Cardiopulmonary resuscitation is regarded as a simple and effective method of treating cardiac arrest when promptly and correctly carried out.1 Paediatric Advanced Life Support (PALS) is a specialized training developed by the American Heart Association (AHA) for emergency care of infants and children.
In Low- and Middle-Income Countries (LMICs) such as Nigeria, issues such as under-reporting of cases and paucity of data limit reliable estimates of the incidence of sudden cardiac deaths in children and infants.2 In general, survival after “sudden cardiac arrest remains unacceptably low at less than 10% in most parts of the world”.3 Physicians who routinely manage paediatric emergencies are expected to undergo PALS training.
Paediatric emergency care in Nigeria faces numerous challenges, ranging from inadequate infrastructure to a shortage of trained healthcare professionals. The country’s healthcare system struggles to meet the demands of its growing population, with children being particularly vulnerable. Emergency preparedness in Nigeria’s healthcare facilities, particularly for paediatric care, is generally inadequate. In one survey of children’s emergency rooms at 9 tertiary hospitals in southern Nigeria, only 5 (55.6%) had doctors and nurses with training in emergency triage, 5 (55.6%) had doctors with certification in emergency care, but none had a nurse with certification in emergency care.4 In another report of 34 tertiary-level paediatric emergency departments across Nigeria, none of the heads of the emergency department had a specialist or fellowship qualification in emergency medicine, or a sub-specialty fellowship or certificate in paediatric emergency medicine.5 In that report, some professionals are unable to perform high-quality CPR, and or lack the knowledge and skill to carry out PALS, having never undergone any formal session of PALS training. Many of the professionals have either never received formal PALS training or have been trained with long elapsed certification periods.
The absence of regular training and certification programmes in paediatric life support results in a workforce that is not adequately prepared to handle paediatric emergencies, significantly impacting patient outcomes. The impact of inadequate paediatric emergency care is reflected in Nigeria’s high child mortality rates, with the country having one of the highest under-five mortality rates in the world, at 117 deaths per 1,000 live births in 2020.6 Many of these deaths are potentially preventable with timely and adequate emergency care.
To begin to address these shortcomings, Nigeria has prioritized emergency preparedness and life support in her National Surgical, Obstetric, Anaesthesia and Nursing Plan (NSOANP).7 In collaboration with a cleft-focused organisation (Smile Train Incorporated, New York), NSOANP deployed PALS training across the country beginning from 2021. The objective of this report is to show the scope and short-term outcome of PALS training in Nigeria and is intended to highlight the potential role of life support training in strengthening children’s surgical safety and outcomes in low resource settings.
METHODS
This is a retrospective review of the PALS training conducted between May 2021 and November 2023. The trainings were conducted at 6 locations across the country, in Abuja (north central zone), Lagos (south west zone), Kano (north west zone), Gombe (north east zone) Enugu (south east zone), and Port Harcourt (south south zone), representing the 6 geopolitical zones of Nigeria.
Participant Selection
The target population for the training was senior level doctors who routinely deal with paediatric emergencies. Participants were selected from specialized cleft care treatment centres, as well as public tertiary hospitals based on their involvement in cleft lip and palate, and children’s surgical care. Participants were nominated by the geopolitical zone lead for cleft lip and palate care to ensure geopolitical spread. The nomination of participants was based on the following criteria:
- Must be a physician
- Involvement in the surgical care of children or providing anaesthesia for children
- Interest in participating in the PALS training programme
Training
Provider training
The training was structured according to AHA requirements. All participants had undergone training in basic life support before progressing to PALS training.
Details of the training involved the following:
-
Selected participants received the PALS student manual at least 3 weeks before the training to study ahead of the training.
-
Participants completed a validated online-based pre-test before commencement of the training and must achieve a minimum score of 70%. They can take the test multiple times as long as it’s done before commencement of the training.
-
The training was an intensive 3-day training programme including lessons and multiple skills acquisition sessions involving basic life support skills for infant and child and, respiratory, cardiac and vascular access skills. These specifically included management of respiratory emergencies, management of cardiac emergencies and management of shock in the form of case scenarios and practice with simulation.
Instructor training
This was a 2-day onsite training of participants who had previously undertaken training in basic life support (BLS) and PALS with excellent performance. As part of the training, they were required to teach BLS and PALS under supervision of the instructor faculty.
Data Management
Data Collection Procedures
Pre-test was done online by each participant. Data on post- test were recorded during the training for each training group and uploaded to ATLAS, the AHA certification platform. A paper-based survey in the form of a 5-point Likert scale was administered to participants to obtain information on their experience as well as their comments regarding the training. A WhatsApp group was created for communication with participants as well as to track their experience and step-down activities after training.
Data Analysis
The data was analyzed using the Excel Analyse-it® statistical software. The difference in pre-test and post-test scores was analysed using the Wilcoxon sign rank test and level of significance set at p <0.05. The 5-point Likert scale for feedback responses were collapsed to a 3-point scale for the purposes of analysis. The data is presented as descriptive information.
RESULTS
Overall, one provider training has been completed at north west, north east, south west, south south locations, 3 at south west and 2 at north central locations. One instructor training has also been completed.
Provider Training
There were 106 participants, including 67 (63.2%) males and 39 (38.6%) females, from across the 6 geopolitical zones (Figure 1).
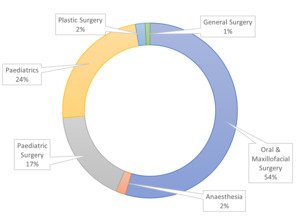
The participants were from diverse specialties with responsibilities for paediatric patient care, but most (54.5%) were anaesthesia specialty (Figure 2). Seventy-five (70.8%) participants were consultants, 30 (28.3%) trainees and one (0.9%) a medical officer. All 106 participants passed the post-test and were certified by AHA.
Participants’ Performance
The pre-test scores were 73% - 98% (median 81%) compared to the post-test scores of 84% - 98% (median 92%). The difference between the pre-test and post-test scores was statistically significant at p = 0.003.
Participant Feedback
All participants (100%) agreed that their skill in operating a manual defibrillator had improved. All participants (100%) agreed that they were more confident in their ability to properly handle emergencies in children. They all agreed that using the systematic approach of “Evaluate- Identify- Intervene” prevents omission of critical signs and reduces delay in intervention. Overall, the participants (100%) were satisfied with the quality of training, the diligence of trainers, and impact of the training. The participants were willing to step down their newly acquired skills to other staff at their respective institutions.
Instructor Training
During the period, 2 instructors (one anaesthetist and one paediatrician) have been trained. Since training, both instructors have been involved in conducting 12 BLS provider trainings and 8 PALS provider trainings at different geopolitical zones of the country.
DISCUSSION
Deployment of the Paediatric Advanced Life Support (PALS) training programme as part of implementation of Nigeria’s NSOANP is an important step in addressing the critical need for improved emergency paediatric care and safe surgery for children in the setting.
The PALS training programme has demonstrably improved the knowledge, practical skills and confidence of healthcare providers in managing paediatric emergencies, as all 106 participants successfully passed the post-test and received certification. One report has previously found that PALS course significantly increased immediate short-term knowledge of paediatric resuscitation amongst physicians, nurses and paramedics.8 In one study at tertiary hospitals in Nigeria, a global but remediable deficiency in emergency care preparedness amongst paediatric emergency departments was reported. That report highlighted the need for training in basic and advanced life support.5 The success of our training is crucial, given the reported deficiencies in paediatric emergency care skills among healthcare providers in Nigeria. The unanimous feedback from participants about their ability to operate manual defibrillators and manage paediatric emergencies further highlights the effectiveness of the training programme. The adoption of the systematic “Evaluate-Identify-Intervene” approach by all participants is encouraging. This methodical approach is designed to prevent the omission of critical signs and reduce delays in intervention, which are common issues in the chaotic environment of paediatric emergencies.9
The reach of the training programme across Nigeria’s six geopolitical zones ensured a broad and inclusive impact. By selecting participants from diverse regions and specialties, the programme is potentially addressing the disparity in emergency care skills and knowledge across different parts of the country. This geographical spread is essential for building a robust emergency care network capable of delivering high-quality life support care to children regardless of their location.
NSOANP has planned to gradually expand the PALS training to all members of the healthcare sector who are involved in the treatment of children, including emergency room physicians, general medical practitioners as well as paramedics. This is intended to broaden the reach and impact of the programme. In addition, it is recommended to integrate such training programmes into the curricula of medical and nursing schools in Nigeria and similar settings. Future iterations of the training would leverage technology to maintain continuous engagement and professional development. To expand and sustain the programme, NSOANP is doing the following:
- Encouraging those trained to step down and conduct such skills training at their respective institutions. To this end, NSOANP has planned to engage with the administrations of these institutions to support such trainings.
- NSOANP is continuing to seek additional funding to expand and sustain the training.
- Strengthening life support training and skills continues to be a key priority of the NSOANP policy, which is now being revised to focus on the next 5 years.
Limitations
A limitation of this study is that it reports on the training of a small number of healthcare providers involved in the surgical care of children, out of the larger number of paediatric related healthcare providers in Nigeria. However, following the success of the training programme, NSOANP has planned to gradually expand the training to involve a larger number and wider spectrum of paediatric-related healthcare providers. Although this report has not yet evaluated the actual clinical impact of the training on emergency paediatric care in the country, NSOANP plans to include this as the training is gradually expanded.
Recommendation
The PALS training programme is effective in ensuring acquisition of life-saving paediatric emergency care skills by physicians involved in children’s care. We recommend that this training should be part of the routine skills training for healthcare providers involved in the treatment of children.
CONCLUSIONS
The PALS training initiative under NSOANP has enhanced the emergency care skills of healthcare providers, thereby contributing to safe surgery in children. The programme’s success underscores the importance of structured and targeted training in improving healthcare delivery in resource-limited settings. Continued efforts to expand and sustain such training programmes are essential for building a resilient healthcare workforce capable of addressing paediatric emergencies effectively.
Acknowledgements
We are grateful to Drs. Chisom R. Udeigwe-Okeke and Mohammed AS Abdullahi, and Mrs. Ngozi Opara for their useful suggestions during the preparation of this manuscript.
Ethics statement
Ethical approval was obtained from the institutional review board (health research and ethics committee) of National Hospital, Abuja, Nigeria, as part of Nigeria’s NSOANP creation and implementation process. In addition, participants were informed that participation in the training was voluntary and accepting to participate implied consent to participate, but no written consent was obtained.
Funding
The PALS training programme was funded by Smile Train Inc., New York, as part of their support for the implementation of Nigeria’s NSOANP.
Authorship contributions
AOO contributed to the analysis and interpretation of the data, AND drafting of the manuscript AND final approval of the version to be published AND agreement to be accountable for all aspects of the work; ONA contributed to the analysis and interpretation of the data, AND drafting of the manuscript AND final approval of the version to be published AND agreement to be accountable for all aspects of the work; JOS contributed to the analysis and interpretation of the data, AND drafting of the manuscript AND final approval of the version to be published AND agreement to be accountable for all aspects of the work; NO contributed to the conception and design of the work, analysis and interpretation of the data, AND reviewing the manuscript critically for important intellectual content AND final approval of the version to be published AND agreement to be accountable for all aspects of the work; EAA contributed to the conception and design of the work, analysis and interpretation of the data, AND reviewing the manuscript critically for important intellectual content AND final approval of the version to be published AND agreement to be accountable for all aspects of the work
Disclosure of interest
Nkeiruka (Nk) Obi is a staff of Smile Train Inc., which funded the PALS training programme. She contributed to the conception, drafting, review and final approval of the manuscript for publication.
Correspondence to:
Professor Emmanuel A. Ameh
Department of Surgery, National Hospital, Abuja
Nigeria
[email protected]