 to 2017, remaining constant throughout the rest of the analyzed period. This occurs because of the number of doctors in ESF teams observed in those years and the method of calculating the percentage of the population covered by PHC. It considers that an ESF team – counting on a doctor available for 40 hours per week, in addition to the service of other health workers (nurse and auxiliary nurses) and community health agents – has a higher capacity to serve the population, compared to the presence of a physician working in a traditional health care model.
Brazilian doctors in the Programa Mais Médicos (PMM)
Figure 2 shows an increase in the percentage of active contracts of Brazilian doctors between 2013 and 2017, from 13.9% to 33.4%, even though the agreement with the Cuban government was already in force. After the end of the agreement with Cuba, the participation of Brazilian professionals rose to 77.1% in December 2018, possibly due to the efforts of the Brazilian government to fill the vacancies by launching two selection processes during that year.27 In October 2019, this percentage dropped to 69.4%, which indicates the difficulty of maintaining these professionals, although two more selection processes were launched to fill the program’s vacancies.28
This tendency suggests that if the agreement with the Cuban government had not ended abruptly, the vacancies previously filled by Cuba physicians could be gradually filled by Brazilian doctors, partly as a result of the increase in the number of vacancies offered in undergraduate medical programs, particularly from 2003 onwards. Data from Instituto Nacional de Pesquisas Educacionais Anísio Teixeira (INEP - Brazilian institution of educational research of the Ministry of Education) show that there was an increase of 6,172 places offered in undergraduate medical programs from 2003 to 2010, and an increase of 19,187 places from 2011 to 2018.29 The more robust increase in this second period is partly the result of the medical training axis of the PMM, which changed the procedures to certify new undergraduate medical programs, and the opening of new places in existing undergraduate medical programs.10
Although there was an increase in the participation of Brazilian physicians in the period analyzed, the total number of active doctors in the PMM in October 2019 was still not enough to replace the Cuban doctors. In December 2017, there were 18,468 active doctors; in October 2019, there were 15,914. Of the 2,894 vacancies in the program in July 2019, 64.8% had been occupied by Cuban doctors in December 2017. The municipalities with the highest number of vacancies that had been occupied by Cuban doctors are large (more than 500 thousand inhabitants) of the Southeast Region, such as São Paulo (71) and Rio de Janeiro (41), and in the federal capital Brasília (21), probably in basic health units located in poor suburban neighborhoods.
The profile analysis of the 358 physicians occupying vacancies in Special Indigenous Health Districts in October 2019 shows that only 79 (22.1%) were Brazilian professionals. In addition, among the doctors assigned to these districts, 88.3% had joined the program less than a year ago, which indicates low retention of the health workers in these locations. This highlights the need for specific policies to attract and retain doctors to provide PHC services to the indigenous population.
DISCUSSION
The increase of PHC coverage suggests that the analyzed programs have improved accessibility by increasing the availability of health workers in basic health units. However, its effects seem to have reached a limit: population coverage has remained at 74.6% since 2017. This indicates that these policies have been effective, but new strategies are needed to attract and retain these professionals in PHC.
The analysis of the Brazilian programs to expand the supply of doctors in PHC identified some strategic lines that brought innovation to the policy and increased access to health services: (1) hiring doctors via the federal government, was important to reduce bureaucracy at the local level and standardized compensation, which may have contributed to reducing wage competition and the turnover of these professionals between municipalities; (2) providing the opportunity for physicians not registered in Brazil to apply for the positions, meeting the demand in the short term; and (3) establishing a strategy to train a more significant number of doctors, by increasing the number of places in undergraduate medical programs and the stock of doctors in the long run.
Despite the advances, there are still challenges to overcome. It has been difficult to attract and retain Brazilian professionals to Special Indigenous Sanitary Districts, to municipalities far from urban centers, or to underprivileged suburban areas. The current Brazilian policy to expand the supply of doctors in PHC was established by Law 13958/2019, known as Programa Médicos pelo Brasil, and seeks to address these challenges. The program emphasizes the supply of health workers a) in municipalities of small population size, low population density, and far from urban centers, b) in Special Indigenous Sanitary Districts, quilombo settlements, or riverside communities; and c) places of high vulnerability, with a high proportion of the low-income population.30 However, the policy is restricted to the supply of physicians and neglects strategies adopted in previous policies, such as improving the infrastructure of basic health units and actions to train doctors.31
In this context, new strategies are needed to overcome the gaps in PHC, attracting and retaining doctors and better serving the population. Some alternatives have already been recommended, such as the expansion of nurses’ duties in PHC, through training them at a graduate level. With this measure, health workers will have greater autonomy in decision-making to manage the care of patients with mild acute illnesses or already diagnosed with chronic diseases.32 The duties of other health professionals, such as auxiliary nurses and community health agents, can also be expanded through providing specific technical courses and developing clinical protocols of activity. These measures can enhance the reach of the services, and expand the scope and the effectiveness of ESF teams, regardless of whether the doctor is present.
Another mechanism to promote access to health services, especially to populations living in municipalities far from large urban centers, is the implementation of medical teleconsultation services. Teleconsultations could be carried out in basic health units, with the assistance of a nurse or another health professional.33 However, both the expansion of the role of health professionals and the operation of teleconsultations require agreements with the professional regulation councils that discuss law changes. Teleconsultation is currently prohibited by Resolution 1974/2011 of the Federal Council of Medicine.34 Due to the COVID-19 pandemic, an opening was created for the use of telemedicine, understood as the exercise of medicine mediated by technologies for assistance, research, disease and injury prevention, and promotion of health, but only while the crisis caused by the SARS-CoV-2 lasts.35 Unlike Brazil, by the end of 2015, seventeen European countries (including Portugal), and other nations such as Mexico, Australia, and Japan already used teleconsultation. In the US, among the 50 federal states, nineteen used teleconsultations without restrictions, and thirty allowed teleconsultations but required a minimum face-to-face service.36
CONCLUSIONS
Improving universal health coverage in Brazil through strengthening primary health care will require further efforts to overcome the challenge of attracting and retaining doctors to work in disadvantaged areas, increasing the availability and accessibility of health workers. Physicians, particularly young doctors, need appropriate working and living conditions in the regions where their services are needed; at the same time, they must be able to learn and evolve in their careers continuously. Therefore, the development of new policies should also be driven by these ends. In addition, new policies need to emphasize the participation of other health professionals such as nurses, auxiliary nurses, and community health agents, as well as incorporate new technology able to reduce distances between health professionals and users of the Brazilian health care system.
Acknowledgements
The authors would like to thank the Oswaldo Cruz Foundation (Fiocruz), for granting the license for training VMDF, which maintained her remuneration during the three-month leave she received from his work activities. The authors would like to thank the Universidade NOVA de Lisboa and the Institute of Hygiene and Tropical Medicine for accepting VMDF’s voluntary professional internship, and for the use of its facilities.
Funding
The authors certify that they have no affiliation with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest, and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. The authors also certify that this work was not supported by any public or private funding agency.
Authorship contributions
VMDF acquired and analyzed the data, and was a major contributor in writing the manuscript. LVL contributed in the conception of the work. All authors interpreted the data, read and approved the final manuscript.
Competing interests
The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correpondence to:
Virgínia Maria Dalfior Fava
Oswaldo Cruz Foundation (Fiocruz), Ministry of Health, Rio de Janeiro, Brazil
Av. Brasil, 4036 - Prédio da Expansão - 10º Andar – Manguinhos
CEP: 21040-361 – Rio de Janeiro – RJ – Brasil
+55 61 99922-2772
[email protected]

_and_percentage_of_the_population_covered_by_ph.tiff)

_and_percentage_of_the_population_covered_by_ph.tiff)