Cervical cancer (CC) is a preventable public health problem that affects women worldwide. The highest burden of the disease is found in Sub-Saharan Africa.1 In this study, we refer to SSA as a region in Africa that includes 48 countries according to the World Bank classification.2 According to the latest 2018 Globocan estimates for cervical cancer rates, Swaziland has the highest age standardised incidence rates of about 75 per 100,000 women per year while Malawi have the highest age standardised mortality of about 54 per 100,000 women per year in the world respectively.1 The high mortality and morbidity of CC in SSA can be attributed to the lack of national cancer prevention programmes and limited resource allocation to the prevention and treatment of CC precancerous lesions.3 Overall, the main risk factor for CC is persistent or chronic infection of the cervix by one or more types of oncogenic or high risk human papilloma viruses (HPV) with serotypes 16 and 18 accounting for as much as 70% of cases of CC around the world.4 HPV is the most common infection acquired during sexual intercourse, usually early in sexual history, but HPV alone cannot explain the high incidence of the disease – hence, a number of associated co-risk factors have been identified. These include HIV infection, multiparity, multiple sexual partners, early sexual exposure, low socioeconomic status, smoking, use of oral contraceptives for over five years and co-infection with other sexually transmitted agents, such as those that cause herpes simplex, chlamydia and gonorrhoea.5 HIV compromises the immune system, making women more susceptible to HPV infection.6 Indeed, the association of CC and HIV/AIDS was identified more than two decades ago.7
Given the high burden of CC in SSA and the inadequate allocation of resources, advocacy and political attention to its control in the region.3,8 There is a need for alternative strategies to reduce the burden of CC and the disparity between high income countries (HICS) and low and middle income countries (LMICs).9 Systematic reviews of the reasons for low CC screening uptake in SSA by Lim and Ojo,10 Randall and Ghebre,11 Maseko et al,12 and McFarland et al.13 found fear, low level of awareness, embarrassment and invasion of privacy, lack of spousal support, cost, distance to screening facility, long waiting time and attitude of health workers to be the reasons discouraging SSA women from attending for CC screening. They identified some evidence gaps in areas including: overcoming cultural beliefs and practices, the role of men and religious leaders, and low level of awareness and knowledge of CC screening services. They suggest strategies to address some of these gaps should include use of community-based resources and members to provide culturally sensitive innovations.
Approaches to increase uptake of cervical cancer screening
A number of innovations have been studied to increase uptake of CC screening among women with limited access, including women in SSA and other regions of the world. Systematic reviews14–18 have examined the effect of different interventions at overcoming barriers to uptake of CC screening among ethnic minorities and women with limited knowledge worldwide. Interventions examined include CC education, provider recommendations and use of local health assistants. A recent systematic review,15 showed that a theory-based CC educational intervention significantly increased CC screening rates by more than twice (OR=2.46; 95%CI: 1.88-3.21) and offering women self-sampling for HPV testing also increased CC screening rates (OR=1.71; 95%CI: 1.32-2.22) compared to controls; the review also noted a significant effect on uptake of CC screening of invitation letters, making appointments and sending reminders to women due or over-due for screening. Innovations involving the use of community members to overcome cultural feelings and to provide culturally harmonised communications have increased success of screening among women outside of SSA.19,20 To inform the development of culturally suitable community-level cervical cancer screening for women in SSA, our systematic review will concentrate on evidence of implementation and effectiveness of community-based resources such as community health workers and or community-based civil society organisations in supporting CC screening in SSA.
Community Health Workers (CHWs)
CHWs are a category of health workers that mainly work in the community outside of health facilities; they usually have a relationship with their community, such as common language, ethnicity, race, geography, or disease condition.21 The work, cadre and efficacy of CHWs differ from country to country - and within countries, from one region to another. The World Health Organization (WHO) has defined CHWs as people who work in health care and services-related fields and have training specific to and for the purpose of their job or intervention - they have no formal professional or paraprofessional certificate or tertiary degree education. The WHO recommends that CHWs should be members of the community where they work, chosen by the community and accountable to the community – whereby they are supported by the health system, but not necessarily part of it.22 The WHO recommended a task-shifting approach to purpose-trained lay or volunteer workers (eg, CHWs) from professional health workers (eg, nurses and doctors) in order to compensate for the shortage of manpower deficit and other health care services in developing countries; this approach will help in filling the gap and reduce time to scale-up of manpower.23 Task-shifting to non-physician health workers (NPHWs) was found to be an effective and reasonable innovation to increase access to cancer care in LMICs.24
CHWs played a remarkable role in controlling the recent Ebola outbreak in Guinea, Liberia and Sierra Leone and the implementation of MDGs and achieving Universal Health Coverage in WHO Africa region.22 They have supported HIV, malaria and pneumonia and tuberculosis prevention and treatment in SSA.25 Table 1 describes some of the different names and cadres of CHWs in use in SSA.
Community-based Organisations (CBOs)
Community based organisations such as non-governmental civil society organisations (CSOs) include: faith based organisations (FBOs) eg, churches; womens’ organisations; health facility committees; village or ward development committee (VDC or WDC); rotary clubs; social clubs; academic and professional institutions and organisations; students’ unions; foundations and philanthropies. The role of non-governmental civil society organisations (CSOs) and individuals in the community in supporting cancer control efforts was emphasised by Brawley et al.26; these organisations support health care providers by providing training, equipment and supplies, advocacy and education to the public. They collaborate with governments and businesses to support and catalyse national cancer control in low and medium income countries; CSOs are more acceptable in some settings than governmental organisations and are more likely to provide culturally appropriate support to overcome barriers and attitudes to screening because of their cultural understanding of groups targeted for screening.
For over a decade, The Alliance for Cervical Cancer Prevention (ACCP) has demonstrated significant success, building partnerships and learning from a number of community based organisations in SSA about identifying effective ways to increase women’s voluntary participation in screening programs. For example, 1) in Kenya, they partnered with “Maendeleo Ya Wanawake Organization”, a national grassroots women’s organization with an estimated individual membership of 2 million women and more than 25,000 women’s groups, 2) in Ghana, they partnered with a local Rotary International Club and 3) with Khayelitsha Settlement in South Africa.27–29 Engagement of faith-based groups led to a reported increase in uptake of CC screening, knowledge of CC and positive change of behaviour towards CC screening among African American and Somali American women in the US.30,31
Rationale
In all systematic reviews on strategies to increase uptake of CC screening we have found, none have focused on our particular target groups and interventions – that is, examining the implementation and effectiveness of community level structures and services such as CHWs and or CBOs on CC screening among women in SSA (living with and without HIV). The review with most similarities to ours described efforts to integrate CC screening with HIV services in order to improve uptake of screening in SSA, finding that routine provision is still not adequate.32 This review will examine literature for SSA; although CHWs and CBOs are involved in supporting health care delivery in different contexts around the world, we choose to restrict our geographical coverage to SSA to ensure that findings are of immediate applicability in our target population.
Review question
What are the evidence of implementation and effectiveness of community health workers and or community-based organisations at increasing uptake of and/or continuing participation in CC screening among women in SSA?
Study objective
To explore and assess the implementation and effectiveness of community health workers and or community-based organisations in increasing uptake and or continuing participation in cervical cancer screening among women in sub-Saharan Africa.
METHODS
The development and reporting of this protocol was guided by the Preferred Reporting Items for Systematic Review and Meta-analyses Protocols (PRISMA-P) statement,33 the Centre for Reviews and Dissemination (CRD)34 and the Cochrane Handbook for Systematic Reviews of Intervention.35
Eligibility criteria
This criteria is guided by the PICOS (Problem or Population, Interventions, Comparisons or Control, Outcome and Study design) framework.36,37
Population
Included participants: Our target group are women eligible for CC screening in SSA. They are:
-
Women of reproductive age group (18-49 years) and older women (50 years and older) either HIV negative or HIV positive.
-
Women with prior normal screening results or schedule for follow-up screening.
-
Women due or overdue for screening in various settings such as screening programs and outreaches, HIV clinics, community health centres and sexual and reproductive health services.
Excluded participants: Women who:
-
Have had a hysterectomy.
-
Were treated or are in follow-up care for cervical cancer.
-
Are pregnant
-
Are younger than 18 years.
-
Are living outside sub-Saharan Africa.
Interventions
The interventions are services offered by community health workers and or community-based organisations in SSA.
Comparison
We will consider studies with and without control groups. The control groups will be women who either receive no intervention, or routine standard screening services.
Outcome measures
Primary outcome measure: This is the reported uptake of CC screening and/or continuing participation, as a result of interventions based on community health workers and or community-based organisations in sub-Saharan Africa.
Secondary outcome measures: These are the reported: barriers to and facilitators of CC screening; increase in knowledge of CC and screening; acceptability and satisfaction with CC screening method or screening program aided or led by CHWs and or CBOs, accessibility to CC screening programmes or facilities and costs of screening interventions.
Studies design
We anticipate varying study designs including RCTs, and observational, qualitative and mixed-methods studies. Due to the challenges and high cost of conducting RCTs in SSA, we anticipate finding mainly non-RCTs, including cohort studies, case-control studies, and controlled before and after studies from SSA. We are aware that inclusion of non-RCTs might compromise the validity of recommendations and robustness of the review, but they will be subjected to rigorous quality assessment. Further, although, RCTs are the optimal study design for review of implementation and effectiveness of interventions, reliance solely on RCTs may mean missing important data in challenging settings such as SSA.
For studies including cancers/diseases other than CC, or conducted in both SSA and non-SSA countries, we will take all possible steps to extract results specific to CC and SSA - and, where possible, contact study authors for further information. Conference abstracts where we are unable to find full text will be excluded as they typically don’t provide sufficient data for analysis. No restriction of language will be imposed. The most affordable CC screening method in SSA is VIA or VILI. If, however, we identify interventions aimed at increasing uptake of other CC screening methods (including HPV DNA testing, cytology/pap smear), we will consider them for inclusion.
Search methods
The PICO (Problem or Population, Interventions, Comparison and Outcome) framework will be used in developing the search strategy and identifying relevant studies.35 Published, unpublished and grey literature in all languages will be searched and translations will be carried out when necessary. The search strategy will be developed in collaboration with a medical librarian. Medical Subject Heading (MeSH) and free text terms will be developed and combined to identify published studies on MEDLINE via OVID interface, the search strategy will then be adapted for EMBASE, Global Health, CINAHL, ASSIA, PsycINFO, Web of science, Cochrane Central Register of Controlled Trials (CENTRAL) and Google Scholar (first 500 results). Truncation commands (using root words to capture alternative word endings), proximity operators (for words within a chosen distance of each other) and Boolean logic operators (OR and AND) will be used, and to ensure maximum yield, preliminary trial with search terms will be conducted and refined.
We will search African regional databases including African Index Medicus (AIM), African journal online (AJOL) and African Organisation for research and training in cancer (AORTIC), Open Grey and ProQuest Dissertations and Theses Global databases will be searched for more published, unpublished and grey literature.
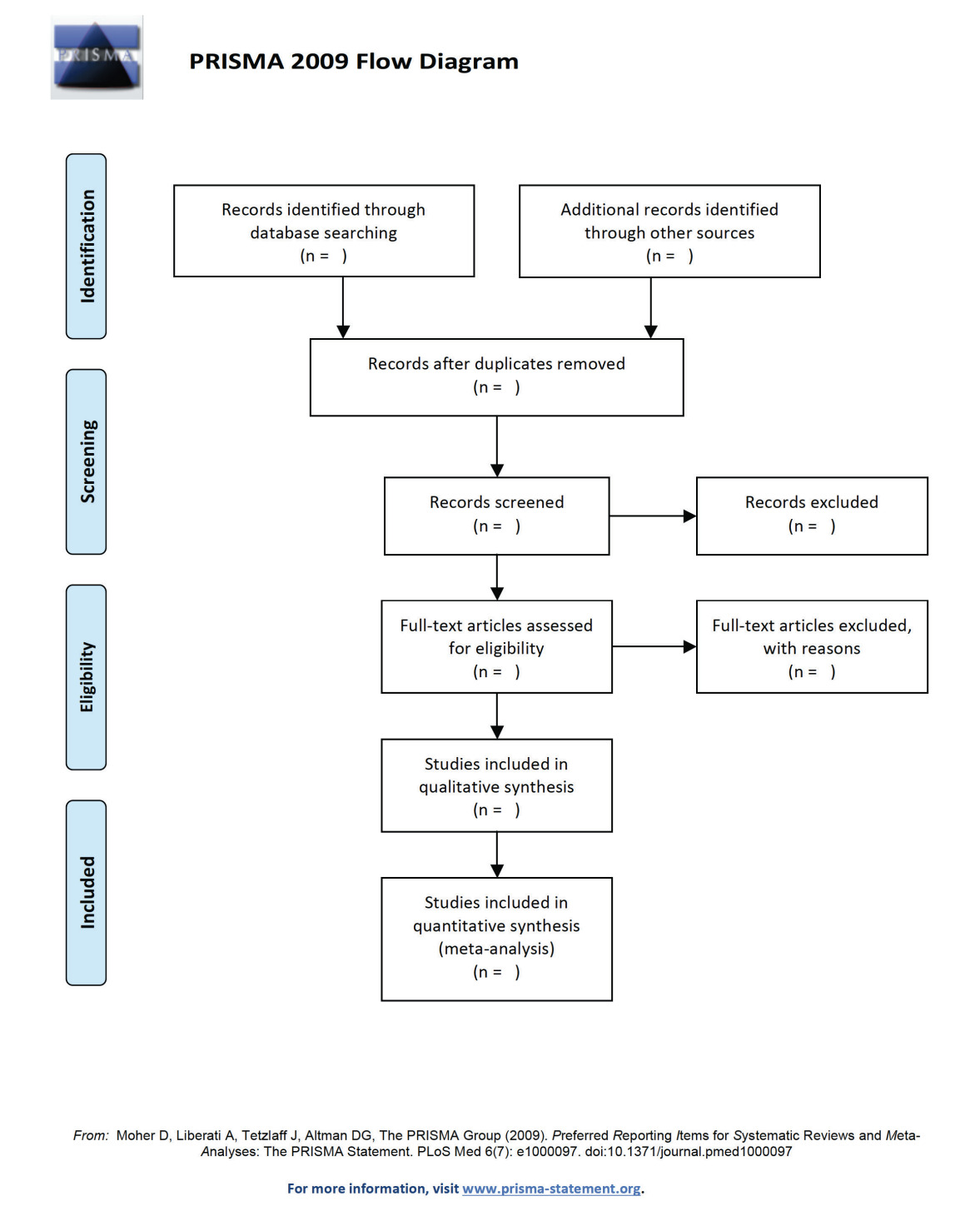
Additional papers will be located through hand-searching of citations and reference list tracking, and contacts with authors and experts in the field for further information. A PRISMA flow chart diagram (Figure 1) will be used to summarise the search and selection strategies.38 Our search strategy for identifying studies on MEDLINE database is presented in Table 2.
Data collection and analysis
Selection of studies
All titles and abstracts of studies identified by electronic database searches will be saved in EndNote library, after screening for duplicates, the remaining titles and abstracts will be reviewed independently by two reviewers. Full text copies will be downloaded and two reviewers will independently assess the studies for eligibility of inclusion into the review and disagreements will be resolved by discussion, 10% of the selected studies will be checked by 3rd reviewer for consistency. The reasons for exclusion of those studies screened in full text will be documented.
Data extraction
Two reviewers will independently extract the data from included studies using defined data extraction forms and differences between reviewers will be resolved by discussion and mutual agreement. Key characteristics of the studies (including primary outcomes) and secondary outcomes of the review will be recorded on separate tables.
The key characteristics to be extracted include:
-
Author, publication year and funding source.
-
Journal citation (including language).
-
Period of study (by year)
-
Country of study/study setting.
-
Study design.
-
Study population (characteristics and total number enrolled).
-
Intervention details (types of intervention, role of intervention, duration of intervention; duration of follow-up); primary outcomes including descriptive statistics, odds ratio (OR) or risk ratio (RR).
Quality assessment
In this review, we will adapt and use the quality assessment tools as shown in Table 3. We plan to report in narrative form and tables the results of methodological assessments of each individual study, the overall quality of the entire set of included studies cannot be merged together due to variation in tools and assessment methods. Our aim will be to exclude studies with very low scores based on distribution of quality scores especially outliers. Disagreements that arise between the reviewers will be resolved through discussion.
Data synthesis
We anticipate that meta-analysis will not be the appropriate method of data synthesis due to heterogeneous nature of the study designs – therefore, we will conduct a narrative synthesis of data from included studies according to.25,39,40
For any data we are able to synthesise through meta-analysis, we may consider a subgroup analysis based on vehicles for delivery of interventions (eg, CHWs or CBOs) or target groups (eg, HIV positive and HIV negative women). This will allow us to report the summary effects computed within subgroups, and, if possible, compare the summary effects computed in diverse subgroups. Statistical pooling of the effect of individual studies will be undertaken using RevMan 5.3, Review Manager Software.
Odds Ratios (OR) and a random-effects model will be used for meta-analysis.41 We will assess heterogeneity between studies using Higgin’s I2 statistic. Publication bias in the included studies in meta-analysis will be assessed using Funnel plots to be generated by RevMan 5.3 software.42 GRADE will be used to assess the strength of the body of evidence.
Ethics and dissemination.
Ethical issues – This study does not require ethical approval as only secondary data from published and grey sources will be assessed.
Publication plan – The systematic review protocol is registered with PROSPERO, registration number: CRD42018102539. Results of the review will be presented in conferences and submitted to peer-reviewed journal for extensive reach out to patients, researchers, healthcare professionals and policy makers on cervical cancer in sub-Saharan Africa.
CONCLUSION
This review is the first component of a project that is intended to inform a culturally acceptable community level cervical cancer screening programme in sub-Saharan Africa. The study will provide an understanding of the role of community members in supporting CC screening in their communities. It is the first review to our knowledge on the role of community health workers and community-based organisations in increasing CC screening in SSA.
Acknowledgements
We thank Marshall Dozier at the University of Edinburgh for guidance on search of database and strategy, and for agreeing to review this protocol.
Funding
This review is part of PhD study funded by Commonwealth Scholarship Commission. The Commission had no role in preparation, funding and decision to publish this protocol.
Competing interest
The authors completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest..
Correspondence to:
Danladi B. Adamu
Usher Institute
University of Edinburgh
Old Medical School
Teviot Place
Edinburgh, EH8 9AG
United Kingdom
[email protected]