Lower respiratory tract diseases remain significant causes of pediatric mortality globally, accounting for 16% of deaths under age five.1–3 The burden of respiratory mortality is greatest in low- and middle-income countries (LMICs) where many health facilities lack sufficient pediatric acute care resources.4,5 Staff in resource-limited facilities must quickly triage patients using available assessment techniques for timely initiation of treatment and potential transfer to higher levels of care. World Health Organization (WHO) guidelines for care of sick children focus on two physical exam findings- tachypnea and chest indrawing- without addressing the multitude of other respiratory assessment tools used by healthcare workers.6,7 The lack of additional validated markers of respiratory distress linked to relevant clinical outcomes makes triage of these pediatric patients challenging.8
Treatment options for pediatric respiratory distress including oxygen, continuous positive airway pressure (CPAP) and high flow nasal canula (HFNC) are increasingly available in LMICs; however, evidence-based treatment algorithms for initiation and use of these therapies are lacking.9,10 Several studies have looked at the correlation of respiratory symptoms or composite scores to important single clinical markers which may indicate therapy is needed. A meta analysis of children with lower respiratory tract infections, however, did not find a single clinical sign or symptom that accurately and reliably identified hypoxemia.11 Although scores of dyspnea are in use to guide management of asthma and bronchiolitis, they have undergone limited and inadequate validation for disease severity.12,13 Additionally, many resource-limited settings (RLS) lack technology to perform advanced diagnostics used to guide therapy, such as blood gas analysis and pulmonary function tests. As pediatric respiratory interventions are deployed in RLS, understanding which respiratory assessments are predictive of poor clinical outcomes could guide management and transfer of care decisions.
The objective of this review is to determine which respiratory assessments in children under five years of age have been associated with poor clinical outcomes in RLS.
Methods
We conducted a systematic review of the literature following the PRISMA checklist.14 We conducted a search for studies published between January 1, 2008 and January 21, 2018 using Ovid MEDLINE (Online Supplementary Document, Appendix S1) and Embase.com. All results were limited to English, German or Spanish languages and ages 0-5. Major categories of search terms were “respiratory distress”, “respiratory symptoms”, “low- and middle-income countries (LMIC)” and “clinical assessment”.
Eligibility criteria
Publications that met the following criteria were included:
-
Took place in a low- or middle-income country as defined by the World Bank, July 2019.15
-
≥ 50% of subjects were under five years of age.
-
Evaluation of subjects occurred in a hospital, emergency department or outpatient clinic setting (not in a home).
-
Respiratory diagnostic assessment, including physical exam, vital sign, laboratory test and/or diagnostic/imaging study, was performed (no parent report symptoms) .
-
Association between a respiratory diagnostic assessment and a poor clinical outcome (including death, clinical course, transfer, monitoring or laboratory result and/or treatment requirement) was reported.
Publications that met the following criteria were excluded:
-
Not original research (comments, editorials, letters and/or notes).
-
Systematic reviews.
-
Case reports or case series with <30 patients.
-
Respiratory diagnostic assessment involved advanced equipment, such as respiratory viral PCR and/or pulmonary function testing.
-
Clinical outcome was a diagnosis, such as pneumonia and/or bronchiolitis.
Data extraction
Citations were managed with Covidence (Copyright © 2019 The Cochrane Collaboration).16 Five reviewers screened and discussed 100 abstracts to reach consensus on inclusion and exclusion criteria. Four reviewers screened an additional 30 abstracts, of which 60% were included/rejected unanimously with an inter-rater reliability of 0.57. Remaining abstracts were screened by one reviewer, and included abstracts underwent full text review. Two reviewers reviewed and reached consensus on inclusion of full text publications and categorization of bias. Disagreement on study inclusion/ exclusion, data selection and bias assessment were resolved by discussion between the two reviewers. If no concensus was found between two reviewers, discussions between all review authors was used to resolve the disagreement. Data was extracted into REDCap (8.11.9- ©2019 Vanderbilt University).17
Assessment of bias
We used the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS) score to objectively evaluate bias in six domains,18 namely:
-
Selection of participants – Selection biases caused the inadequate selection of participants
-
Confounding variables – Selection biases caused by the inadequate confirmation and consideration of confounding variables.
-
Measurement of exposure – Performance biases caused by inadequate measurements of exposure.
-
Blinding of outcome assessments – Detection biases caused by the inadequate blinding of outcome assessments.
-
Incomplete outcome data – Attrition biases caused by the inadequate handling of incomplete outcome data.
-
Selective outcome reporting – Reporting biases caused by the selective reporting of outcomes.
For each domain, a study was determined to have “low risk,” “high risk,” or “unclear risk” of bias according to specific score criteria. Two reviewers performed bias assessment on each publication.
Data synthesis
Given the heterogeneity of publications, a meta-analysis was not performed. In line with the review objective, we focused analysis on publications reporting a statistically significant association between an assessment and outcome for reporting results. The data were summarized descriptively, stratified by country income level.15 When >1 publication described identical study populations (study location, age group, inclusion criteria, study dates), the study population was only included once in Table 2 (summary characteristics). All other analyses report data from each individual publication regardless of population overlap. “Statistical significance” was determined by the authors of the manuscripts.
Results
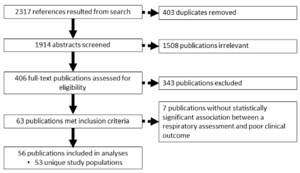
Of 2317 identified publications, 1914 abstracts were screened, and 406 underwent full text review. 343 publications were excluded after full text review because: they did not fit inclusion criteria (79%), no full texts were available (12%) or the content was not relevant (9%). 56 of 63 full text publications reported statistically significant associations and were included in analyses (Figure 1) – representing 53 unique study populations. Kuti19–21 and Chisti22,23 published multiple manuscripts using identical study populations. Two additional publications by Chisti described study populations enrolled during almost identical study periods at the same site and some patients may have been included in both publications.24,25 We did not receive author confirmation about this question, so these populations were considered unique in this analysis. Relevant findings of each publication, stratified by country income level, are summarized in Table 1 (plates A, B and C) with more details found in the Online Supplementary Document, Appendix S2.
General characteristics of unique study populations are described in Table 2. Fifty-five percent of studies occurred in lower middle-income countries, and inpatient general wards was the most common clinical settings. Most studies included infants and/or children 1-4 years, with median patient age of 11 months (when reported). The number of study subjects aged less than 5 years ranged from 65 to 16,162, with a median of 420 (when reported). Bias distribution is shown in Figure 2. The confounding variables domain had the highest risk of bias, with 11% of publications having “high risk” and 39% having “unclear risk”.
Respiratory assessments are reported in Table 3. Some trends by country income existed, for example, chest indrawing was most frequent in upper middle-income countries while low-income countries were most likely to report grunting and nasal flaring. Hypoxia, defined by most studies as oxygen saturation <90%, was the most common respiratory assessment and reported equally frequently among all income levels. Twenty publications reported increased mortality in hypoxic vs. non-hypoxic children with ranges of [(3.8%–29.0%) vs. (0%–7.1%) and odds ratios of (1.6–14.8)]. Nine publications reported prolonged admission or treatment failure in children with hypoxia.
Tachypnea was reported by twenty-six publications (Table 3). Tachypnea was defined by age-appropriate cut-offs in most publications but also as “fast breathing”59 and “abnormal respiratory rate”62 which included high and low rates. Upper middle-income country publications reported associations with tachypnea more often than other income categories and country income was associated with the outcome linked to tachypnea. All seven studies reporting an association between tachypnea and hypoxia were conducted in low- or low middle-income countries.29,33,38,55,59,61,75 Meanwhile the seven studies reporting increased mortality with tachypnea were conducted in low middle- or upper middle-income countries.42,51,54,64,65,71,74 The mortality ranged from 1.7%-10.0% in tachypnoeic children vs. 0.7%-4.1% in non-tachypnoeic children. Two other publications instead reported decreased mortality in tachypnoeic children. Naheed (2009) evaluated 4155 Bangladeshi children 2- 59 months hospitalized with pneumonia and found that 95% of survivors, and 83% of non-survivors were tachypnoeic (P<0.001).58 Non-survivors were more likely to have severe pneumonia, but analyses were not adjusted for severity of illness. Emukule (2014) evaluated 3581 Kenyan children less than 5 years hospitalized with respiratory illness. Sixty-four percent of survivors had tachypnea versus 56% of non-survivors (odds ratio, OR=0.7, 95% confidence interval, CI=0.5-0.9); however, this association was not significant in multivariate analysis.50
Clinical outcomes are reported in Table 4. The most commonly reported clinical outcome was death (54%), followed by hypoxia (23%), length of hospitalization (16%) and treatment failure (13%). Hypoxia was the most commonly reported risk factor associated with mortality (77%), followed by chest indrawing/retractions, (27%) and tachypnea (23%). No trends by income level existed for death, length of hospitalization nor treatment failure. Upper middle-income countries were more likely to report outcomes of general ward admission or need for mechanical ventilation.
Three authors reported risk factors for hypoxia and increased mortality in hypoxemic patients in the same study population. Bassat (2016) evaluated 825 children less than five years of age hospitalized with respiratory distress in Mozambique and found that tachypnea, cyanosis and thoracoabdominal breathing were independently associated with hypoxia, and these hypoxemic children had increased mortality (20% vs. 7%).29 Kuti used a population of 420 Gambian children to report risk factors for hypoxia, including head nodding (35% vs 16%), grunting (61% vs 23%), and cyanosis (20% vs <1%)19 and increased mortality in hypoxic vs. non hypoxic children (40% vs 18%).20 Benet (2017)'s multicenter study of 405 hospitalized children (2 - 60 months old) reported risk factors for hypoxemia including: lower chest indrawing (90% vs. 77%), cyanosis (14% vs. 5%), lack of “rasping” (17% vs 6%), and generalized opacification on chest X-ray (CXR) (44% vs. 28%) as well as higher mortality in hypoxemic children (9% vs 2%).46
Discussion
To our knowledge, this is the first systematic review of markers of pediatric respiratory distress associated with poor clinical outcomes in LMICs. Our findings underscore substantial heterogeneity in the literature related to this topic and this precluded meta-analysis.
This study demonstrates the following key findings: i) hypoxia, chest indrawing/retractions, and tachypnea are the most commonly reported risk factors for child mortality from respiratory disease in RLS; ii) studies in RLS most frequently report death as the primary outcome of pediatric respiratory illness; iii) hypoxia is a key respiratory assessment and outcome of interest in RLS; and iv) few trends exist related to reporting of respiratory assessments or outcomes based upon country income level.
The results of this review serve several purposes for clinicians and researchers caring for children in RLS: With increasing availability of advanced respiratory support (HFNC and CPAP), clinicians need validated criteria for identifying children likely to benefit from this support and/or in need of transfer to higher levels of care.7 It can also help researchers to develop and implement respiratory scores, choosing predictors based upon available resources and patient population.
Hypoxia, chest indrawing/retractions, and tachypnea were the assessments most commonly associated with mortality in this review. This is a reflection likely of a true physiologic association as well as the frequency with which these assessments are performed and studied in these populations. These assessments are in line with World Health Organization guidelines using tachypnea and chest indrawing as indications for antibiotic therapy and for categorization of pneumonia severity.7 A recent meta-analysis from predominantly LMICs found that the strongest predictors of a pneumonia diagnosis in children under 5 years were tachypnea (likelihood ratio, LR=1.9), chest indrawing (LR=1.8) as well as grunting (LR=1.8) and nasal flaring (LR=1.8).76 While evidence-based diagnosis is important for medication treatment including antibiotics and bronchodilators, determining severity of disease is more essential to guide respiratory treatments and transfer decisions. The heterogeneity of poor clinical outcomes in this review has limited the ability to do a meta-analysis, however some systematic reviews have reported associations with specific clinical outcomes. A recent systematic review in infants less than 60 days in RLS found that the strongest predictors of hospital admission were tachypnea (OR=1.5-3.1), grunting (OR=1.5 –2.9), severe chest indrawing (OR=1.5–8.9), and cyanosis (OR=1.5–25.8).77Several of these same exam findings have been previously reported to increase the likelihood of hypoxia: cyanosis (LR=10.4), grunting (LR=2.6), nasal flaring (LR=2.2) and chest retraction (LR=2.6); however authors concluded that “neither single nor combined symptoms and signs have satisfactory performance in predicting hypoxia among young children with acute respiratory infection”.10 Although our findings emphasize the importance of these common respiratory assessments, the heterogeneity in studies makes identifying optimal predictors for variably resourced clinical settings challenging.
Death was the most commonly reported outcome for respiratory disease in this review. Given that over 800,000 children under five died from lower respiratory diseases in 2017, it is not surprising that reducing mortality remains the focus.2 Ongoing inequities in access to respiratory care, such as oxygen and CPAP, contribute to this discrepancy in mortality.78–80 We did not find a trend toward reporting non-mortality outcomes as income level increased, in contrast to high-income countries that have transitioned to reporting predominantly non-mortality outcomes.81–83 This could reflect high mortality rates in upper middle income countries, making death still the most relevant outcome. Alternatively, it may reflect differences in facility-level resources and mortality risk independent of country income level, given known differences in within-country resource availability and access to care. As more regional estimates of disease burden are reported through the local burden of disease project, we may gain understanding of how within country allocation of resources influences outcomes and potential respiratory assessments.84,85
The heterogeneity of reported risk factors and outcomes in this review is not unique to markers of respiratory distress or to RLS. Inconsistencies in measurement and reporting of outcomes are widespread and make it challenging to draw conclusions from many systematic reviews. Many researchers advocate for the development of core outcome sets, which contain a standardized collection of outcomes that should be measured and reported for a particular disease entity.86 Development of a core outcome set for pediatric respiratory disease in RLS would need to involve stakeholders across the resource spectrum to ensure that the agreed upon collection of outcomes are relevant to their settings, similar to approaches used by inFACT, a network of investigator‐led clinical research consortia that aims to promote international collaboration in critical care research and address barriers in undertaking trials.87 A core outcome set could reduce study heterogeneity and improve the ability to use existing data to answer important clinical questions.
This review has a number of limitations. By focusing on publications reporting statistically significant associations with clinical outcomes, we introduced selection bias in addition to existing publication bias favouring significant associations. We minimized this bias by including studies reporting only univariate associations although likely many univariate associations would be not remain significant after multivariate analysis. We used LMICs as a proxy for RLS and categorized studies by country income, which may not equate to comparable resource availability in individual study sites. There was inadequate information about study location (urban vs. rural, national vs. district hospital) or available resources to develop a better stratification schema. We excluded multiple assessments of respiratory illness a priori, including more expensive laboratory or diagnostic tests (PCRs, PFTs), elements of patient history (ie cough) and non-specific danger signs (inability to drink, persistent vomiting, convulsions, lethargy, severe malnutrition) to focus on items most pertinent to respiratory disease in RLS. Only three publications evaluating composite scores were included in this review, which may relate to our search strategy or a paucity of validation of scores in RLS. We excluded specific diagnoses, such as pneumonia or asthma, as valid outcomes because these can be subjective or based on diagnostic criteria that include our assessments of interest (ex. tachypnea for pneumonia). Given the broad nature of the research question, our search strategy identified a large number of abstracts that could only be screened by one reviewer, increasing selection bias. For two publications we were unable to determine if they referred to the same study population, which could affect data in Table 2.
Conclusions
In conclusion, this review emphasizes the importance of hypoxia, chest retractions, and tachypnea as risk factors for mortality while highlighting death as the primary outcome of interest for pediatric respiratory disease in RLS. Given wide variability in clinical settings in LMIC, we were unable to determine consistent, validated markers of pediatric respiratory distress that correlate to poor clinical outcomes. Clinicians and researchers throughout LMIC would benefit from development of a core outcomes set to standardize methodology in future studies. More uniform measurement of outcomes across RLS should allow for more thorough review with meta-analysis to be performed. An analysis like this has the potential to aid clinicians and researchers in identifying which markers of respiratory distress best identify children at highest risk of clinical deterioration and mortality.
Acknowledgements: Susan Groshong, MLIS; Rachel Umoren, MD MS (collaborator); Krystle Perez, MD MPH (collaborator); Maneesh Batra, MD MPH; and Funding for REDCap Server provided by Institute of Translational Health Science (ITHS) grant support (UL1 TR002319 from NCATS/NIH).
Funding: None.
Authorship contributions: AH, AV, KP, KN and RU designed the study. SG carried out the database search. AH, AV, KN, KP and RU (screened abstracts). AH, AV, KG and KN assessed and extracted data from full text articles. AH prepared tables and figures. AH, AV, KG and KN wrote and edited the manuscript.
Competing interests: Author AH is an author of two abstracts in the search. She did not review these abstracts for inclusion. The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no other conflicts of interest.
Correspondence to:
Dr. Anna Hedstrom
4800 Sand Point Way NE
Seattle Children’s Hospital, FA.2.113
Seattle WA 98105
[email protected]
https://orcid.org/0000-0002-3269-1892