Reliable information on the causes of death can help identify health care priorities, allocate resources as well as to design, monitor and evaluate the outcomes of healthcare interventions.1–3 Most mortality surveillance systems in developed countries rely on medical certification.3 However, in developing countries like India, there are several challenges to obtain information on cause of death.3,4 About three-quarters of all deaths occur at home in India, particularly in rural areas and cause of death remains unknown for more than 50% of these.4 The global picture is not very different and it is estimated that close to one in two deaths go unrecorded in terms of cause of death.2 Verbal autopsies have been used to ascertain cause of death in resource poor settings in India and elsewhere where deaths occur at homes and are medically unattended.2,4 Verbal autopsies use information on symptoms and signs of the diseases and events preceding death to ascertain cause of death.5 The information is gathered from a relative or a carer of the deceased by trained personnel using a standardized tool. This system is particularly useful for providing information about broad disease categories causing deaths and has been used in many countries to assess causes of deaths in specific populations such as children and mothers, for mortality surveillance and to assess the effect of health interventions.6,7
Two thirds of India’s population and 12% of the world’s population lives in rural India. However, information on causes of deaths sepcifically for rural areas of India is rare. There are few studies but these are from relatively affluent or peri-urban rural areas.8,9 The Sample Registration System (SRS) of India is the only source of nationally representative mortality data which also uses verbal autopsies to ascertain cause of death. The SRS covers a population of about 7.5 million which is less than 1% of the population of India.4,10 It has recently reported the causes of death for India for years 2010-13.10 Although this report did provide data on causes of death from the underdeveloped states it did not do so separately for rural regions where the challenges to healthcare delivery are maximum.10 Also, the India State-Level Disease Burden Initiative recently reported modeled estimates for the causes of death in India for year 2016 using the method developed by the Global Burden of Disease study.11 While these studies provide a national picture, and, to some extent, that in the underdeveloped states, information on causes of death from rural regions and particularly underdeveloped rural regions remains missing. This information is extremely important as the populations in such regions remain vulnerable to preventable mortality and would benefit significantly from priority-driven healthcare response to address emerging healthcare challenges and assess progress towards Universal Health Care.
In this community-based study, we determined causes of deaths prospectively using a well-validated verbal autopsy tool in rural areas of Gadchiroli, one of the most underdeveloped districts of India.12
METHODS
Study area
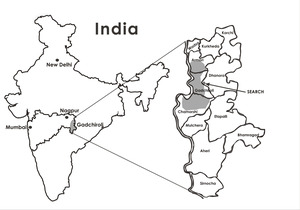
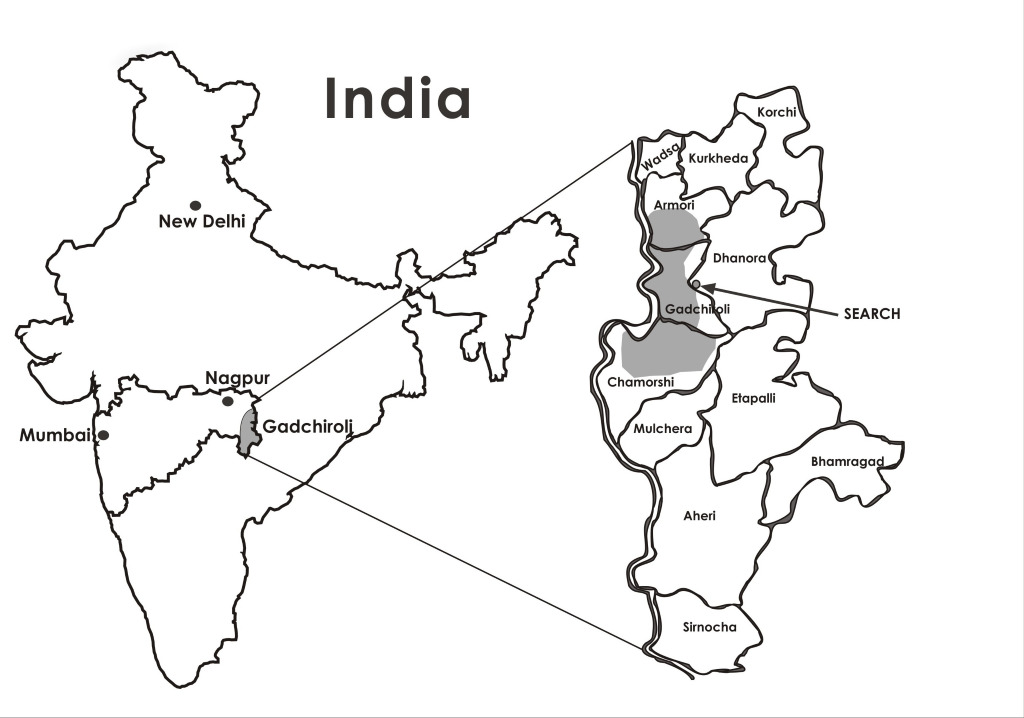
This study was conducted in Gadchiroli district of Maharashtra state of India. It has a total population of 1,107,294. A majority (93%) of the population lives in rural areas and about one third (38.3%) of the population is tribal.13 Close to 75% of the total land of the district is covered by forest. The literacy rate of the district is 66%. Subsistence farming and farm-labor are the main occupations in the district and in 2011 the per capita annual income was Rs 33,504 (about 550 US$).13 There are very few private medical practitioners in the district and the healthcare is predominantly provided through the public healthcare system which includes one district hospital, 12 community health centres, 45 primary health centres and 36 public health units.13 However, many of these facilities are understaffed. The physician to population ratio in this district is about 1:5000 as against 1:1300 for the rest of India in 2011.14
Society for Education, Action and Research in Community Health (SEARCH) is a non-governmental organization working in Gadchiroli district since 1986. It has a demographic surveillance system in 86 villages with a population register which is updated yearly and all the births and deaths are recorded.
Study design and data collection
This was a prospective study to assign causes of death in a well defined population in a demographic surveillance site using verbal autopsies. The data collection method and sample size calculations have been described in detail previously.15 Briefly, information on the circumstances that lead to death was collected using a verbal autopsy tool which has been validated in the Registrar General of India’s SRS,16 the only nationally representative system for ascertaining cause of death in India. For this study, information on causes of death was collected from 86 villages distributed in three administrative blocks (Gadchiroli, Armori and Chamorshi) of the district (Figure 1) where the mortality surveillance system is active. Data were collected prospectively between April 1st 2011 and March 31st 2013. Residential community health workers reported all deaths. Trained male field supervisor of SEARCH visited the household where a death had occurred and collected information using a verbal autopsy tool. The supervisor visited the household within two weeks of the death if the death occurred in the field practice area of SEARCH and within four weeks of death if the death occurred outside the field area. The verbal autopsy tool used for this study had an open ended narrative and a series of close ended questions. A symptom specific checklist was used to obtain additional information on a given symptom. The forms were filled in the local language Marathi. To account for any missing deaths house to house cross-surveys were conducted annually.
Assigning cause of death
Trained physicians independently read the verbal autopsies and assigned the underlying cause of death using the method developed for the Million Death Study by the Registrar General of India and the Centre for Global Health Research at the University of Toronto.17 A code was assigned to the cause of death using the World Health Organization’s (WHO) tenth revision of the International Classification of Diseases (ICD-10). If there was a disagreement between the coders, the coders were provided the code assigned to the death by the other physician and asked to reconcile the cause of death. If the two coders continued to disagree, a third senior physician adjudicated the cause of death.
Ethical approval
The study was approved by the institutional ethical committee of SEARCH. Verbal consent was obtained from the relatives of the deceased person and this consent procedure was approved by the institutional ethical committee of SEARCH. All the data were kept securely and confidentially. The procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Statistical analysis
The de jure method was used whereby only the deaths of the individuals who were resident of the 86 villages were used to calculate death rates. We calculated death rates by dividing the number of deaths between April 1st 2011 and March 31st 2013 by the population under surveillance. The data on the population size were obtained from the population register of SEARCH which is updated annually. The person-years of follow up were calculated by multiplying the mid-period (2012) population by the period of surveillance which was two years for this study. The cause-specific mortality fractions were calculated by dividing the numbers of deaths due to a particular cause by the total number of deaths. Data were analyzed using statistical software Stata version 10 (Stata Corp, College Station, TX, USA).
RESULTS
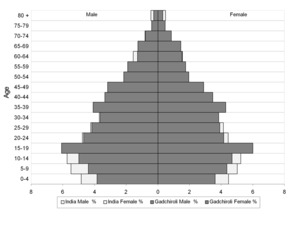
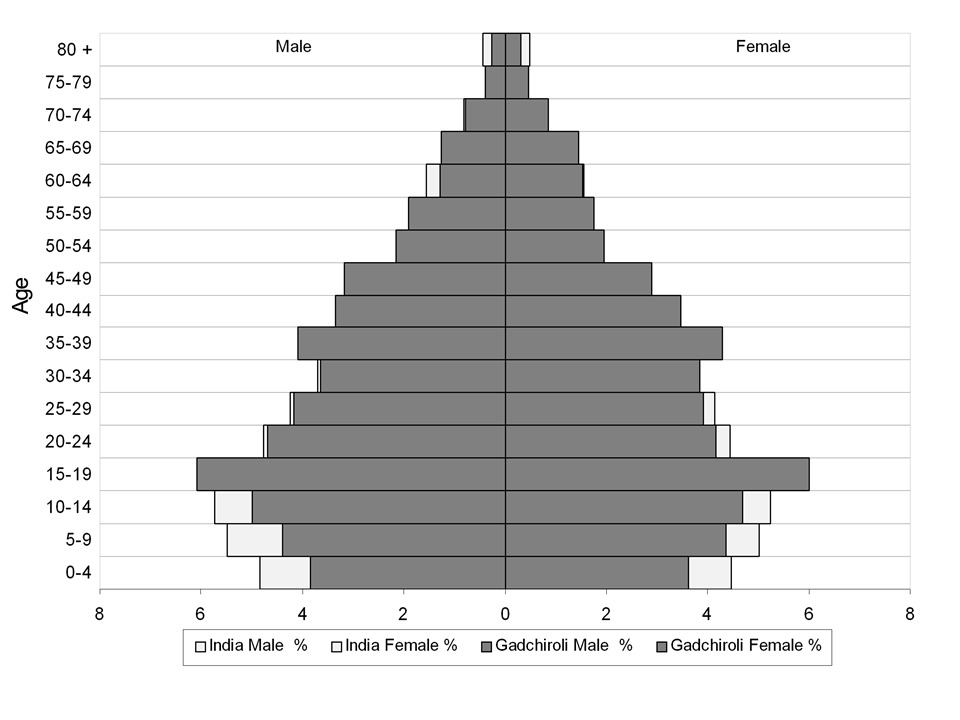
A total of 1599 deaths occurred over 188,308 person years of follow up during the study period. The population structure and its comparison with the national population structure is shown in Figure 2 and shows that the study area had lesser under-15 population compared to the Indian national population.
Out of all deaths 730 (45.7%) occurred among females and 869 (54.4%) among males. The crude death rate for the population was 8.5 (95% confidence interval (CI) 8.1-8.9) per 1000 population (7.8 and 9.2 for females and males respectively).
Two physician coders agreed in 83% and adjudication by a third physician was needed in 17%. 1485 (92.9%) deaths occurred at home, 79 (4.9%) occurred in hospitals and 35 (2.2%) occurred at other places such as during transit.
Based on the cause-specific mortality fraction, the five leading groups of diseases causing death were diseases of the circulatory system (20.8%), infections and parasitic diseases (18.4%), external injuries (10%), diseases in the perinatal period (6.5%) and diseases of the respiratory system (6.4%) (Table 1). Collectively, these five groups accounted for about two thirds (62%) of all deaths. Among diseases of the circulatory system, deaths due to stroke (14.3%) outnumbered deaths due to ischemic heart disease (4.3%). Stroke accounted for 69% of all deaths due to cardiovascular diseases. Among infectious diseases, tuberculosis was the commonest cause of death (6%) followed by diarrhoea (4.6%) and malaria (3.9%). Among external causes of death, the commonest causes were suicide (2.5%), accidents (2%) and falls (2%). Among diseases of the respiratory system, chronic lower respiratory diseases (3.6%) and pneumonia (2.8%) were the commonest causes. Neoplasms (5.8%) were the sixth leading cause of death.
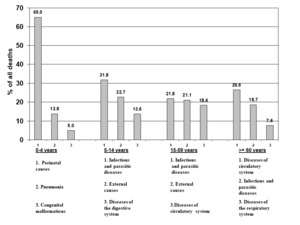
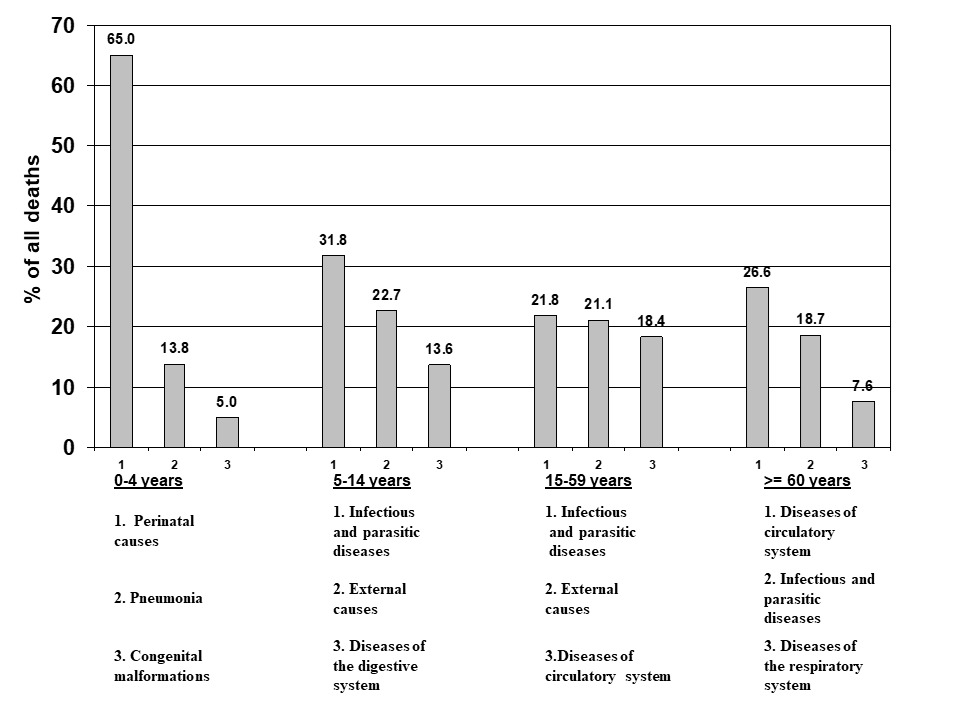
The sex-wise distribution of causes of death is shown in Table 1 and age-group-wise distribution in Table 2. External causes of mortality were more common among males compared to females (12.4% vs 7.1%, p<0.05). Maternal deaths accounted for 1.2% of all deaths among women. Out of total deaths 10% occurred in those <5 years of age while about two thirds (67.8%) occurred in those 50 years and above. The three leading causes of death in various age groups are as shown in Figure 3. These included perinatal diseases, pneumonia and congenital malformations in the age group of 0-4; infections, external causes, diseases of the digestive systems in the age group of 5-14 years; infections, external causes and diseases of circulatory system in the age group of 15-59 years and diseases of the circulatory system, infections and diseases of the respiratory system in the age group of ≥60 years.
DISCUSSION
Our study shows an evidence of epidemiological transition 18 with NCDs becoming the leading cause of death in the rural areas of one of the most underdeveloped districts of India. NCDs including cardiovascular diseases, chronic respiratory diseases, diabetes, cancers and injuries accounted for 38.5% of deaths. Infections and parasitic diseases, pneumonia, diseases in the perinatal period and diseases of pregnancy, childbirth and the puerperium collectively accounted for 28.3% of all deaths while external causes including injuries contributed to 10% of deaths. To our knowledge this is the first study from an underdeveloped rural region of India to report on causes of death.
How do our results compare against the global and national trends? In 2010, there were 52·8 million deaths globally.19 Out of these, NCDs accounted for 65.3%, communicable, maternal, neonatal, and nutritional causes accounted for 24·9%, and injuries accounted for 9.6% of deaths.19 In the SRS report, out of total deaths in India for years 2010-13, 49.2% deaths were due to NCDs, 27.7% were due to infections and perinatal conditions and 10.7% due to external causes including injuries.10 The fraction of mortality due to NCDs was lower in our study (38.5%) than the global and the national average while that due to infection and perinatal conditions (28.3%) was higher. Thus, rural Gadchiroli seems to be in a phase of epidemiological transition where NCDs have become a leading cause of death but the fraction of deaths due to infections and perinatal conditions has not declined significantly. Also, external injuries have emerged as an important cause of death, indicating a triple challenge to healthcare systems from these conditions.
In terms of leading causes of deaths, a comparison with the data from underdeveloped states from the SRS report also shows some important differences.10 Using the same disease grouping categories by the ICD-10 codes as used by the SRS, the five leading causes of death in our study were cardiovascular diseases (21.8%), ill defined causes (18.4%), diarrhoeal diseases (6.1%), tuberculosis (6.1%) and malignant and other neoplasms (5.8%). In the SRS study the five leading causes among the underdeveloped states were cardiovascular diseases (15.6%), ill defined causes (12.4%), perinatal conditions (8.5%), respiratory diseases (8.2%) and diarrhoeal diseases (7.8%).10 Cardiovascular diseases, ill-defined conditions and diarrrhoeal diseases were among five leading causes of death in both the studies. Perinatal deaths did not appear in the top five leading causes using the disease grouping used in the SRS study and this is likely to be due to the successful implementation of the home-based neonatal care programme in almost half of the villages in our study area which has significantly reduced infant mortality.20 Cancers featured in the top five leading causes of death in our area and this is likely to be due to high prevalence of tobacco use in our study area.21
Cardiovascular diseases accounted for 20.7% of all deaths in rural Gadchiroli. According to the SRS data, the percentage of deaths due to cardiovascular diseases for the years 2010-13 was 23.3% nationally and 15.6% for the underdeveloped states. The higher percentage in our study could be due to differences in risk factor distribution or possible regional differences in cardiovascular mortality.22,23 Among cardiovascular diseases stroke was the leading cause of death and accounted for 14% deaths. The deaths due to stroke significantly outnumbered deaths due to ischemic heart disease (4.34%). This is likely to be due to the early phase of epidemiological transition in this region where hypertension driven deaths predominate.24 Hypertension is the leading risk factor for stroke.25 Due to increasing life expectancy in rural areas of India leading to aging and changes in risk factors, hypertension is emerging as an important risk factor for cardiovascular diseases in rural India. For example, in a nationally representative study, the prevalence of hypertension among urban Indian adults was close to 25% while in rural India it was 20%, suggesting that the prevalence of hypertension in rural India is increasing and catching up with that in the urban areas.26 Hypertension often remains undiagnosed, untreated and uncontrolled in rural areas 26 due to the lack of healthcare facilities which increases the risk of cardiovascular diseases such as stroke.
Infections and parasitic diseases have accounted for 18% deaths. his is higher than that reported from rural areas in northern and southern India (12%) and the modelled national estimate reported by the India State-Level Diseases Burden Initiative (15.5%) but is close to the national average (17.8%) reported in the SRS data.8,11,27 This is higher than that reported from rural areas in northern and southern India where infections were responsible for 12% of deaths but is close to the national average of 17.8% reported in the SRS data and the higher than the modeled estimate reported by the India State-Level Diseases Burden Initiative (15.5%).8,27 Our findings are similar to those reported from a demographic surveillance site in Bangladesh where infections were responsible for 18-23% of all deaths.28 Among infections, tuberculosis was the leading cause of death (6.1%) in our study followed by diarrhoeal diseases (4.6%), malaria (3.9%) and pneumonia (2.8%). Despite the efforts under the National Tuberculosis Control Programme, tuberculosis has remained an important cause of death in rural areas of India accounting for 4-7% of all deaths.8,27 Three deaths (0.19%) were due to rabies. Together these data indicate a significant burden of infectious diseases in this region. The higher number of deaths due to infections could be due to multiple factors such as lower socioeconomic status, lower awareness about personal hygiene and lack of easy access to healthcare.
External causes of death and injuries were the third leading cause of death in our study and accounted for about 10% of all deaths with falls, accidents and suicides each contributing to about 2% of deaths. These data are in agreement with previous verbal autopsy-based studies from rural India which have reported that 12-14% of deaths are due to external causes of death.8,27 A study from rural Bangladesh reported less deaths (6%) due to external injuries.28 Suicides contributed to about 3-5% of deaths in two studies from rural India 8,27 while in our study suicides contributed to 2.5% of all deaths. A study from rural Bangladesh reported about 1% deaths being due to suicides.28 All the suicide deaths in our study were in the age group of 15-59 and in this age group suicides accounted for about 7% of all deaths.
In our study maternal deaths accounted for 1.2% of all female deaths and 1.6% of all deaths in the age group of 15-59 years. This number is not very far off from the percentage of maternal deaths among females reported from other studies on mortality surveillance from relatively affluent rural parts of India. For example, in a study from a rural part of northern India where causes of deaths were determined between 2009-2012 maternal deaths accounted for 2.3% of all deaths among females aged 15-49.29 In a study from southern India conducted in 2003-2004 maternal deaths accounted for 1% of all female deaths.8
In our study deaths due to infectious, perinatal and maternal conditions, which are the current health priorities of the government healthcare system in rural areas,30 were outnumbered by the deaths due to NCDs and injuries in rural Gadchiroli. Our data indicate that even in one of the most underdeveloped districts of the country NCDs have emerged as a health priority. Our findings suggest that most of the rural and underdeveloped areas of India may have undergone epidemiological transition with NCDs becoming the leading cause of death. Since government healthcare systems remain an important source of care in the underdeveloped rural areas of India, these systems have a challenging task of addressing the triple challenge of diseases due to NCDs, infections and injuries.
Our study has important global implications. It suggests a rapid pace of epidemiological transition even in the most underdeveloped settings in India which could also be the case in underdeveloped rural areas of other developing countries. Since very little data are available from such areas, our study indicates an urgent need for mortality data to monitor healthcare priorities and develop healthcare response. Such data would be important to track progress towards Universal Health Coverage promoted by the World Health Organization as well as Sustainable Development Goals adopted by the United Nations General Assembly in 2015.31
There are several strengths to our study. The study was conducted in a demographic surveillance site in one of the most underdeveloped districts of India. The information was collected prospectively by highly experienced field staff using a well-validated verbal autopsy tool. Almost complete coverage of deaths was achieved through death reporting by a village health worker and yearly cross surveys to account for any missing deaths.6 Each verbal autopsy was coded independently by two trained physicians with fairly high agreement (83%). The study also has some limitations. For example, in 23% of deaths the cause of death could not be ascertained due to insufficient information. However, in previously published studies from rural India, the cause of death have remained undetermined in about 19% of deaths.9 The slightly higher percentage of unclassified deaths in our study is likely to be due to poor access to healthcare in this region. Some studies have reassigned codes for certain nonspecific cause of death to more specific categories e.g. sudden death to cardiovascular disease and fever of unknown origin to infectious diseases.10 In our study we did not reassign the cause of death codes to disease groups or categories leading to a higher number of non-specific disease codes. Recall of events surrounding death can lead to recall bias. We tried to minimize recall bias by conducting verbal autopsies within two to four weeks after the death. An additional limitation of the study is that verbal autopsy methods do misclassify underlying cause in some deaths.4,8 However, this limitation applies to all studies using verbal autopsies. Furthermore, the results of our study may not be completely representative of all underdeveloped regions of rural India as these regions could have different access to healthcare.
CONCLUSIONS
NCDs were the leading cause of death even in a rural area of an underdeveloped district of India. However, infections continued to cause a significant number of deaths and were the second leading disease category causing deaths followed by injuries. Our study indicates an urgent need for realignment of public healthcare systems in rural underdeveloped regions of India and probably other developing countries which typically focus on maternal and child health and infections. These systems will now have to address the triple challenge of NCDs, infections and injuries.
Acknowledgements
We thank Dr Rajesh Dikshit and Dr Raju Jotkar from the Million Death Study Group for help in training the field workers in data collection. We thank Anandrao Dudhbale, Diwakar Jengthe, Charandas Sahare, Remaji Shedmake, Subhash Bodhankar for technical assistance.
Funding
SEARCH was supported by the John D. and Catherine T. MacArthur Foundation. Dr Kalkonde is a Wellcome Trust/DBT India Alliance Intermediate Fellow. Dr Sahane was supported by the Dr P.S. Bidwai Rural Chronic Non-communicable Diseases Research Fellowship.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Yogeshwar Kalkonde, M.D., M.Sc.
SEARCH, PO and District Gadchiroli
Maharashtra
India 422605
[email protected]