The 20th and 21st centuries will no doubt be remembered for the number of armed conflicts in several low- and middle-income countries (LMICs). Many of these conflicts have left behind a large legacy of physical mutilation and major limb loss (MLL).1–3 In many affected countries, it is now not uncommon to see young men and women, some of them sole bread winners and/or single parents, moving on makeshift crutches, ill-fitting or broken prosthetic limbs or wheel chairs.4 Re-integration of these victims back into mainstream societies is hampered by resource limitations, lack of appropriate service delivery models, cultural attitudes to disability, stereotyping and ethnic/tribal differences that triggered the conflict.5–7 Experiences gained from countries such as Uganda and Sri Lanka show that during and in the immediate aftermath of the conflict, there is usually a response from national and international voluntary agencies to meet the immediate needs of victims.8 The wave of emotion (and visibility) generated by modern media which drives this initial response is, however, time limited. The burden of providing for the permanent disability associated with conflict hence falls almost entirely on national governments who in many instances are neither equipped nor resourced to take on this additional role effectively.9 The resulting gaps in service provision have a potentially life-changing impact on victims, their families and the wider community.10 As these countries transition into the post-conflict period the existing pool of patients with MLL are joined by new groups of patients who lose limbs due to complications associated with diabetes, peripheral vascular disease, malignancy or civil trauma.11 Understanding this changing demography, and the cumulative effect on the existing pool of victims is essential for effective service planning in many post-conflict countries.
The Acholi sub-region of Northern Uganda is about the size of Belgium, and has a population of approximately 1.5 million residents.12 It is one of the three Sub-regions that comprise Northern Uganda which has a total population of 7.8 million.12 The region witnessed a brutal war between Lord’s Resistance Army (LRA) and the government forces which lasted for almost two decades with large scale combat coming to an end around 2006.13,14 The number of victims who lost limbs as a result of this conflict has never been determined. As most victims live in remote villages, with little contact with service providers, the available estimates (mostly limited to the Gulu district alone) are likely to underestimate the extent of the problem.15 The Gulu Regional Referral Hospital (GRRH) and Lacor St Mary’s Missionary Hospital (LSMH) are two major hospitals in the Acholi sub-region where most of the surgical services (general, trauma and orthopedic) were provided during the conflict and post-conflict period. In the immediate aftermath of the war several international non-governmental organizations in partnership with GRRH have played a crucial role in setting up and providing relatively comprehensive prosthetic limb and rehabilitation services (Gulu Referral Orthopedic Workshop: GROW).15 The services provided by these agencies were primarily aimed at victims of the conflict and hence the needs of the new cohorts of patients in the post-conflict period were not fully met. To complicate matters further, the funding of this facility to date – including the costs of consumables, has come mostly from donor agencies and few tangible attempts have been made to ensure that such a vital facility is built on a more sustainable financial model. This creates several problems to patients dependent on these services. For example, in 2015/16 and subsequently the facility at GROW remained under-functional for over 5-6 months/year due to lack of funds as donor agencies scaled down their operations (Personal communications MN). The impact of these changes will no doubt have catastrophic consequences as summarized by one of the patients who told our team “if this Unit closes we will all die”.
In this context, we have undertaken this study with the following objectives:
a. Describe the causes, pattern and immediate peri-operative outcome of ongoing MLL at the two major hospitals in the Gulu district in the post-conflict period.
b. Explore the experiences of service-users and understand some of the socio-economic and ethno-cultural factors that influence day-to-day experience of people living with MLL.
c. Describe the current state of prosthetic limb service provision in the region and the challenges to the sustainability of those services.
METHODS
A: Describe the causes, pattern and immediate peri-operative outcome of ongoing MLL at the two major hospitals in the Gulu district in the post-conflict period
A retrospective review of major limb amputations at the two major hospitals in Gulu district - GRRH and LSMH was undertaken. Major limb amputation was defined as amputation (or disarticulation) above the ankle or wrist joints.
Recovery of notes
The operation notes of all patients who underwent these procedures between June 2007 and August 2018 were retrieved from the medical records departments of both hospitals. At GRRH many patient files were missing and so available data were extracted from the operating theatre registers. The notes at LSMH were sourced by dedicated medical administration staff whereas at GRRH they were sourced by the clinical staff.
Selection and analyses
All individuals who had had major limb amputation at GRRH or LSMH were included. A data capture sheet was used at both sites to record demographic data and details of the amputation. Two practicing surgeons (OTR & MSM) at each hospital individually scrutinized the records and extracted the relevant information to the data sheet. It was agreed apriori that the minimum data set should include age, gender, indication for amputation, level of amputation, investigations undertaken, number of limbs amputated, admission and discharge dates, co-morbidities, complications, clinical outcome and address of the nearest district headquarter. Patients for whom the minimum data set was not available were excluded from the final analysis. Google maps was used to estimate the approximate distance from GROW to nearest district headquarters via road for each subject. Information extracted from the above sources was entered and analyzed with SPSS (Version 15) (IBM, London, UK). Results are presented with descriptive and inferential statistics.
B: Explore the experiences of service-users and understand some of the socio-economic and ethno-cultural factors that influence the day to day experience of people living with MLL in the Region
In most health systems, prosthetic and orthotics services are closely linked to rehabilitation services all physically disabled people may require. Hence absence of prosthetic services will also suggest relative paucity of general rehabilitation services in that country. In this component of the study therefore we included patients with MLL and other visible physical disabilities to get a detailed insight into the life experience of people living with physical disabilities in the Region. Six semi-structured focus group discussions were done to explore the lived experiences of individuals with MLL and other visible physical disabilities in this setting. Trained, local investigators who spoke the local language and had the local cultural awareness conducted the discussions. Questions were open to allow the group freedom to discuss matters important to them, and identify themes not anticipated by the research team (Appendix S1 in the Online Supplementary Document.
Selection of focus groups and qualitative data analyses
A focal person for the district health offices of Omoro, Nwoya and Gulu districts were contacted by phone. This person then located the local community development officers for each district, who were then able to mobilize village health team workers for training. The trained village health team workers went house to house to recruit people in the community known to suffer from disabilities, including MLL. The audio recordings for focus groups and key informant interviews were transcribed into English by a third party and analyzed using thematic analysis. Two researchers analyzed the data separately and then compared results to ensure validity. Overlapping themes and inconsistencies were discussed and resolved through frequent meetings. Results were reported collectively but the source of each quote has been denoted by the age and sex of the respondent. NVivo Pro 12 software (QSR International, Victoria, Australia) was utilized to facilitate management and analysis of the data.
C: Describe the current situation and challenges with regards to prosthetic limb services provision in the region
A general literature and internal government and health department document search was undertaken to assess the current state of prosthetic and rehabilitation services in the area. The information obtained was verified by direct interviews with relevant officers attached to the District health office for Gulu – the main administrative district for the Region. Further key informant interviews were also undertaken by telephone by two of the investigators (MSM&AC) on the 16th and 17th October 2018 to verify the information obtained from the above sources. Individuals were identified purposefully through known links of GROW and the Gulu District Health Office, and then by asking those interviewed who else they felt were centrally involved in prosthetic services or amputee support in the area.
Ethical considerations
To ensure confidentiality, patient details were not recorded on data capture sheets. Personal identifiers were removed from interview transcriptions of both key informant interviews and focus group discussions. Transcripts were secured in password protected documents. Full informed consent was obtained for focus group discussions and key informant interviews to be audio-recorded and for photographs to be taken. Written consent was sought from individual subjects but if patients were illiterate, witnessed oral consent was used. There was an expectation that some topics may be traumatic to discuss. Participants were provided with access to a trained counsellor who was present at all focus group discussions. Participants who expressed a desire to access rehabilitation services having previously been unable to were linked up appropriately. Institutional Ethics Board approval for the focus group sessions was obtained from the University of Gulu, Uganda and the University of Manchester, UK.
RESULTS
A: Retrospective review of inpatient notes
Two-hundred and thirty-three records of amputations were identified between June 2007 and August 2018. The complete data set was available for 141 patients - all of them had their surgery April 2014 – August 2018. A detailed analysis of this cohort (n=141) is summarized in Table 1. The mean (SD) age of this cohort was 43 (22.2) years and the age range was 1 – 93 years. The male:female ratio was 2:1. The mean (SD) duration for hospitalization was 6.4 (8.2) weeks. The mean (SD) distance travelled by patients was 91kM (75), (Range: 1-307kM).
Indication for amputation
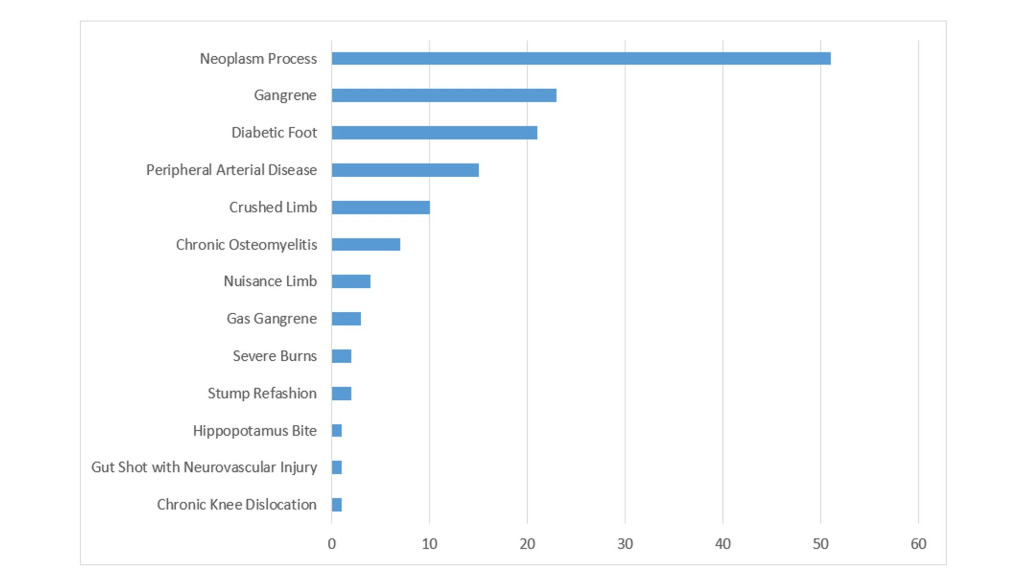
The immediate indication for amputation is summarized in Figure 1. Amongst the 51 patients who underwent amputation due to malignant neoplasms, 39% were due to squamous cell carcinoma (n=20), 26% were due to soft tissue sarcoma (n= 13), 16% were due to osteosarcoma (n=8), 14% malignant melanoma (n=7), and 6% were due to “other sarcomas” (n=3). Trauma (crush injuries, gun shot and animal bites) accounted for 8.5% (n=12) of all amputations. The co-morbidities most commonly seen in the entire cohorts were peripheral arterial disease (11%), diabetes (15%), hypertension (4.3%), HIV (3.5%), Anemia (2.1%). Others include epilepsy, renal failure and old infected gunshot wounds. Ten per cent of patients (n=14) died before discharge and other complications associated with surgery included stump sepsis (12.8%), septic shock (2.1%), Multiple Organ Dysfunction Syndrome (MODS) (1.4%), and necrotizing fasciitis (1.4%). Other longer term complications experienced were chronic anemia, deep vein thrombosis, bone infiltrations and compartment syndrome.
Level of amputation
The description of the level of amputation is summarized in Table 2. Amongst patients who underwent above knee amputations (AKA), 52.5% presented with dead limb in comparison to 39.% with below knee amputations (BKA). Hospital mortality was greater amongst patients who underwent AKA than those who underwent BKA or upper limb amputations (15.3%, 6.3% and 11.1% respectively).
Outcome of amputation
Of all patients, 87.9% (n=124) were discharged home and 9.9% died (n=14). Gas gangrene was associated with the highest mortality rate (2 deaths of 3 diagnoses). Amputations due to peripheral arterial disease had a 26.7% mortality rate (4 out of 15 patients), diabetic foot carried a 14.3% death rate (4 out of 21 patients), and 3 out of 23 patients with gangrene died. Despite an overall peri-operative mortality rate of approximately 10% (14 patients in total) we could not identify any statistically significant associations (multivariate analysis, P>0.05) between death and any of the other variables studied (age, sex, co-morbidity). Some of the other complications seen amongst our cohort included stump sepsis (12.8%), septic shock (2.1%), Multiple Organ Dysfunction Syndrome (MODS) (1.4%), and necrotizing fasciitis (1.4%). Two patients (1.4%) self-discharged or were lost for follow up. Even though 124 patients (88%) were discharged when their wounds had healed to an acceptable stage, only one of them was referred formally to rehabilitation services (<1%).
B: Qualitative results: focus groups
Focus group discussions were made up of individuals with disabilities such as amputations, congenital abnormalities, people with burn contractures and those unable to walk for other reasons. Six focus groups were conducted with a total of 63 participants and the details for each of the six groups are shown in Table 3. Two major themes emerged in relation to the experiences of people with disabilities in the area. They were:
a. Impact of disability on participants lives
b. Experiences of services and support available
A: Impact of disability on the participants’ lives
Stigmatization & bullying
Some participants described social discrimination as a major negative impact on their lives. Whereas some felt they could overcome such stigmatization, others described a life of fear of retribution. At times stigma was described as extreme to the point of abuse. The following examples are particularly relevant:
i. Female, 20 years old “I had challenges at school because pupils would take away my leg and force me to use one leg, this gave me hard times, but then if I left the artificial limb at home they would make more jokes. However, I just got used to it (applause from other FGD members)”
Impact on relationships
Being disabled was associated with an inability to provide for their family, dependence on other family members and relationship breakdown. Both men and women were equally affected. Participants also described relying on other people as a struggle. The following example gives an insight into the nature of the problem:
i. Female, 45 years old “People despise us a lot. For example, I started staying with my husband but then people started talking a lot, saying “Why do you stay with a mere disabled person? How will she help you?” My husband changed his mind and chased me away”
Physical pain
Another recurrent theme to emerge through these interactions was residual physical pain associated with stumps or other injuries. This was often linked to their inability to work and therefore an inability to provide for themselves and their families. This was true of both men and women. The following example provides an insight into this:
i. Male, 29 years old “I feel pain during rainy and dry season. I request for any help from government…we do not have any way to survive like human beings”
Economic burden
The economic burden of being disabled was twofold – inability to work and the extra costs associated with accessing disability services in distant places. The following statement provides some insight into this dimension.
i. Female, 27 years old: “I could not get money to go to Lacor hospital. I cannot do any work, I cannot work in the garden or fetch water. I was told that the walking stick has become too short for me but I do not have money to get another one”
Resilience
Though comments were mostly negative there were also some comments of resilience, hope and suggestions for how aspects of their lives might be improved.
i. Female, 45 years old: "I think it depends on the person who has love for you. I may be a disabled person and look for a fellow disabled person and we stay together happily because the children you will bear will not be disabled. Those “healthy people”, some of them do not have beautiful kids like for a disabled person.
B: Participants’ experiences of available services
Access to services
Services were reported to be too far away. Some participants complained that when they eventually reached the health centres, they were not suitably designed. Suggestions for improvements included reducing the distance service-users had to travel.
i. Male, unknown age: "This one [prosthetic leg), if it gets spoilt you have to go from Lalogi up to Gulu to have it worked on. If the orthopaedic workshop could be brought nearer to people here in the sub-counties, and things for walking could be made here, that would be good".
Affordability of services
There were both direct and indirect costs to getting treatment. Direct costs included the cost of treatment itself, transport to the services and the cost of food and board once patients arrived. The total time required to access services was considered an indirect cost as individuals and their attendant were unable to earn a living during this time. The following statement is particularly informative:
i. Male, 30 years old: “It is costly when you come from far away, and then you have to cater for your own meals, buying from the shops and hotels. That’s why some people choose not to come; because of lack of money”
Availability of services
Some participants explained that once they had obtained the money to reach the services, they found a lack of resources hindered their care:
i. Male, 30 years old “At times, when you could go, you find the materials are not available or you find the doctors are not around”
Acceptability of services
If services were then affordable and available, sometimes they were not thought to be appropriate. The following statement captures some of the sentiments expressed:
Male 24 years: "I was taken to Kumi hospital where my leg was repaired. After one week I came back but the first leg was made like it was for a white person. The colour was different from my normal body colour and, you know, when you go to school, pupils always make fun of it"
Sustainability of services
Some participants discussed the support they had previously received from non-governmental organizations. Although helpful at the time, the lack of sustainability was a problem. Some participants explained that they felt the government should offer more support. The following statement is particularly relevant:
i. Male, 54 years old: “The people who were helping left us. I still have the wounds and its painful. Here in Alero, the only thing I get when I go to the health facility is Panadol”.
Distrust in the voluntary sector
Participants had different views on how the lack of sustainability had affected them. Some felt that a lack of follow-up and feedback created a sense of distrust of researchers and overseas aid agencies. Other participants described a willingness to accept help from anywhere. The following statement highlights some of this irony:
i. Female, 30 years old: “We have a lot of problems, yet people come and say “we want disabled people”. They write down our names but we are not seeing results. Sometimes we find it useless they are reminding us of the past. It is better if they leave us to stay like this with our problems that God has organized for each one of us”.
C: Current state of rehabilitation and prosthetic limb services in Northern Uganda
Following a review of available literature in publicly available documents – published and internal documents, three key informant interviews with the health officers in charge of the services were conducted on 16th and 17th October 2018 via telephone to discuss the current situation and challenges in providing prosthetic limb services in the Acholi sub-region of Northern Uganda. Information was corroborated between informants and an internet search was undertaken to fact check.
For a population of 7.8 million in the whole of Northern Uganda, there are four orthopaedic workshops designated for providing prosthetic upper and lower limbs. These are located in Gulu, Lira, Arua and Kuluva. Of these four centers, GROW is the only fully functioning center at the time of writing this manuscript. The service at GROW provides access to prosthetic limbs, orthopaedic appliances, physiotherapy, occupational therapy, counselling and psychotherapy to amputees.16 There is an adjoining hostel where clients can stay whilst their limbs are remodeled, and a social worker service. The others have limited capacity to fabricate and provide prosthesis. GROW was handed over to the ministry of health in 2008 but still receives partial funding from AVSI International, an Italian non-governmental organization.16 Kaluva orthopaedic workshop is funded by a Christian voluntary organization and patients who attend Lira and Arua orthopedic workshops are expected to pay privately for services or are funded by a range of charities/individuals on an ad-hoc case by case basis. The following statements by service providers are revealing:
i. “The biggest challenge is materials, we usually have to import them, there is no funding and the patients cannot afford them”
ii. “We were being funded by one organization but they pulled out in 2012 after the war. The government tried to step in but provided funding for only a year and a half”
The demand for services greatly outweighs supply. The workshop in Arua provides services to refugees from South Sudan and the Democratic Republic of Congo as well as the resident population. The current waiting list has 150 clients. In 2017, 61 clients were fitted with prosthetic limbs. The workshop contains all the necessary machines but has not been provided with materials in eight years. The case is worse in Lira, the premises is small and lacks essential machinery.
DISCUSSION
This study provides an overview of major limb loss (MLL) in one of the poorest communities in the World. We have shown that the existing pool of patients who suffered MLL as a result of the war are constantly joined by a significant number of new patients who lose limbs as a result of a range of non-communicable diseases. Our qualitative data shows that these patients undergo tremendous emotional and physical disabilities through living as disabled people in the region and the services available are neither adequate nor configured appropriately to meet the needs of this ever-increasing pool of victims. The study also shows that patients’ experiences are adversely affected by several physical, socio-cultural, economic and organizational factors. The particular challenges posed by the transformation from a ‘war time’ health service provision – largely lead by the voluntary sector to the regular health providers – either governmental or private sector, is also highlighted. Our study suggests that unless this transformation is anticipated and planned for, perhaps as an integral part of the initial interventions, large numbers of very vulnerable patients can fall victim to the gaps that arise in service provision during the transition period. This is the first study of this nature to be undertaken in this region which suffered one of the most well-documented civil wars in the past 50 years – known for its brand of extreme violence, terror and brutality. This manuscript seeks to bring these issues – many of them amenable to carefully planned interventions (e.g. simple service reconfigurations and cultural interventions) to the attention of the local health authorities, Ugandan government, non-governmental organizations, funding agencies and the wider academic community.
Amputations are usually done as an end procedure when all other options have failed. In the absence of modern limb-salvage surgical techniques – usually involving interventional radiology, these decisions have to be made on the basis of clinical examination only in Uganda as well as many LMICs. The most common indication for ongoing MLL was neoplastic disease, most of which were squamous cell carcinomas. This was surprising as trauma is often described as the most frequent reason for amputation in several other LMICs.4,11,17 In our study trauma (crush injuries, gun shot and animal bites) was the 5th most common cause of limb loss during the study period. Until very recently, the road network in and around Gulu was poor and tarmacked roads that could allow high speed travel were few and far between. The mode of transport was mostly walking, vans, buses, or motor bikes (locally referred to as ‘boda-boda’) which could travel only at modest speeds due to the nature of the roads laden heavily with pot holes. It is possible that the accidents that take place in such roads, though associated with soft tissue injuries and major blood loss, do not lead to MLL as frequently as seen in other countries. If so, this situation is likely to change quickly as high-speed modern roads are being built very rapidly, associated with post-war development and new investments.18,19 Regional variations in the etiology of MLL have previously been reported in other African countries like Nigeria. These studies found that whereas diabetic complications were the main causes for amputation in some areas of the country, in others trauma was the most common cause.11,17,20 A Tanzanian study also found diabetes to be the most common cause of major limb loss.21 The emergence of non-communicable diseases (NCDs) such as peripheral vascular disease, diabetes and leg gangrene as causes for major limb loss is in keeping with the increasing importance of NCDs in the overall disease burden in Sub Saharan Africa. The mortality rate after major amputation was 9.9% in our study and compares with the findings of Unnikrishnan et al.22 The incidence of stump infection after amputation surgery in Africa has been reported to be between 13 – 77% depending on the choice of peri-operative prophylactic antibiotic use.23 We did not have data on the antibiotics used in our patients, but the infection rate in our cohort (12.8%) compares very well with data from South Africa in patients in whom amoxicillin and clavulanic acid was used in combination for prophylaxis.23 Even though patients with co-morbidities such as peripheral vascular disease and diabetes had a greater mortality (27% and 14% respectively) in keeping with previously reported observations the differences did not reach statistical significance on multivariate analysis.24 The finding that only <1% of patients were formally referred for rehabilitation services clearly illustrates the relative lack of such services available to these patients. The only prosthetic limb facility at GRRH was established to provide rehabilitation services to the existing pool of war victims and is not resourced to provide services to the new victims who continue to join this pool year on year. This will clearly have significant socio-economic consequences given the fact that they are young subjects (mean age: 43 years).
The most common neoplasm resulting in amputation was squamous cell carcinoma (n=20, 39%). This is the most common cause of skin cancer in Tanzania and other parts of Sub-Saharan Africa and is known to be commoner amongst the black populations than their white counterparts.25,26 These patients often present late, with tumors that are thought to be biologically more aggressive and often found on the lower extremities. As a result amputation rather than resection becomes the preferred treatment option.26 Simple public health measures such as health education and raising awareness amongst community health workers may facilitate early detection of skin cancers and thereby prevent limb loss as a result. The preponderance of males in our study is also well recognized by several previous studies.17,20,21
Our focus group discussions found that living with MLL in Northern Uganda is a devastating experience. Not only did individuals feel frustrated and unfulfilled personally due to poor self-image, they also expressed great distress in being unable to support themselves and their families. The descriptions provided clearly illustrate physical, psychological, ethno-cultural and economic dimensions to this problem. Physical problems such as pain and reduced mobility meant that individuals were unable to work. Not only does physical pain have a huge impact on quality of life, but feeling frustrated and unfulfilled adds to the psychological impact of the pain itself, as described before in other LMIC settings.27,28 In keeping with previous data, the majority of our patients are in the economically productive age group.17,21,29 In northern Uganda, the majority of people work in agriculture or other employment that relies on physical mobility. This employment is mostly informal; without social insurance or pension should individuals become unable to work. Disability can therefore have a devastating financial impact on the individual and their dependents – a feature that was strongly captured by the focus groups. Similar findings have also been reported in Kampala.27,30 In this context, the cultural bias and stereotyping that adversely impacts the experience and employability of disabled people need special emphasis. Participants described experiencing stigma to the point of abuse. This can also lead to reduced health seeking behaviour.31 Strategies that attempt to tackle stigma – including culturally sensitive public engagement programmes, perhaps involving arts, culture and participatory theatre, are strongly encouraged to encourage empowerment and social inclusion.
The duration of hospital stay following amputation is usually reported to be four weeks or less.32 Our data found a mean duration of six weeks. This is likely to be due to a combination of prolonged hospital stay before and after amputation. The advanced stage of the disease on presentation delays surgery.33 The reduced capacity of rehabilitation services may then delay discharge post-operatively. Our focus groups discussed how some patients are compelled to remain in hospitals until their wounds are fully healed, rather than returning home to then face issues of poor access and additional transport costs. We found on average, patients had to travel 91Km to reach rehabilitation services. Improving access to simple wound care and rehabilitation services in the local communities would reduce the burden of prolonged hospital stay. The cost of prosthetic limb services may also prohibit access. Participants of focus groups described both the direct and indirect costs which were significant. Widening access to rehabilitation/prosthetic services- perhaps through the introduction of mobile prosthetic and rehabilitation clinics that have been implemented successfully in other LMIC settings such as in post war Sri Lanka (Unpublished), may improve access, reduce costs and even reduce duration of hospital stays after amputation surgery.34
Limitations of study
We had several limitations in our study. Of the 233 cases of amputations in the two hospitals, only 141 data sets were complete. This is a problem found in many low- and middle-income settings, where a lack of human and physical resources may mean that other aspects of care take priority over record-keeping. This is particularly a problem in Northern Uganda where resource limitation is very acute and consequently record keeping is, in general, very poor. The problem is more acute at GRRH – an entirely state-run Hospital, than at SMLH which is a missionary hospital charging a modest fee from patients and hence has access to more funds. However, even when all 233 cases were analyzed, “malignant lesion” remained the most common cause (n = 80, 34.3%), followed by gangrene (n = 61, 26.2%). Trauma was the third most common in this larger cohort (n = 30, 12.8%). In both data sets “gangrene” was a common cause of amputation. Unfortunately, patients had minimal investigations before undergoing surgery and hence the values provided for co-morbidities such as diabetes, anaemia and peripheral arterial disease in our study are likely to be under estimations.
CONCLUSIONS
As Northern Uganda recovers from a devastating civil war, the development in the road network and an increasing rate of non-communicable disease is creating a new cohort of patients requiring major limb amputation. These new patients join an existing large, but undetermined, number of patients with MLL as a result of the conflict. Current service provision is grossly inadequate to meet the demands of this population that is bound to rise year on year. In a society where the family income is based primarily on physical labor and agriculture this will have a devastating impact unless urgent attention is paid to the need for rehabilitation services. The one fully functioning rehabilitation center is overwhelmed by demand and currently faces several unique challenges associated with the transitional arrangements. Public health measures to reduce the rates of amputations – particularly due to the delayed diagnosis of skin malignancies and diabetes mellitus, are urgently needed. Culturally appropriate public engagement programs are urgently required to address the extent of marginalization and stereotyping that adversely impact on the day to day experience of disabled subjects.
Acknowledgements: The study was partly funded by the University of Manchester Social responsibility budget and MRC-AHRC Grant AH R/005796/1.
Funding: Components of this study were funded by the Arts and Humanities Research Council (AHRC), UK (AH/R005796/1: November 2017-October 2019).
Competing interests: The authors completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Professor Mahesh Nirmalan MB BS, MD, FRCA, PhD, FFICM
Vice Dean for Social Responsibility and Public Engagement
Faculty of Biology, Medicine and Health
Consultant in Intensive Care Medicine
Manchester Royal Infirmary
University of Manchester & Central Manchester Foundation Trust
Manchester, UK
[email protected]