Maternal, newborn and Child Health (MNCH) in the Democratic Republic of Congo (DRC) is hindered by excess mortality from preventable causes such as early marriage (18%), the low prevalence of contraception (8%), elevated rates of an unmet need for contraception (28% of adults; 31% of adolescents), and the high prevalence and complications of pregnancy among adolescents.1 The most recent mortality rates are 846 maternal deaths/100,000 live births, 28 neonatal deaths per 1000 live births and 58 infant deaths per 1000 live births.1 However, there are many other factors present in DRC that lead to excess mortality and poor MNCH including poor nutrition, lack of adequate services for antenatal and postnatal care, poor immunization coverage for women and children, and elevated rates of malaria and low treatment rates.1 In addition, the elevated sexual and gender based violence (GBV) rates in DRC have a profound effect on MNCH.1–4
The United States Agency for International Development (USAID) funded the Integrated Health Project (IHP) and the IHPplus in the Democratic Republic of Congo (DRC) to reduce mortality through improved access and quality to maternal, newborn, child health (MNCH) services, family planning and reproductive health (FP/RH), malaria, and water, sanitation and hygiene (WASH) services.5,6 Implemented at the health area level from 2012-2017 and supported by the Plan National de Développement Sanitaire 2016-2020 (National Health Development Plan), a modified champion community approach (CCA) was implemented as a community mobilization approach to strengthen the community dynamics to promote health services and improve the health of communities.7
Community mobilization is a development theory that advocates engaging community members to identify their community priorities and develop strategies to make positive behavior changes. Community engagement transforms passive beneficiaries into active partners who are responsible, independent and accountable for their own health and development.8 The use of community mobilization approaches can aid in changing attitudes, norms, practices and behaviors of individuals and groups.9 In doing so, communities are better able to assess and prioritize their needs and develop solutions that are contextualized and culturally appropriate to their communities. As such, a modified CCA was utilized to engage community members to improve MNCH outcomes, conduct outreach within their community, and become invested and involved in the development of their community instead of relying on others to force change. Our modified CCA utilized a bottom up and inclusive approach and eliminated competition between households to the top down approach first used in Madagascar in the 1990s.10,11 A unique modification to the approach included income generation and development of the champion community (CC) into a non-governmental organization (NGO).
The purpose of this study was to review the impact of the CCA on MNCH indicators in health areas where the approach was implemented. We drew on our experiences from scale-up of this model to describe this modified CCA, lessons learned and factors that made this approach a success in rural areas of DRC to inform the application of our modified CCA to other settings.
METHODS
Our CCA was implemented in 34 health zones between 2012-2017 to increase demand-driven, accessible, and high-quality healthcare and improve MNCH indicators by enabling community members to plan, carry out, and evaluate health initiatives based upon their own health priorities.
Development of a champion community
The seven steps to the development of a CC in DRC ranged from six months to one year and were dependent on the ability of community members to freely move (more difficult in conflict areas of Sud Kivu and the Kasais) and organize on a regular basis. These steps included orientation of community stakeholders, election of steering and executive committees, recruitment of CC members, work plan development, capacity building, monitoring and evaluation, and CC qualification (Figure 1).12
Community orientation
Public structures and community stakeholders were oriented on the approach to gain buy-in and support. In DRC, these included the Ministry of Health, district and zonal health offices including the chief medical officer, health area health centers, especially nurses and community health workers associated with the centers. At the community level, stakeholder introductions included the Comité de Développement Sanitaire (CODESA) which coordinates the activities of volunteers (relais communautaires or RECOs) and others such as women’s groups, youth leaders/groups like the Scouts, or community mobilizers, non-governmental organizations (NGOs), community-based organizations (CBOs), civil society organizations (CSOs) and faith-based organizations (FBOs).13
Election of the steering and executive committees
Two oversight committees were established and were important for oversight and mentoring. The Champion Community Steering Committee (CCSC) was composed of elected committee members that include a President, Vice-President, Secretary and elected counselors or local supervisors such as the nurse from the catchment health facility, chief(s), and religious and/or other traditional leaders. The CCSC served as a technical decision-making body responsible for central coordination and monitoring of activities outlined in the work plan and supervision of activities of the CC. The Champion Community Executive Committee (CCEC) also included a president, vice-president, secretary and a treasurer for bookkeeping and transparency of funds earned through income generation projects. Within DRC context, the community had to be encouraged to include women and youth.
Recruitment of champion community members
There were no limits to the number of members in the CC, but they had to represent the community (sex, age and ethnic group) and volunteer time for activities. Community structures such as the Chiefs, RECOs and CODESA members were encouraged to participate to extend their previous capacity building to the strength of the CC and to fold in all relevant community structures into the CC umbrella.
Work plan development
Using a decision tree analysis to address root causes and help define community health priorities, each CC developed a work plan with three to five priorities and activities to address their needs at health area levels that were updated yearly. Work plans consisted of improving behaviors for assisted birth, increasing ANC and PNC care visits, childhood vaccinations, breast feeding, FP/RH, human immunodeficiency virus (HIV) tuberculosis awareness and testing, and decreasing malnutrition and GBV. Nurses and/or CHWs ensured progress on the workplan and were available to lend technical assistance to activities and monitoring and evaluation.
Capacity building
As a standard package of training, champion communities received financial management, microproject design, leadership, monitoring and evaluation training and were taught to implement Education-Through-Listening (ETL) approaches.14 They were also encouraged to develop culturally-acceptable messaging such as interpersonal communication (household visits for vulnerable groups such as pregnant women or new mothers or HIV patients), interactive drama, mini-campaigns at the village or health area level or at churches, schools, community meetings, and town crier messages (megaphone messaging). Few if any pamphlets or other training materials were available in DRC, therefore the CCs found resourceful and creative ways for health messaging. In addition, CCs were encouraged to participate in all district/zonal health campaigns and develop an income-generation project to support their activities.
Monitoring and evaluation of activities
In cooperation with the nurse or CHW at the catchment health facility, indicator targets in the work plan were updated and reviewed monthly. For DRC, most of these tables were written on large paper charts and posted on the health facility walls or in CC offices. Indicator data were used for written monthly reports which were reviewed by the CCSC and health facility before being transmitted to local stakeholders and the project.
Champion community qualification
Box 1 shows the criteria for determination of reaching CC status. A ceremony in the community, funded by the community was encouraged to celebrate reaching their goal of becoming a CC. At this point, the development of CC sub-groups was encouraged such as Champion Mamas to better address breastfeeding and GBV or to create a network of women to conduct household monitoring of pregnant women and women with infants and children; Champion Youth to address youth specific issues such as education, drugs, alcohol or early marriage; and Champion Men to address negative norms and increase dialogue among household members and change men’s attitudes towards women.
Ownership and sustainability
Project staff worked with CCs to file for and receive NGO status. Grant writing and presentation training were implemented so CCs could continue to identify needs, create partnerships with other organizations and sustain their activities though income generation and grants even after the project ended. Communities, usually in neighboring health areas, who witnessed the development of CCs, autonomously developed CCs that were mentored by the project-implemented CCs. Autonomous CCs thus extended the approach to other health areas and health zones without the aid of the project.
Statistical analysis
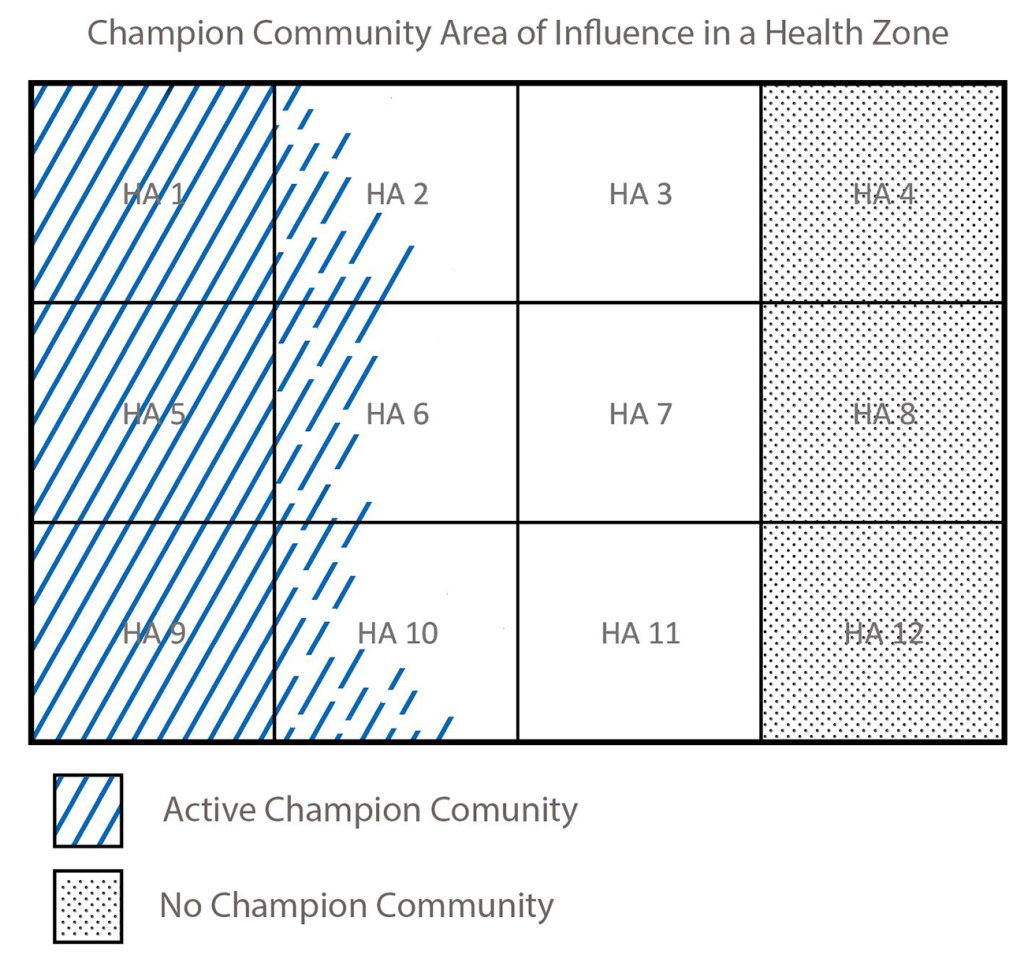
DRC has 516 health zones with 393 reference (general) hospitals and 8,504 health areas with 8,266 health centers intended to extend primary health care to approximately 5,000-10,000 persons.15 Each health zone (HZ) contains 8-16 health areas (HAs) (Figure 2).15 The approach was implemented at the health area level where each CC represented approximately 30,000-40,000 persons within three to four health areas of a health zone depending on the size and population of each health area. To limit any crossover effects from messaging in nearby health areas, the furthest 3-4 health areas were chosen for comparison (Figure 2).
Prior to 2017, only health-zone level data were available; therefore, it was not possible to compare the impact of CC activities on MNCH indicators as CCs did not cover an entire health zone. In 2017, the District Health Information System (DHIS 2) sub-grouped data by health area levels, making it possible to compare indicator changes in health areas where CCs were and were not present.
Indicators were analyzed for each of the 73 Champion Communities and grouped by each project field office. (Tables S1-S16 in the Online Supplementary Document) An average of the indicator was calculated for the 3-4 CC health areas and compared with an average for 3-4 non-CC health areas. Χ-2 (proportions) and two-sided t-test (number of visits/referrals) analyses were used to compare Champion Community health area indicators with the same indicators in distant non-Champion Community health areas. A statistically significant P-value of <0.05 was used in both the χ-2 and t-test analyses. As of 2018, not all Champion Community work plan indicators could be analyzed. For example, data were not collected or were too unreliable in the DHIS2 at health area levels for WASH; tuberculosis; GBV; latrines; potable water; and HIV indicators. Health area indicators available for analysis from DHIS2 included ANC-1 (1 visit) or ANC-4 (4 visits), acceptance of modern family planning methods, vaccinations for DPT/HepB/HIB (3 doses of pentavalent diphtheria, pertussis, tetanus, hepatitis B, and Haemophilus influenzae type b) and measles for children 0-11 months, breastfeeding (exclusive for 6 months and up to 23 months), moderate malnutrition rates among children 6-53 months, and the number of malaria visits for diagnosis and treatment.
RESULTS
Champion community summary
Thirty-five CCs were implemented in 34 health zones in Kasai Occidental, Kasai Oriental, Katanga, and Sud Kivu from 2012-2017. (Figure 3) Over the course of the project, 40 other CCs, covering additional health areas and health zones developed autonomously and were closely mentored by the project implemented CCs. Thirty-three of 35 project implemented CCs remained active in 2018. (Table 1) Two CCs established in 2012 did not continue to function as a CC; one due to poor leadership and one due to another project paying members to do their activities which undermined the approach of self-determination and sustainability. As of June 2018, there were 73 CCs in 34 health zones among eight project field offices (Tables S1-S16 in the Online Supplementary Document). For project-implemented CCs, 28/33 (85%) were legally established NGOs of which 40% (11/28), by 2018, had outside funding from other NGOs and international organizations and were considered independent (Table 1).
Champion community impact on MNCH Indicators
Full data can be found in Tables S1-S16 in the Online Supplementary Document. The following represents a summary of these data and presented as the percent of the CCs that have statistically significant rates by indicator.
Using aggregated health area data for 2017 for CCs with work plans that included ANC-1 and ANC-4, 48% of IHPplus CCs and 40% of autonomous CCs had statistically significant increases in the number of pregnant women attending ANC compared with non-CC health areas. (Figure 4) For family planning (acceptance of modern methods) rates, 55% of IHPplus CC and 25% of autonomous CC health areas had statistically higher rates than comparison health areas. Overall, breastfeeding rates (immediate and exclusive) was the indicator that showed the most statistical improvement in CC health areas. Moderate malnutrition rates among children 6-53 months were statistically lower among 44% of IHPplus CCs and 40% of autonomous CCs health areas. For IHPplus CCs working on increased assisted birth rates, 50% had statistically significant increases in these rates whereas 27% of autonomous CCs had higher rates when compared with health areas with no CCs. Where national vaccine campaigns were less effective or absent, especially in rural areas, 15% of IHP plus CCs had higher rates than non-CC health areas in contrast to 63% of the autonomous CCs that had statistically higher rates when compared with health areas with no CCs.
Finally, for the CCs that worked on curative service rates, 27% of IHPplus CC health areas and 50% of autonomous CC health areas were able to statistically improve rates of attendance for curative services. For CCs that worked on malaria, referrals for treatment and diagnosis among CCs that worked on malaria indicators trended higher but did not reach statistically significant differences from non-CC health areas except for CCs in Kamina (Tables S1-S16 in the Online Supplementary Document). For CCs that worked on malaria, referrals for treatment and diagnosis among CCs that worked on malaria indicators trended higher but did not reach statistically significant differences from non-CC health areas except for CCs in Kamina (data not shown). (Tables S1-S16 in the Online Supplementary Document).
DISCUSSION
The CCA has been employed in several countries with varying results.10,16–20 None of these approaches included income generation or the development of NGO status for independence and sustainability. All data supporting the positive impact of such an approach on health indicators is largely recorded in gray literature and lack evidence-based evaluation methods of the effect of this approach on health indicators.
Accelerator behaviors and/or the continuum of care approach for MNCH includes integrated service delivery for mothers and children from pre-pregnancy to delivery, the immediate postnatal period, and childhood to reduce maternal, neonatal and child deaths and improve health.21 However, barriers to MNCH are more than the lack of access to focused ANC.22 Understanding the accelerator behaviors in each CC implementation area was paramount to address behaviors through specific messaging to change deeply held beliefs, develop and cultivate a critical mass of supporters, expose communities to better services/solutions, create precedents and inevitably help communities realize health and enact behavior change.23–25 By empowering the community to address their specific MNCH priorities through community mobilization,8,14 CCs were able to increase ANC use, improve breastfeeding (immediate and exclusive) rates, increase family planning rates, increase assisted birth rates and decrease malnutrition rates in the health areas where they operated. These data suggest the CCA is an effective means of community mobilization which has associated improvements in MNCH indicators. Vaccinations (DPT/HepB/HIB and measles) did not have statistically significant differences between CC and non-CC health areas due to the large number of health zone campaigns that worked concurrently in CC health areas and across health zones. Most of the CC health areas and non-CC health areas had baseline vaccination rates above 80%; some as high as 99%. Although not all of the indicators in work plans improved, factors that hindered this included the presence of other influencers such as the Church of the Apostate who did not allow members to access health care, poverty, less than fully functional health centers, and other organizations working on the same indicators in the same areas.12
Lessons learned
The approach showed “Economy of Effort” and “Value for Money” as CCs, once established and independent, were contracted for their expertise by other USAID, international and local partners such as the Ministry of Health and the health zone to aid in health campaigns and household sensitization and independently developed other CCs; thus, extending the approach.
Based on our experience, CCs were best placed in remote and or insecure areas and showed more consistent statistically significant improvement in indicators. Despite remoteness, CCs are adept at describing and finding solutions to local problems.12 Although the CCA can work in any context, in more urbanized areas the same indicators may not be priority (MNCH) whereas problems such as HIV/STDs, GBV and drug and alcohol use may be higher priority health issues for communities that are not remote. In addition, CCs in urban areas had ready access to other groups that may not be basing projects on volunteerism.
Monitoring, evaluation, learning and impact
Impact analysis should be done periodically to assess whether the mobilization activities are working. Quarterly impact assessment would allow for incremental adjustment to the program and allow feedback to each CC. Electronic, community-based data collection would be helpful as opposed to relying on DHIS2 data or paper data on clinic walls.
Membership and decision making
It was vital to incorporate community leaders (religious, traditional, health) into the approach including local (health zone) authorities so they could learn the approach and support the CC on priorities and help in capacity building. Decisions must be democratic, and women must be represented and included in all levels of the process. In DRC it was important to overcome the paternalism that existed in many remote and urban areas.
Income generation
Income generation and the development of NGO status was a transformative step to independence, autonomy and sustainability of the approach. Income generation gave the CCs an ability to support their activities and other priorities and not rely on project funding. The type of income generation projects included collecting monthly dues, Village Savings and Loan Associations (VSLA), small businesses (soap and food products), agriculture projects, fish farming, livestock and small animal breeding among others.12
Legal NGO status
Over the course of the project, many of the CCs with NGO status were able to write proposals and gain outside funding from other donors including numerous NGOs, World Bank, UNICEF, health zones and Ministry of Health funds among others. With NGO status and income generation, the community decided their health priorities and advocated for their needs becoming partners in health and development instead of just a means to meet project goals.
Autonomous champion communities
Other communities realized the benefits of the modified CCA and started their own CCs and utilized project implemented as mentors. Many of the autonomous CCs developed in 2017 during a time when the CC activities for the project were not funded. This illustrated the approach was sustainable and likely to continue even after the end of the project.
Challenges
Remote communities
Remoteness of many of the CCs limited frequent oversight, visits and capacity building on a regular basis. In areas where the rainy season prevented travel, there were six-month periods where phone contact was the only means for oversight. In some of the more remote areas, CCs utilized income generation and local resources to build capacity.
Using skills to “fish”
Changing the mindset of a handout versus using skills to “fish” remained one of the biggest challenges. Some of the CCs received incentive grants for income generation projects; however, there were no differences in the success of these projects whether they were given an incentive or outside funding for their projects (US $500).12 Therefore, the incentive funding was stopped. It should be noted that none of the autonomous CCs could receive funding and they too created successful income generation projects without outside resources, illustrating that technical capacity building should be prioritized over funding or material support.
Women’s participation
Paternalism in DRC meant some CCs would form without asking for the participation of women in the community. These CCs were not as successful as CCs with a more representative group of women. This required urging CCs to represent the community and include women and youth. With the autonomous development of Champion Mamas in Ruzizi and Katana health zones, these sub-groups had statistically improved and higher rates of MNCH indicators especially for breastfeeding and nutrition, showing the importance of including women in CCs.
Use of local languages
To ensure women’s participation, the use of local language in meetings was very important. It was not uncommon for men in the group or even district and zonal authorities to insist on the use of French. It was apparent during visits to the CCs that the use of French disenfranchised women who would not raise their hand to say they did not understand what was being said.
Accounting and transparency
Champion Communities need more capacity building and training for accounting and more importantly transparency when funds are given as small grants. There was poor understanding of contracts and many CCs utilized funds that were not within the scope of the contract they signed in a trial of a small grants program. In several cases, funds given for community mobilization were utilized for buying livestock or small animals and to boost their income generation. Transparency will improve their credibility and standing to receive outside funding.
Data collection
Data collection skills were lacking at the community level. Support at higher levels was needed to address this challenge. Data not integrated into DHIS2 could have been easily collected by CCs. Furthermore, DHIS2 only began health area level data in 2017. Prior to 2017, health area level data would have been helpful to follow indicator trends for integrating health areas with and without CCs and make changes to programming if data were available.
Staff accountability and diversity
There are few social behavior change communication (SBCC) educational opportunities in DRC. Although staff have degrees from universities, and some in SBCC, these programs are not comprehensive and lack the necessary rigor to allow expertise in community mobilization in a range of contexts. Staff, in some cases suffered from paternalism at higher levels, a lack of diversity (female versus male staff) accountability and professionalism.
Exporting the approach
The adapted and innovative CCA used in DRC is exportable and is useful in other contexts and sectors. This same approach is also being implemented in USAID’s ONSE Health Activity in Malawi with similar success.
Limitations
The analysis cannot be construed to represent cause and effect. It was not possible to control for all confounders; only a randomized control trial or a longitudinal study could control for most confounders. Therefore, where both CC health areas and non-CC health areas have high rates, for example, for vaccination, it should be assumed that vaccination campaigns (health area/zonal/provincial-level campaigns) in those areas contributed to the rates and are not solely due to the CC community mobilization efforts. However, if there are statistically different rates of an indicator (such as breastfeeding) among indicators that do not have campaigns, it is reasonable to assume that the increased rates were associated with the work of the CC behavior change efforts. Finally, for community mobilization efforts to succeed, there must be an equally functional health facility or the SBCC efforts at the community level will not be effective.
CONCLUSION
Given the sustainability of the modified CCA and acceptability among other communities through the development of autonomous CCs, this approach should be integrated into the developing National Community Health Plan in DRC. The modified and adapted CCA used in DRC was an innovative community mobilization tool that fostered community mobilization and institutionalized community leadership to engage community members in improving their health outcomes. By conducting outreach within their community, CC became invested and involved in the development of their community. The modified CCA utilized in DRC that shows evidence to improve MNCH indicators now serves as a “gold standard” in community mobilization and behavior change that can be exported to other contexts.
Acknowledgements
The contents, views or opinions expressed in this publication or presentation are those of the author(s) and do not necessarily reflect official policy or position of Uniformed Services University of the Health Sciences, the Department of Defense (DoD), or Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government. This program evaluation was a secondary analysis of Ministry of Health, aggregate, de-identified data and therefore exempt from ethics review. Work on this study was completed as Senior Director of Health, Research and Evaluation at Overseas Strategic Consulting, Ltd.
Funding
This study was made possible by the generous funding of the United States Agency for International Development (USAID) under sub-agreement number OAA-A-11-00024-01-MSH under USAID Cooperative Agreement Number AID-OAA-A-11-00024.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Lynn Lieberman Lawry MD, MSPH, MSc
Associate Professor, Global Health
Uniformed Services University of the Health Sciences
4301 Jones Bridge Rd
Bethesda, Maryland 20814
USA
[email protected]


_to_illustrate_choice_of_compar.png)

_with_statistically_.png)

_to_illustrate_choice_of_compar.png)
_with_statistically_.png)