Current estimates show that 3 in 4 of people with diabetes live in low and middle income countries(LMIC) and about 10% of the global health expenditure is spent on diabetes.1 In 2019, India ranked second after China with about 66.8 million people with diabetes (PWD) accounting for an overall prevalence of 7.5% and is predicted to increase in the future with the largest increases in Africa, the Middle East, South East Asia and Central America.1,2 PWD in resource limited settings receive less than optimal care due to lack of understanding about the disease, fragmented health care delivery system, and poor financial resources especially in the rural areas.3–5 A suboptimal patient-physician interaction in the overcrowded outpatient wings lead to inconsistent management advice for the patients.6 In addition, delays in early diagnosis in these settings that cause greater burden of disease with complications.7 In this scenario, there is a need to identify innovative, cost effective, targeted interventions that strengthen health system to reduce the impact of diabetes in low resource settings.
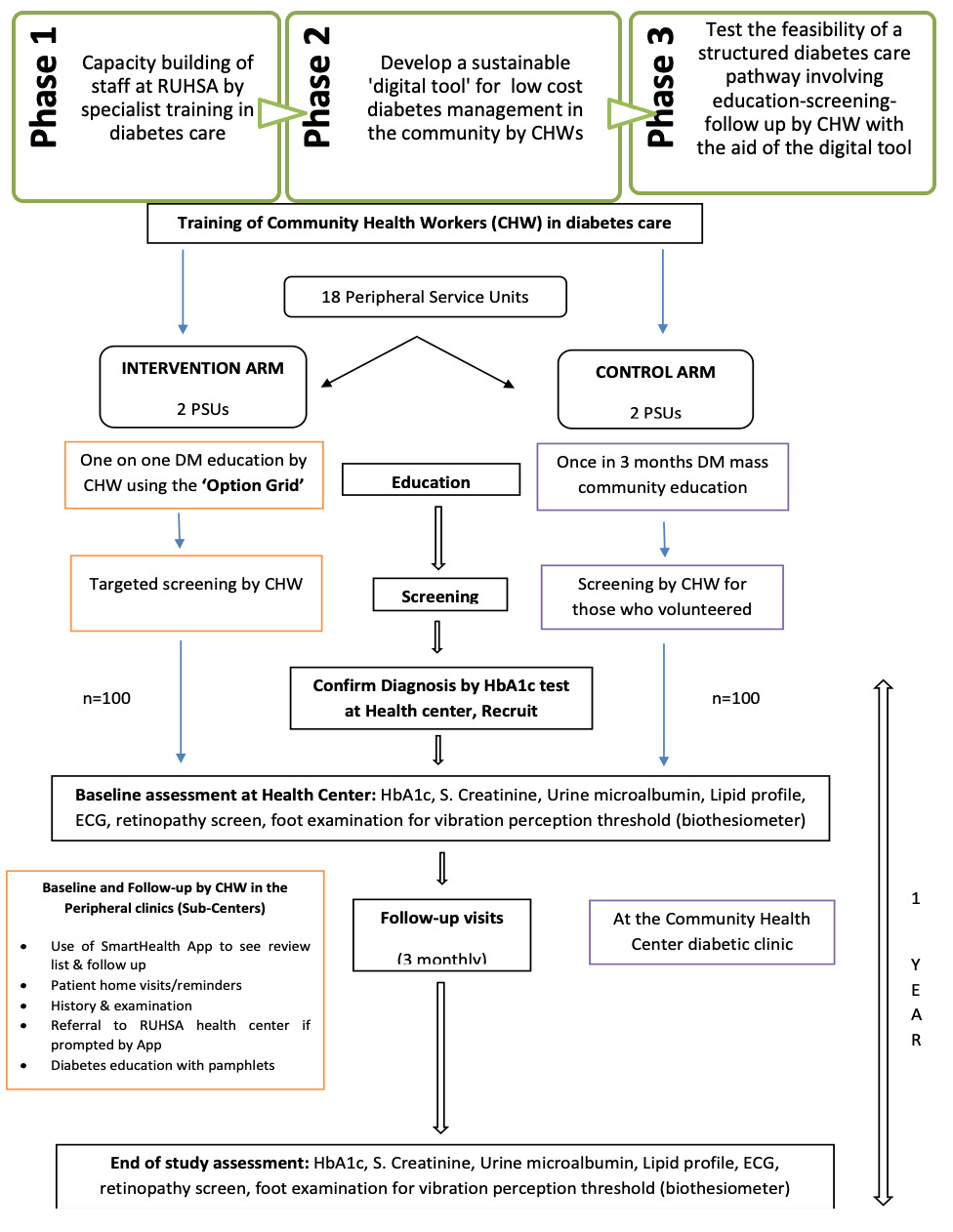
There is some evidence for the use of socially accepted community health workers (CHW) in chronic disease management. Supported by community education, CHWs will address the deficiencies in the health literacy, early detection, compliance to treatment and follow-up in the Indian health system.8 In this paper, we present the findings from a phase II, nonrandomized controlled, community trial testing the feasibility and non-inferiority of introducing trained community health workers to manage diabetes in the community. CHWs offered screening for diabetes at the outreach centers, educated the community using ‘patient educational tools’ and followed up using tablet app with action prompts comparing with the standard care comprising of weekly physician consults in the diabetic clinic at the secondary level health centre, clinic based and routine community education. This trial sought to assess the non-inferiority of community health worker initiated education, screening early detection of cases, referral for physician consultation and follow-up over standard care in terms of compliance to screening, accessing treatment, number of health worker visits and physician consultations and glycaemic control. Ethical approval was received from the Institutional Review Board in April 2016.
Methods
Study setting
The study was carried out by RUHSA (Rural Unit for Health and Social Affairs) department of Christian Medical College, Vellore, located in K.V Kuppam, a rural revenue block (an administrative unit of a district) in Vellore district of Tamil Nadu, India with a population of 140,000. RUHSA is a 70-bed secondary level health center attached to a primary care sub-center in each of the 18 peripheral service units (PSUs) in the block. As part of the RUHSA community outreach care, a peripheral health team consisting of a doctor, public health nurse, social worker, 2 cadres of community health workers (one health-aide for every PSU with minimum education level of 12th grade; and one family care volunteer (FCV) for every village who are mostly illiterate) organises twice a month clinics at the PSU (one doctor led and one nurse led), screening camps, community education camps and various socioeconomic development programmes.
Study design
It was a phase II, non-inferiority (NIF), non-randomized controlled field trial with a parallel design, open labelled and allocation ratio of 1:1 in control and intervention arms. The NIF trial design was used since the involvement of community health worker with less formalised medical training hypothesised to offer important advantages over standard treatments like convenience, better compliance and reduced cost. For the purpose of this trial, 4 PSUs (clusters) were selected, of which 2 each were chosen to be the control and intervention clusters. There were no changes to the trial design after commencement.
Existing standard care for DM at the study site
A weekly diabetes clinic follows an interdisciplinary team approach led by primary care physicians at the secondary level health center with nurse educator providing health education, physiotherapist checking the feet for peripheral neuropathy with monofilament and biothesiometer, nutritionist providing dietary advice, physician reviewing the diabetes control and ophthalmologist screening for retinopathy. The patients with complications were referred to tertiary care centre for advanced care. In addition, standard care includes active engagement of communities through diabetes awareness campaigns using multiple tools like flash cards, skits and educational videos. All the patients receive monthly medications from the doctor led clinic at the sub-center. RUHSA caters for 2300 registered diabetes patients with a weekly, half-a-day clinic attended by more than 60-80 patients, with only one senior and one junior doctor for medical consultations. This clinic burden potentially adds to doctors’ stress and suboptimal care.
Sample size and recruitment of study participants
For this feasibility study, 100 participants in each arm were deemed sufficient for proof of concept and demonstrate non-inferiority of the intervention.9 Study participants were recruited from the 4 of the 18 PSUs in K.V Kuppam block. The 4 PSUs for the pilot trial were chosen purposively based on the assumption that all the 18 PSUs in the rural block have similar socio-cultural and demographic characteristics with respect to diabetes. The information about the study was disseminated through distribution of pamphlets by CHWs in the two intervention PSUs and through standard once in 3 months mass campaigns in the two control PSUs. Volunteers from the identified PSU’s who came forward for screening, were recruited into the study. All those who had already developed severe complications including cardiovascular accidents, renal failure, myocardial infarction, liver cell failure were excluded from the study. Random Blood Sugar (RBS) test was done by the CHW on all the adult volunteers aged between 30-65 years at the PSU, who were either identified as "at risk’ or known to have diabetes. Those with RBS ≥140mg/dl and the individuals who are known to have diabetes on treatment were referred to secondary level health center for glycated haemoglobin (HbA1c) test to confirm the diagnosis or identify those with uncontrolled diabetes. Participants with HbA1c ≥ 6.5%, both new and known cases were invited to participate in the trial. Written informed consent was obtained from the participants. All the study participants, both in the intervention and control arms were offered subsidized care in order to eliminate bias due to financial constraints to access care. Recruitment of 200 consenting participants was completed over a 6 months period from March to August 2018.
Intervention package
An intervention package included development of decision making patient education tools, development of a SMARThealth app and training of CHWs in diabetes care using the educational tools and the app.
Development of decision making patient educational tools
Educational tools were developed which included one-page ‘option-grid’, pamphlets on- all about diabetes, physical activity and diet and posters. Option-Grid is a shared decision making aid, easy-to-read that help patients and providers discuss diabetes care options. The grid has the most frequently asked questions by the patients when they need to make preference-sensitive decisions and the most current evidence based responses. This option grid was in the local vernacular language.
Development of android tablet based SMARThealth App
A mobile application (App) was developed to help the CHWs to navigate patients to access care pathway. The app was conceptualized and designed by the investigators and developed in collaboration with the George Institute for Global Health (GIGH), India. The GIGH had already developed a technology platform that included risk based screening algorithms, clinical decision support systems, follow up reminder programs and reports for healthcare management collectively called SMARThealth application. SMARThealth application was developed for non-physician healthcare workers to assist medical professionals in assessing and/or managing a person’s health. The application was modified and designed to address the specific objectives of this study with inputs from the authors.
Training of CHWs in diabetes care
The training of CHWs consisted of intensive 10-week training on various aspects of diabetes, screening by glucometer RBS testing and use of android tab based app with the functionality of a checklist of medical history and examination findings.
Delivery of intervention
After receiving the training, in the intervention villages, CHWs educated the participants through distribution of pictorial pamphlets and motivated to do screening for DM at sub-center (see Figure 1). Screening was encouraged, if participants had following risk factors: age above 40 years, symptoms of diabetes, family history of DM and above 30 years of age, gestational diabetes, known manifestations of complications of diabetes and high blood pressure. Option grid was used to counsel the patients on disease manifestations, complications, treatment options and facilities. The pictorial pamphlets informed them on diet and level of physical activity. In the control villages, people had exposure only to the community educational campaigns once in 3-4 months as part of the standard care.
CHWs also screened participants using glucometer random blood sugar (RBS), 3 monthly measurements of blood pressure (BP), height, weight, identification of swelling of face and feet, impairment of vision, absent dorsalis pedis pulsation and loss of sensation in the feet using monofilament. They referred participants once in 3 months for HbA1c test and annually to secondary level health center for checking of serum creatinine, lipid profile, spot urine micro-albumin, ECG, retinopathy, foot for perception of vibration with biothesiometer. Participants were referred by CHWs for physician consultation only for initiation of treatment and if a complication or uncontrolled HbA1c was detected at 3 monthly reviews.
CHWs were trained on the use of the tab app prototype, piloted on a few patients in the health center and modified. The five forms created in the app included 1. Patient identifiers, socio-demographic characteristics and RBS screening 2. HBA1c listing for recruitment 3. Participant review listing 4. Diabetes relevant history 5. Diabetes relevant examination findings. CHWs were able to access the app forms with a personalized username and password maintaining the patient data security and confidentiality. They could enter data in the app forms and get action alerts without internet in the remote rural areas. The participant review listing enabled her to see the list of patients, review dates and make a home visit once in 3 months. The data is synchronised with the server in the health center once a week.
At the diabetes clinic, the patients were assessed by the physician using password protected doctor’s review list that was generated through the risk stratification algorithms in the app and the data was entered in the doctor’s review form. The App had embedded decision-making prompts built in at every variable for both the CHWs and physicians. The standards have been fed into the programme with the internationally accepted cut-offs. The App also generated a real-time graph of number of patient visits made by the CHWs on a day to day basis and that helped the research team and physicians to monitor the CHWs work, and motivate them based on their performance.
Variables, data sources and collection methods
In the intervention arm, at first visit CHWs collected the following variables using the app: Sociodemographic characteristics, risk factors, DM complications and comorbidities including history of smoking, alcohol use, duration of DM, family history of DM, history of stroke, foot ulcer, heart attack and impaired vision. At 3 monthly physical examination, findings of weight, height, BMI, blood pressure (systolic-SBP and diastolic-DBP), foot ulcer, swelling of face and feet, dorsalis pedis pulsations, touch sensation in the feet and HbA1c levels were collected. At the physician’s consultation: blood pressure, vibration perception threshold in the feet using a biothesiometer (Digital Bio-Thesiometer, Model Vibrometer-VPT, Diabetic foot care India PVT Ltd) were done and annually, screening for retinopathy, laboratory investigations of lipid profile, urine micro albumin, serum creatinine, calculated eGFR, urine spot microalbumin/creatinine ratio and ECG were conducted. In the control arm, all variables were collected by the physician at the community health center during their regular consultation visits.
Statistical analyses
Categorical variables were summarised as counts and percentages and continuous variables were summarised using mean ±SD and median with interquartile range. The differences in percentages between the groups were assessed using Pearson’s χ2 test and the differences in the mean values of normally distributed continuous variables were tested using independent samples ‘t’ test and non-normally distributed variables were tested using Mann-Whitney U test. A P-value of <0.05 was considered statistically significant. In this study, we tested the non-inferiority of using community health workers in detection of cases and complications and selective referral for physician consultation to reduce overburdening of poorly staffed health system and ensure equity of care. Our null hypothesis was that using CHWs is not less effective to current standard care for diabetes in low resource settings. The equivalence margin was defined as recommended maximum of 4 physician review visits per year, no significant difference in case detection rates, glycemic control rates and compliance to 3 monthly HbA1c tests between the 2 arms. We estimated the effect of the intervention and the temporal trend on the glycaemic control at 3, 6, 9 and 12 months of follow-up using generalized estimating equation (GEE), with exchangeable correlation structure, adjusting for age, duration of diabetes and family history of diabetes.10 Statistical analyses were conducted using IBM SPSS version 23.0.
Results
Participants’ sociodemographic characteristics
Between March and August 2018, we recruited 200 participants with 100 in the intervention and 100 in the control arms. The socio-demographic characteristics of the subjects are shown in Table 1. Both intervention and control arm had about 60% males and 40% females. Among the intervention group, the participants were slightly younger with a mean age of 48.28 ± 7.32 whereas in control was 51.31 ± 8.9 (P=0.009). About 40% had an education level of more than 9th grade in both groups.
Participants’ medical history and diabetes disease status at baseline
The median duration of diabetes was 5 years (interquartile range of 3-10 years) and 6 years (interquartile range of 3-8 years) in the intervention and control group respectively; mean HbA1c level was 8.11% (SD = 1.51) in both groups; only about 20-30% of the known diabetics had good control of diabetes with HbA1c level below 7%. About 60% were overavweight and obese and one-third of them were hypertensives in both the groups (Table 2).
Study outcomes
The primary outcomes measured were as follows: comparison of process indicators like compliance to regular and structured screening for complications by CHWs in the intervention arm, compliance to HbA1c monitoring (Table 3) and compliance to annual recommended intvestigations (Table 4). The outcome indicators were case detection rate in the population, both new and known cases, number of physician consultation visits and glycaemic control at 3, 6, 9 and 12 months of follow-up (Table 5).
Case detection and screening for complications by health workers
In the intervention arm, health workers were able to identify 100 confirmed diabetes cases by screening only 178 informed people, self-referring to sub-centers whereas in the control arm, they had to screen 259 people to recruit 100 participants. The case detection rate (P=0.0003) and compliance to 3 monthly HbA1c level measurements (Table 3) were significantly higher and compliance to recommended annual investigations was nearly significant (Table 4) in the intervention arm. The compliance to retinopathy screening was equal in both arms because there was a special retinopathy screening initiative led by the ophthalmologists during the study period.
Of the 40 who were identified to have impaired vision and referred for care, 27(67.5%) were screened for retinopathy and 3 (11%) had retinopathy; of the 23 who were detected to have swelling of feet, 22 were tested for serum creatinine and 1 had more than 1.6mg/dl, 2 had eGFR less than 60 ml/min/1.73 m2; 8 were detected to have foot ulcers and were referred for treatment; 5 had loss of touch sensation in the feet and 4 found to have absent dorsalis pedis pulsation and were further investigated.
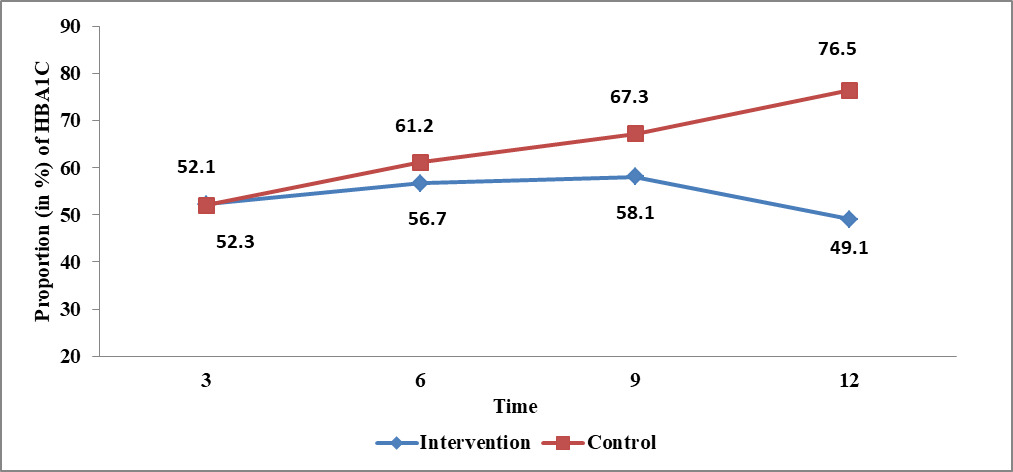
Glycaemic control and physician consultation visits
We found the number of physician consultation visits to community health center was significantly reduced in the intervention arm (Table 5, P=0.041). Further, the generalized estimated equation analysis showed that there was a significant reduction in the proportion of subjects having HBA1c >7% in the intervention arm compared to control arm (odds ratio, OR=0.72, 95% confidence interval, CI=0.54, 0.98) overtime (Table 6, P=0.036, Figure 2) after adjusting for age, duration of diabetes and family history of diabetes.
Discussion
Escalating prevalence of diabetes in LMICs9 with its inefficient health care system and poorly informed clients warrants us to identify innovative, feasible interventions to strengthen health system and reduce the impact of diabetes in these communities. This community-based trial assessed the feasibility and non-inferiority of trained community health workers to impart diabetes awareness in the community and offer screening for early case detection and complications to improve diabetes management in low resource settings. The main findings were that the health workers could effectively educate and significantly improve the early detection of cases, screen for complications of DM using a simple checklist (Table 4). In addition they facilitated improved compliance to structured follow-up with HbA1c (Table 3) and management, ensured timely referrals and reduced the number of unnecessary physician consultations (Table 5). Intervention also improved glycaemic control (Table 5 and 6) among participants in the intervention group. A tablet based App programme with action prompts used in this project facilitated patient referral by the health workers to the diabetes clinic and provided a handy list of the referred patients to the physician for review and thus the continuum of care was maintained.
The study was able to demonstrate not only a non-inferiority of the intervention but a significant improvement in diabetes care in low resource settings as compared to the prevailing standard of care. This was indicative in the key processes and outcomes such as case detection rate at the community level, early identification of complications, compliance to structured follow-up, reduction in the unnecessary physician consultation visits overburdening the health system and glycaemic control.
There are published studies from India that have investigated different models of involving health workers in promoting early detection of chronic, non-communicable diseases and adherence to treatment at community level.11 Fathima et al in 2013 reported effective use of health workers who were trained to do house-to-house survey and collect data on risk factors for cardiovascular diseases and reinforce adherence to treatment. The study found that the trained health workers can certainly help with the detection of cases and identify complications using simple checklists.12 However, the feasibility and cost effectiveness of health workers who have multiple tasks to complete, undertaking house-to-house survey in an ongoing healthcare programme is questionable. Another study done in the study site has demonstrated that trained health workers can effectively serve as peer health educators and play an important role in plugging gaps in service delivery including administering point-of-care screening tests on antenatal women at the sub-centers during the once a month doctor led-clinic to detect sexually transmitted diseases.13 Research studies for cancer prevention including the ones done in this study site have demonstrated that health workers functioning as patient navigators could enhance patient-provider communication, advocate for patient’s rights, facilitate decision-making, provide psychological supports and linkages, and provide culturally appropriate services.14–16
Strengths and limitations of the study
The strengths of this study were that existing health care personnel and health systems were utilized in a resource limited setting, to deliver a structured model of care for patients with diabetes in rural communities. Training grass root workers within the community in diabetes care enhanced by digital technology was the strength of this study, while the ‘health education’ and ‘community engagement’ components were the backbone of the success of this model. A good rapport established between the CHWs and the community, transcended the initial barriers to this process such as financial constraints, caste discrimination, health seeking behaviour, stigma associated with diabetes. It is through informed decision making process that the participants were enrolled into the study rather than house-to-house survey. The health workers found the SmartHealth android based App simple to use with an easy user interface. The App worked in the remote areas without internet access, and it was not merely a data entry tool, but one that guided the CHWs to make decisions and timely referrals.
Although a limited sample size was sufficient for proof of concept in this feasibility study, demonstrating a statistically significant difference between groups with more precision/power, requires testing this hypothesis on a larger sample in randomised controlled trial. Moreover the study site has a unique primary health care programme with a strong community outreach and experience, providing care to the rural block for more than 4 decades and therefore the proposed model of CHWs driven diabetes care may be more acceptable in such a setting.
Research implications
This feasibility study in the limited sample size and a small geographic area has shown promising results for task shifting to CHWs trained in diabetes for patient engagement and diabetes care in this rural population. CHWs have successfully been able to Engage, Screen-Examine, Refer and follow-up patients in the community. Since the structure of the Indian public health system has existing community workers such as the ASHAs (Accredited Social Health Activist), USHAs (Urban Social Health Activist) and ANMs (Auxillary Nurse Midwife) and an established primary, secondary and tertiary level care centers, it is prudent to envision that this model can be replicated in other health care settings across India.17 We propose a scale up of this package of interventions by conducting a multicentric randomized controlled trial including a risk-benefit and cost-effectiveness analysis, and taking into account stakeholders’ views and opinions regarding this model of diabetic care.
Acknowledgments
We are indebted to the our research team who worked passionately to complete the study, health workers who were willing to function as patient navigators to improve diabetes management, and to all the participants who responded to our screening invitations and structured care.
Ethics
Approval from the institutional review board of Christian Medical College, Vellore, India was obtained. All study subjects provided written informed consent.
Funding
We acknowledge the funding received from Friends of Vellore, UK and NHS Grampian Endowment fund, University of Aberdeen- Approval Number: EA0852.
Authorship contributions
BB– drafted the manuscript, co-investigator; RI- revised and edited the manuscript, project lead; SP – input to manuscript, co-lead of the project; HRP – patient follow-up and input to manuscript, co-investigator; PA input to manuscript, co-investigator; AP – input to manuscript, co-investigator; NT- input to project conceptualization; JL– input to project and assisted with statistical analysis; JM – input to project and manuscript; PD– input to manuscript, lead tablet android based application; OJ- input to manuscript and co-lead tablet android based application
Competing interests:
The authors completed the Unified Competing Interest Form at www.icmje.org/coi-diclosure.pdf (available upon request from the corresponding author) and declare no competing interests.
Correspondence to:
Rita Isaac
RUHSA Department, Christian Medical College, Vellore
Tamil Nadu, India
[email protected]