Absent or reduced fetal movements (ARFM) are reported to occur in 4-18% of pregnancies1 and studies in high income countries (HICs) have shown an association with adverse perinatal outcomes including stillbirth,2,3 preterm birth and fetal growth restriction (FGR).2 A recent Confidential Enquiry in the UK found that maternal presentation with ARFM occurred in 28% of intrapartum perinatal deaths, and suboptimal care was evident in 33% of cases4 highlighting the importance of appropriate management of ARFM.
Diagnosis of ARFM may occur following maternal perception or can be defined using tools such as “kick charts”. Observational studies report that fetal movement counting is associated with better identification of FGR and a reduction in infants born with Apgar scores <4 at 1 minute,5 and interventions for ARFM may reduce the incidence of stillbirth without any associated increases in other adverse maternal or neonatal outcomes.6 However, data from randomised controlled trials are not sufficient to determine whether “kick charts” or management of ARFM can reduce mortality or morbidity.7,8 Furthermore, it is not currently known whether the results of studies in HICs are applicable to low and lower-middle income countries (LMICs) that have higher stillbirth rates.
To meet the goals for stillbirth reduction in LMICs outlined in the Every Newborn Action Plan, strategies are needed to identify fetal compromise and to institute appropriate action. ARFM may represent a means to detect fetal compromise in low-resource settings. Thus, knowing the incidence of ARFM, its association to adverse pregnancy outcomes, and if any clinical interventions are effective could aid development of optimal methods of screening for fetal compromise in LMICs. Currently, the World Health Organization recommends that care providers enquire about ARFM at each visit and that women who perceive ARFM should be monitored.9
The aim of this scoping review was to assess the current literature on ARFM in LMICs, the objectives of this review were to determine: i) the frequency of adverse pregnancy outcome after presentation with ARFM in LMICs and if there are investigations or clinical factors that predict this; ii) what women’s experiences are regarding the perception of fetal movements and their subsequent care and if there are any specialised management strategies in place; and iii) the extent of knowledge of women and care givers in LMICs with regard to ARFM as a potential cause of adverse outcomes in pregnancy.
A scoping review was chosen as this methodology allows broad inclusion criteria, thereby facilitating the reporting and analysis of as much relevant data as possible, even when meta-analysis cannot be performed.10 This approach was taken as it gives an idea of the number of studies addressing ARFM in LMICs and a view of the total body of research evidence.
METHODS
Following the methodological framework outlined by Arksey & O’Malley,11 preliminary searches were conducted in African Journals Online (AJOL) to evaluate the types of published studies and to help identify research questions. Using keywords and reference lists of papers identified by these searches, systematic searches were performed in MEDLINE, Web of Science, Google Scholar, LILACS, and AJOL from database inception to 2018. An example search strategy is included as Appendix S1 in Online Supplementary Document (Online Supplementary Document).
A systematic approach was taken to screening and data extraction; titles and abstracts resulting from our searches were screened according to our inclusion criteria and relevant studies were identified. Inclusion criteria were kept broad so as not to exclude any potentially relevant studies. The overall concept of interest is pregnancies in which there is maternal perception of ARFM; consequently studies that evaluated knowledge and/or practice in relation to ARFM were included, as were studies of the outcome of pregnancy after ARFM. Studies of interventions (whether this is specialised management, monitoring or admission, or induction of birth) for ARFM were also included. In this study, ARFM was defined by maternal perception or clinical diagnosis (e.g. use of a kick chart) after 28 weeks of gestation. Screening was performed by two authors (DH and AH) and any disagreements were resolved by consulting with a third author (RS). Reference lists of included studies were checked for other relevant studies. Countries were classified as LMICs based on the World Bank classification of income status.12
Our primary outcome of interest was antepartum stillbirth, defined as death of a baby after 28 weeks of gestation or with a bodyweight of >1000g before birth.13 Secondary outcomes were alternative measures of fetal wellbeing: low Apgar score (<7 at 5 min); small-for-gestational-age (SGA) defined as birthweight below the tenth centile for gestational age or as described by individual studies; preterm birth < 37 weeks; neonatal unit (NNU) admission; umbilical artery pH <7.05 or BE >-12; low birthweight (<2.5kg); very low birthweight (<1.5kg); maternal outcomes were birth by caesarean section and postpartum haemorrhage (PPH).
Data were extracted using a piloted form by two authors independently (DH and AH); discrepancies were resolved through discussion with a third author (RS). Qualitative data in relation to women’s knowledge or experiences of ARFM were tabulated and/or recorded narratively. Where possible, meta-analysis was performed, overall proportions and 95% confidence intervals were calculated for each outcome in women with and without ARFM. I2, a statistic derived from Cochran’s chi-squared statistic Q, was used to describe the percentage of between-study variation that is attributable to variability in the true treatment effect.14 An I2 value of 0-30% was classified as low, 31-60% as moderate, 61-90% substantial, and 91-100% considerable.15
Meta-analysis was performed in STATA version 14 (StataCorp, TX, USA) using the metan16 and metaprop17 commands. Random effects meta-analysis was used in anticipation of heterogeneity between studies caused by differences in design. When necessary, analyses of proportions were conducted using a continuity correction to allow for the inclusion of studies with 0% or 100% values.17 The review was registered prospectively on PROSPERO (CRD42018088635).
RESULTS
Literature searches retrieved 729 abstracts, of which 34 full text papers were obtained after screening based on titles and abstracts (Figure 1). After evaluation of full text papers against the inclusion criteria, 19 studies were included. Twelve studies reported data on women’s knowledge of fetal movements18–29 and seven included quantitative data.30–36 One author was contacted for information36; however additional relevant data were not available.
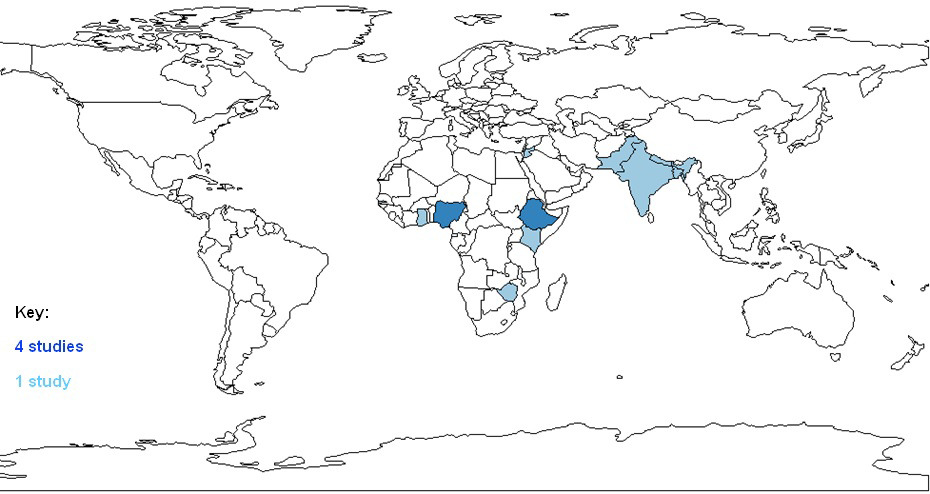
Included studies were from 11 countries: Ethiopia, the Gambia, Nepal, and Zimbabwe (LICs); Bangladesh, Ghana, India, Jordan, Kenya, Nigeria, and Pakistan (LMICs) (Figure 2). Characteristics of included studies for quantitative data are described in Table 1. Four studies used a case-control design and three were cohort studies. Four studies defined ARFM by maternal perception with the two oldest studies (both published in 1988) employing fetal movement counting charts. Six studies reported data for our primary outcome (stillbirth); four in women with and without ARFM and two in ARFM cohorts only. Three papers also reported data for at least one of our secondary outcomes and one paper reported data for one secondary outcome alone.
Data regarding the incidence of stillbirth in ARFM pregnancies and in those with normal movements were extracted from five studies,30–34 comprising 1466 pregnancies of which there were 296 stillbirths. Including all studies, the likelihood of stillbirth was significantly higher in pregnancies with ARFM (OR 14.13; 95% CI 3.46 to 57.77) than without. There was substantial heterogeneity between studies (I2 = 75.9%, P<0.005) (Figure 3), which was likely due to data from the study by Singh & Sidhu (2008). Removing this study from the analysis gave an OR of 6.47 (95% CI 2.45 to 17.04) with an I2 of 51.2% (P=0.10). We were unable to compare the likelihood of other secondary outcomes in ARFM pregnancies to those with normal fetal movements due to a lack of information.
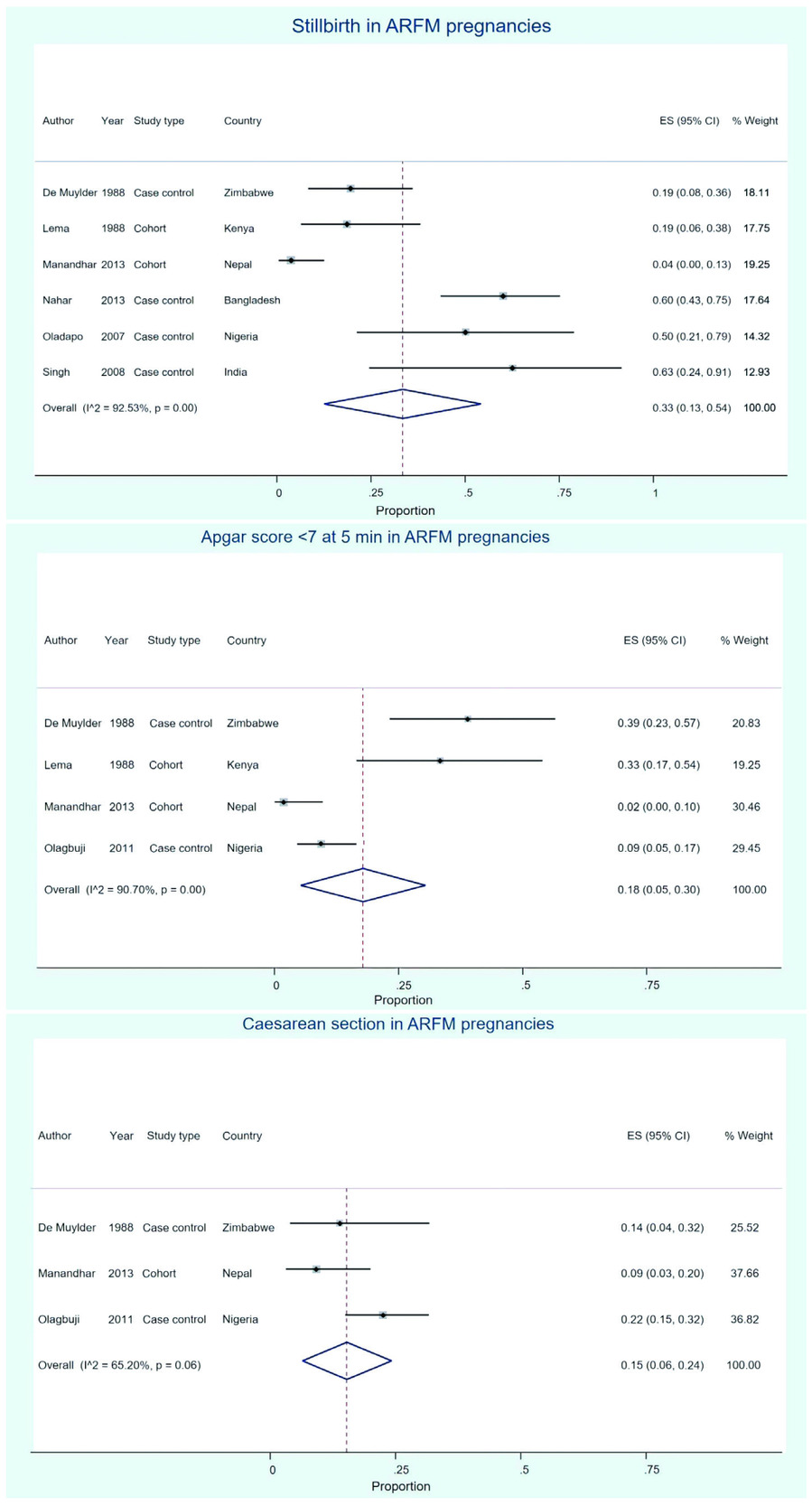
Data for the proportion of pregnancies ending in stillbirth in pregnancies with ARFM was extracted from six papers30–35 comprising 49 stillbirths from 178 pregnancies. Two of these studies were cohort studies of ARFM pregnancies and from the others we used data from the case arm of case control studies. The control group was used from the Singh & Sidhu (2008) study as there was no intervention for ARFM. The overall proportion of stillbirth in ARFM pregnancies was 0.33 (95% CI 0.13 to 0.54, I2=92.53%, P<0.005; Figure 4, panel a) i.e. 33% of ARFM pregnancies resulted in stillbirth.
Data for the incidence of low Apgar score (<7 at 5 min) were available on 225 pregnancies from 4 studies.30,34,35,37 The proportion of low Apgar scores was 0.18 (95% CI 0.05 to 0.30) in pregnancies with ARFM. Again, overall heterogeneity was considerable (I2 = 90.70%, P<0.005; Figure 4, panel b).
Data on the frequency of caesarean section in ARFM pregnancies were available from three papers34,35,37 reporting the outcomes of 191 pregnancies. Only caesarean sections for fetal distress were included, any procedures that were elective or performed for other reasons were excluded from this analysis. The overall proportion of caesarean section in women reporting ARFM was 0.15 (95 CI 0.06 to 0.24, I2= 65.20%, P=0.06; Figure 4, panel c).
NNU admission was recorded by two studies.35,37 Olagbuji37 reported an incidence of 7.5% from 107 pregnancies in their cohort of pregnant women who underwent induction for ARFM and Manandhar35 reported an incidence of 20% from a cohort of 55 women with ARFM, in which there were two perinatal deaths.
Two papers30,37 recorded the incidence of birthweight <2.5kg; both of these studies found a significantly higher incidence of low birthweight in pregnancies with ARFM; Lema30 found an incidence of 46.8% in 27 pregnancies with ARFM compared with 22.4% of the total population (n=110) and Olagbuji37 found an incidence of 11.2% in 107 women who were induced for ARFM compared with 2.8% in 107 women who were induced for prolonged pregnancy (who had no evidence of ARFM).
No formal meta-analysis for studies that intervened based on ARFM status could be performed because the interventions and study methods were not comparable (Table 2). Interventions included screening for fetal compromise using cardiotocography, ultrasound fetal biometry, induction of labour and birth by caesarean section. In one study where women with ARFM were induced with misoprostol37 the proportions of babies born with a 5 min Apgar score <7 was lower than in our pooled analysis (9.3% vs 18%) and the proportion of caesarean sections was higher (38% vs 30%); there were no stillbirths.
Twelve studies used interviews and/or questionnaires, many of which were structured and pretested, to report women’s knowledge of ARFM as an obstetric danger sign. We found no studies reporting care givers’ knowledge of ARFM. The percentage of women who were aware of ARFM as a danger sign in each study ranged from 3.1% to 62.3%, reported in Table 3. In general, studies did not report women’s source(s) of information about ARFM although the numbers of antenatal clinic visits as well as the care provider were commonly reported. One study28 stated that 80.4% of women recalled their care providers enquiring about their perception of fetal movement. Women’s main sources of information were doctors (53.3%) or nurses (46.2%) and 18.2% of women only received information from family and friends, or via the internet or media.
DISCUSSION
This is the first review of studies of women’s knowledge of ARFM in LMICs and related adverse perinatal outcomes; we have highlighted the relative paucity of literature on this topic relative to HICs and identified gaps that should be the focus of future research.
This review is strengthened in that it was conducted following pre-specified eligibility criteria in accordance with a registered protocol. Limitations of this study include that the lack of literature restricts our ability to draw robust conclusions from this review, particularly with respect to studies that looked at ARFM in relation to our desired outcomes. We also did not find any studies that recorded women’s knowledge of ARFM in association with stillbirth, meaning that we were not able to meet all our objectives.
Data from studies of adverse outcomes showed that the likelihood of stillbirth was significantly higher in ARFM pregnancies compared to those without ARFM. This finding is consistent with studies in HICs.2,3,38 All of our included studies showed a higher likelihood of stillbirth in ARFM pregnancies, regardless of study methodology or how ARFM was defined. These data suggest that ARFM should be recognised as a risk factor for stillbirth in LMICs.
The overall proportion of stillbirth in ARFM pregnancies (0.33, 95% CI 0.13 to 0.54) is very high. The highest estimated stillbirth rate in one of our included countries, for example, is Bangladesh at 35.6 per 1000 births.39 The observed proportion of stillbirths is likely inflated by the inclusion of case control studies, meaning that the overall incidence of stillbirth in our included studies is higher than that of in the general population. The proportion of pregnancies ending in stillbirth was also higher than our reported proportions for low Apgar score or caesarean section rate. However, not all studies reported all outcomes, so these proportions may not be directly comparable. Critically, not all studies reported whether all stillbirths occurred following maternal perception of ARFM with a live fetus at first assessment or whether ARFM was the presenting symptom of stillbirth. One study reported that three of five stillbirths were diagnosed on presentation with ARFM30 and in another33 this number was five out of eight; in others this was not reported.
In HICs, ARFM is the single most common presenting symptom (in 44-55% of stillbirths). Thus, if it was the latter case, then ARFM may be useful to make a more prompt diagnosis of fetal death in utero which could avoid maternal complications. If it was the former, then ARFM could be a symptom of fetal compromise to prompt intervention.
The proportion of other outcomes such as SGA or preterm delivery in ARFM pregnancies, or their likelihoods in ARFM versus non ARFM pregnancies could not be examined. We were also unable to investigate the effect of income status, ease of access to care, education, and whether the community in each study is urban or rural on ARFM. From a clinical perspective, each study area should be considered individually, taking combinations of these factors into account.
Critically, we did not identify any studies which investigated whether increased levels of knowledge regarding ARFM resulted in increased presentation to maternity care providers or reduced adverse outcomes in LMICs, although one paper28 reported that 62% of women with correct knowledge of ARFM would seek healthcare assistance if they perceived ARFM. In addition, no studies were found that directly addressed women’s experiences of maternity care after perception of ARFM or of clinicians’ knowledge and views about ARFM; these represent important gaps in the evidence base which need to be addressed as studies in HICs describe that women’s concerns regarding ARFM may be dismissed by clinical staff.40 Robust studies are also needed to determine whether improved knowledge of ARFM is associated with improved pregnancy outcomes in LMICs.
The limited data available from studies of interventions based on ARFM status suggest that this may be a worthwhile strategy for prevention of adverse perinatal outcomes in LMICs. One study of 200 high risk pregnancies34 monitored most women after they had abnormal kick charts (some were allowed to go home and told to return weekly or if kick counts were low). All women experiencing ARFM pregnancies were supposed to be induced or birth achieved by caesarean section; of the 20 ARFM pregnancies with abnormal kick charts where action was taken there were no antepartum stillbirths (although there was one neonatal death due to meconium aspiration). When no action was taken for ARFM (apart from one caesarean section due to fetal distress) taken there were seven antepartum stillbirths (n=16). Another study33 gave kick charts to 250 women; 15 were admitted for ARFM and screened using ultrasound and a non-stress test. Women with satisfactory test results were discharged; otherwise induction took place if indicated. There were no fetal deaths in this group. Another study30 did not present outcomes separately for women who were delivered due to ARFM. One of our included studies37 measured outcomes in 107 women who were induced for ARFM; incidence of stillbirth was not mentioned but there were no early neonatal deaths or low Apgar scores and 8 NNU admissions in this group. There were also two caesarean sections performed for non-reassuring fetal heart tracing; the lower incidence of adverse outcomes may be due to increased monitoring and surveillance.
Our included studies show that research in to women’s knowledge of ARFM has been carried out in both low income and lower middle income countries; Ethiopia was a particular focus for this research with four included studies,18,21,22,25 two of which18,21 were in the same city and over a similar timeframe. Included studies mostly looked at ARFM as a danger sign in pregnancy rather than as a direct link to stillbirth or other adverse outcomes, although one study28 details that 16.4% of 225 women mentioned that stillbirth could arise as a variation from average fetal movement. We also found a number of manuscripts that reported the numbers of women who could identify a certain number of danger signs but did not specify which; it is possible that some mentioned ARFM but we were unable to use data from these papers in this analysis.
A lack of overlap between study populations meant that we were not able to directly compare women’s knowledge of ARFM and the incidence of stillbirth, which could be addressed in future studies. Low levels of awareness (less than 50% of women were aware of the risks associated with ARFM or named ARFM as a danger sign in 10 out of our 12 included studies) could have led to an underestimation of the effect size.
The percentage of women in each study who were aware of ARFM as a danger sign also varied greatly, this variation could arise from a number of factors. Most studies did not identify sources of information about ARFM which could be useful in determining if the type of care, access to care, or care provider has an effect on maternal awareness of ARFM. Importantly, making multiple ANC clinic visits has been linked to increased awareness of danger signs25; this may also underpin the differential effects in urban and rural communities due to access to care. However, only one of our included studies addressed this question19 and found no significant difference in women’s knowledge of ARFM between the different areas. Women with previous pregnancies may also be more aware than nulliparous women; again data were not sufficient for analysis. Importantly, outside factors affecting women’s knowledge may have increased in frequency in the past ten years; one of our included studies23 found that having a working television or radio was associated with knowledge of multiple danger signs of pregnancy. However, there was no clear pattern in terms of location or year of study and their relation to knowledge, but some of the lower percentages were from studies conducted over ten years ago. Further studies are needed to determine whether knowledge in these areas has improved over time, and the most effective ways of giving information about ARFM to women in LMICs.
CONCLUSIONS
The data that are available suggest that awareness of ARFM is an area that should be targeted for improvement, especially as we found an association between ARFM and stillbirth which was comparable to or stronger than that seen in HICs. Future intervention studies with larger sample sizes are needed to look at the effect of admission and further testing for women with ARFM to see if the overall stillbirth rate decreases or is smaller than the estimates found here. Although evidence regarding the usage of kick charts is inconclusive7,38,41 in countries where awareness and resources are low fetal movement counting could be a worthwhile and simple way of defining ARFM in terms of whether further action should be taken.
Correspondence to:
Dexter Hayes
Maternal and Fetal Health Research Centre
5th Floor
St. Mary’s Hospital
Oxford Road
Manchester M13 9WL
UK
[email protected]



_pregnancies.png)


_pregnancies.png)