On March 11, the World Health Organization declared corona virus disease 2019 (COVID-19) a pandemic,1 indicating wide geographic spread of the infection and sustained community transmission on several continents. While this declaration is meant to sound the alarm for governments around the world to take more aggressive action in their preparedness plans and in their response to the epidemic, the term is accompanied by global anxiety and a fear that, at this stage, containment may not be possible. The delay in declaring a pandemic may even exacerbate the fears that authorities have lost control, and that mitigation is the only way forward.2 About one month since this declaration, close to two million confirmed cases are reported globally, with several countries experiencing rapid epidemic spread and a heavy morbidity and mortality toll. In this viewpoint, we argue that even in settings with considerable community transmission and where the epidemic has entered its exponential growth phase, suppression of the epidemic should still be possible, and should be the aim. In the ongoing COVID-19 pandemic, the epidemic potential and associated health, economic, and social impact are so tremendous that suppression is an unavoidable option.
One of the most critical parameters in an emerging epidemic, the basic reproduction number R0, conveys insights into this potential spread if the infection is left to take its natural course. R0 is the number of secondary infections generated by one case at the beginning of the epidemic. It provides an indication of the intrinsic potential of an infectious agent to spread in a population, since the fraction of the population who would eventually be infected is roughly given by 1-1/R0 (absence of interventions). For COVID-19, R0 has been estimated at around 2.5,3–5 which indicates that the infection could theoretically infect 60% of the population (and even higher in the first wave) - a disease burden that the world cannot afford to carry. Here, we provide a theoretical framework based on epidemiological evidence and quantitative insights to inform intervention strategies to control the epidemic, even at this stage where it has been declared a pandemic.
Based on current understanding, we summarize in Table 1 key parameters that affect the spread of the infection as well directions for their respective containment strategies. Today, scaling up testing and moving towards mass testing (rather than just testing individuals within narrow criteria) is increasingly becoming a promising, if not indispensable, intervention. Mass testing allows identification of “hidden” new clusters, hence helping break chains of transmission within a social network through isolation of identified cases and quarantine of their contacts. Awareness of the existence of the infection in a specific social network can also help “disrupt” network connections where the infection is being transmitted. Additionally, targeted surveillance testing of diverse social networks could be beneficial to identify an outbreak in a given social network, possibly at an early phase of infection transmission. Smart and targeted aggressive testing appears to have been a major player in South Korea’s success in containing their outbreak. With over 500,000 tests performed to date, South Korea has one of the highest per capita testing rates.6 Innovative and pragmatic testing strategies, such as safe and efficient “drive-through” testing stations have facilitated the conduct of up to 20,000 tests per day and prevented economically and socially disruptive mitigation strategies such as complete lockdown.7 With the recent development of rapid antigen tests for COVID-19, mass testing will soon become more feasible - pressure on national laboratories will be alleviated and testing capacity could be significantly expanded in a short duration of time. While the success of mass testing relies on rigorous follow-up with contact tracing that is usually government-led, these efforts could be also initiated by the community, with individuals who test positive referring their contacts for testing and self-quarantine. Such individual-initiated “contact tracing” could play an important role in settings where the infection is spreading at a higher rate than what government-led systems can cope with, such as in the advanced exponential phase of epidemic growth where provision of health care becomes the priority.
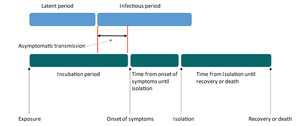
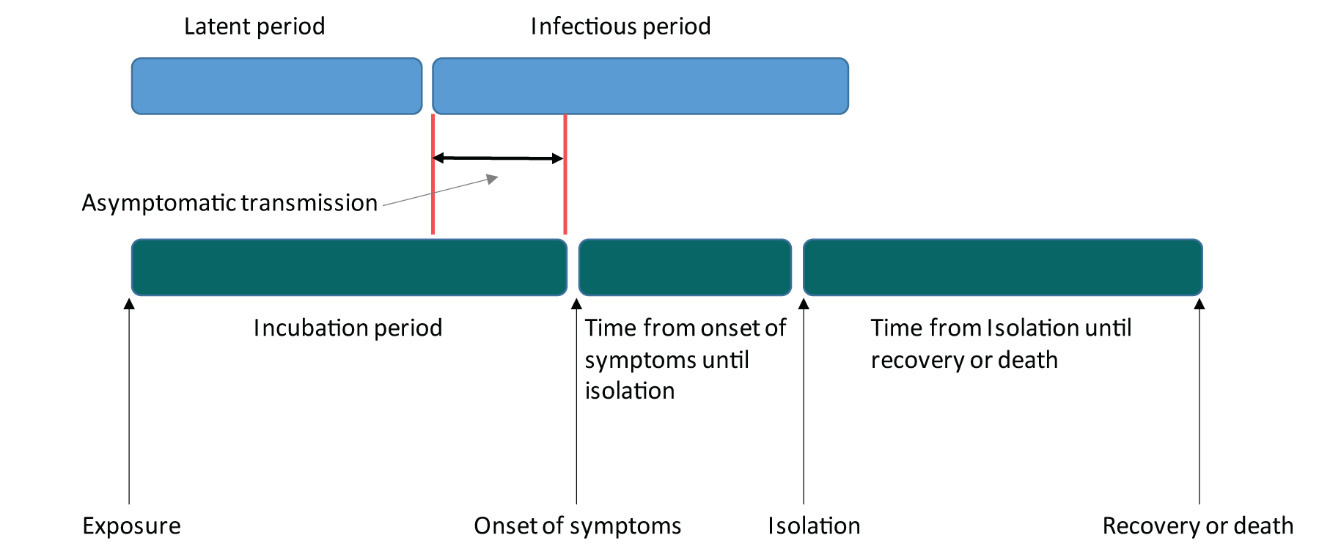
Mass testing followed by contact tracing is key in minimizing the effects of asymptomatic transmission. While earlier reports based on the China data had indicated that the fraction of asymptomatic positive cases who never develop symptoms is limited (about 1%),8 recent evidence from general population screening as well as preliminary findings from the first sero-surveys9–12 suggest otherwise - most infections may be asymptomatic or with symptoms too mild to be recognized. Transmission before onset of symptoms has also been documented13 and, based on limited epidemiologic and clinical data, seems to last 1-2 days,13–15 which is possibly half of the infectious period for this virus estimated at 3.5 days5 (Figure 1). Asymptomatic transmission remains perhaps one of the most critical factors that may complicate containment.5 It has been estimated that a large fraction of infections go unrecognized because of mild, limited, or no symptoms, but play a main role in transmission.5 Proactive case identification, through mass testing and contact tracing, followed by isolation of cases and quarantine of contacts, is needed in order to reduce asymptomatic and other undocumented transmission, a strategy that necessitates robust governmental action with strong individual and collective commitment (Table 1).
With infection transmission expanding worldwide, individual and collective behavior increasingly becomes more critical than government action.15 This takes us back to the definition of R0 expressed simplistically as: Here, is the contact rate, is the probability of transmission per contact, and is the duration of infectiousness. The contact rate and transmission probability can be greatly reduced through personal and collective behavior change. Authorities could still enforce some preventative measures such as lock-downs and bans of gatherings among others; however, each individual has a key role to play by implementing social distancing through limiting their circle of social contacts and number of social encounters (thereby reducing and physical distancing by keeping a minimum distance of 1-2 meters with their contacts (thereby reducing Moreover, reducing respiratory droplet transmission by covering coughs and sneezes, wearing masks, and following recommended hygiene measures (thereby reducing both and are key, as they target main modes of transmission.16–18 These individual behaviors would directly reduce R0 and thus the capacity of the transmission chains to be sustained (Table 1). Immediate self-imposed isolation following onset of symptoms or suspected exposure would effectively reduce the duration of infectiousness, hence also reducing R0 (Table 1, Figure 1). Governments and other concerned public health actors have a critical role in raising public awareness about symptoms and what to do in case of onset of symptoms, as well as in providing necessary diagnostic and clinical follow-up support for isolation; however strong individual commitment is needed to ensure proper implementation and adherence to recommended behavior in terms of reporting, isolation, and prevention of further transmission.
Based on current estimates of R0 at 2.5, at least 60% of transmissions need to be curtailed to reduce R0 to below one, the threshold for epidemic sustainability. This is a large fraction that may seem challenging to achieve given the many setting-specific logistical, system-related, structural, cultural, and other barriers for implementation as well as adherence and sustainability of the containment measures summarized in Table 1. It can be argued that the drastic interventions put in place by the Chinese government, and that were successful in suppressing the epidemic, may be almost impossible to replicate in other countries. However, in truth, what fundamentally matters is the additive effect of the proposed individual interventions. What is required is a combination of interventions where each one of them, even if partially implemented, would compensate for any deficiency in the others. This could be expressed figuratively in the following simplified formula for R0, which incorporates the effects of the intervention strategies put in place as part of a containment plan (Box 1).
Therefore, the total reduction in transmission (due to the addition of the individual reductions) needs to be 60%, a goal which, from this perspective, seems more plausible and could be feasible. For example, if undocumented transmission, the duration of asymptomatic transmission, and the time from onset of symptoms to isolation are reduced each by 30% due to mass testing and contact tracing, and if 30% of individuals engage in social and physical distancing, and if 30% of the infectious droplet transmissions are avoided, R0 with containment would drop to 0.3, which appears to be the value of R0 in China after containment measures were put in place.19 With R0 being below one, transmission chains will not be sustainable, and the epidemic would die out. The additive effect of the proposed strategies is illustrated in Figure 2 through a mathematical modelling simulation of epidemic dynamics.19 The prioritization of the interventions and their individual impact (in terms of reduction in the key epidemiologic parameters) will depend on each setting. For example, if mass testing is not possible due to limited resources and lack of infrastructure, more weight needs to be put in social distancing, physical distancing, isolation of cases, and contact tracing of detected cases.
As the scientific and public health community is learning more about COVID-19 transmission dynamics, it has become almost certain that a vaccine, even if partially efficacious, could be the most reliable intervention in the long-term.20 However, the development and testing of such a vaccine will take at least one year. Manufacturing the vaccine at large scale, distributing it globally, and achieving high coverage is also a gigantic task that is unlikely to be achieved rapidly, as experience tells with other vaccines. The epidemic potential of COVID-19 and the expected toll of morbidity and mortality, even if delayed or spread-out in time by flattening the epidemic curve, is so enormous that suppression using currently available and feasible non-biomedical interventions should be our primary immediate option. Until today, epidemic spread in many countries seems in early stage and suppression is an achievable target. Mathematical modelling21 as well as lessons from China, South Korea, and Singapore have shown that the epidemic can be suppressed even in the exponential growth phase using a combination of interventions. These localized successful suppression experiences have undoubtedly helped contain epidemic spread globally. With more countries moving towards suppression of their local epidemic rather than just mitigation and delay, fighting the pandemic will become a more achievable goal. Although new evidence indicates that perhaps the majority of cases are asymptomatic9–12 which makes containment more challenging, the additive effect of multiple interventions could reduce epidemic transmission below sustainability threshold and remains the most reasonable approach in the absence of a vaccine. With the majority of the population continuing to be susceptible to COVID-19 even after containment of a national epidemic, thoughtful maintenance strategies need to be put in place to prevent epidemic reemergence. This could be done by sustaining the minimal level of interventions needed to remain in place to keep the epidemic below sustainability threshold. Primary responsibility lies on the individual and the community at large to ensure the success of both, suppression and maintenance until a vaccine becomes available and scaled-up. It is time to confront the reality that we live in a new world, where individual and social responsibility should be main pillars. Will this pandemic be registered in history as a pandemic defeated through people’s collective action (a “people’s pandemic”)? Time will tell.
Funding: GM acknowledges support by UK Research and Innovation as part of the Global Challenges Research Fund, grant number ES/P010873/1. Rest of authors acknowledge support by NPRP grant number 9-040-3-008 and NPRP grant number 12S-0216-190094 from the Qatar National Research Fund (a member of Qatar Foundation). The statements made herein are solely the responsibility of the authors.
Authorship contributions: GM co-led the conceptualization, conducted the literature search, and wrote the first draft of the manuscript. HA conducted the mathematical modelling simulations and contributed to the conceptualization. MM, SS, and HC contributed to the conceptualization. LJA co-led the conceptualization and contributed to the mathematical modelling simulations. All authors contributed to the writing of the manuscript.
Competing interests: The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest
Correspondence to:
Ghina R. Mumtaz, PhD
American University of Beirut
P.O.Box 11-0236, Riad El Solh
Beirut 1107 2020, Lebanon
Tel: +961-1-350000 Ext: 4652
[email protected]
Professor Laith J. Abu-Raddad
Weill Cornell Medical College
Qatar, Qatar Foundation - Education City
P.O. Box 24144, Doha, Qatar
Tel: +(974) 4492-8321. Fax: +(974) 4492-8222
[email protected]