The sustainable development goals (SDG)era brings opportunities for universal health coverage(UHC) as a means for achieving equitable health coverage.1 Quality of care (QoC) should be at the centre of UHC initiatives aimed at increasing health care coverage and removing financial barriers.2,3
Service readiness is a component of structural attribute of health care quality in the Donabedian quality triad which consists of structure, process and outcome.4 Provision of inputs to care (infrastructure, medicine, guidelines, equipment) is a starting point for high-quality health care although it does not guarantee better process of care and quality effects.5–8
In 2013, WHO updated a health service readiness index to cover 50 items to allow for comparison of health service capacity across different countries and across health facilities.1 This index consisted of seven basic amenities, 6 basic equipment, 9 infection prevention measures, 8 diagnostic test and twenty essential medicines.9
In line with the commitments of 2014 Nepal Health Policy and 2015 Constitution of Nepal, Government of Nepal (GoN) is striving to achieve the goal of leaving no one behind with the provision of quality health services. Monitoring provision of care is a key management task to ensure programs are on track to achieve UHC goal.10 Ministry of Health, Government of Nepal has been conducting health facility service readiness surveys in coordination with development partners. However, the first comprehensive assessment of health facilities covering all dimensions of care was conducted in 2015.11
As the pursuit for UHC accelerates, health care quality has gained unprecedented attention within health systems. Improving quality of systems and services has been incorporated in all strategies of Nepal Health Sector Strategy (NHSS) 2015-2020.12 Furthermore, NHSS envisions an establishment of quality assurance body in Nepal to develop, introduce and employ quality standards for all types of public and private health care providers. Regular monitoring of key service provision is necessary to hold government accountable to commitments.
However, there are limited published studies exploring inequalities in health service readiness in Nepal by geographical region, and provinces; and influence of key management practices on service readiness. Previous studies exploring inequalities in health outcomes and utilization in Nepal have found that inequalities exist by urban/rural place of residence, ecological region, and distance to health facility.13–18 However, it is less clear whether these inequalities are driven by supply side factors such as service readiness. The objective of this study was to assess extent of service readiness by geography, province and key management practices in primary health care centers and hospitals of Nepal. The findings will help health policy-makers, planners and managers to make informed decision on resource allocation and planning.
METHODS
Data source
This analysis used data from the 2015 Nepal Health Facility Survey (NHFS) a nationally representative health facility survey that provide information on formal sector health facilities. The NHFS is equivalent to the service provision assessment (SPA) survey conducted in other countries which provides information on the availability of basic and essential health care services and the readiness of health facilities to provide quality health services. The data for the analysis for this study was collected using the Inventory Questionnaire collected information on staffing, staff training, infrastructure, medicines, supplies, and services offered in health facilities assessed their service readiness within acceptable standards. In Nepal, harmonization of health facility surveys for rational allocation of scare resources has been given priority for the ministry of health and development partners at the time and the 2015 NHFS was the direct result of this harmonizes agreement. 2015 NHFS is the first comprehensive national level health facility survey in Nepal that combines the components of the USAID-supported SPA of the DHS program, WHO’s Service Availability and Readiness Assessment (SARA), UNFPA’s Facility assessment for Reproductive Health Commodities and Services, and the Nepal-specific Service Tracking Survey.
Sampling of facilities
A total of 963 health facilities were included in NHFS 2015. The study sample included all non-specialized government hospitals, all private hospitals with 100 or more inpatient beds, and all Primary Health Care Centers (PHCCs). The remainder of the sample consisted of Health Posts (HP), private hospitals with at least 15 beds but fewer than 100 beds, stand-alone HIV testing and counselling (HTC) sites, and Urban Health Centre (UHC). The sample of the 2015 NHFS was a stratified random sample of health facilities selected with equal probability systematic sampling with the sample allocation. Stratification was achieved by separating the health facilities by facility type/management authority within each domain. The private hospitals were further stratified by number of beds within domain: 100+ beds and less than 100 beds, where applicable. The sample allocation features a complex allocation by taking many factors into account. Since the 2015 NHFS sample was a stratified sample, sampling weights was calculated based on sampling probabilities separately for each sampling stratum. The 2015 NHFS final report provides more detail on the methodology used in this survey.11
We chose only PHCCs and Hospitals for the current analysis because most of the WHO SARA general service readiness indicators9 are supposed to be available in higher-level facilities ie, PHCCs and above while Health Posts, UHCs and standalone HTCs are not expected to provide all the mentioned readiness items of general service readiness. So, health posts, UHC and standalone HTCs are excluded in this study. Hence a total of 134 facilities (hospitals and PHCCs) were included in the analysis. STATA 15.0 (Stata Corp, College Station TX, USA) was used and Complex sample design was accounted for in the analysis.
Study variables and indicators
The average general service readiness score represents the overall readiness status of PHCCs and hospitals to provide services. The average general readiness score is a composite indicator calculated from the range of indicators from five domains of WHO SARA indicators. Each domain carries equal weights.
The WHO SARA manual9 was used to guide the selection of indicators and general service readiness is described by the following five domains of tracer indicators and each domain consists of a set of tracer items (Table 1).
Statistical analysis
The composite readiness index was calculated from the five domains using weighted additive procedure. This procedure involves assigning equal weights to each domains, and adjusting for the “variation in the number of indicators within each domain so that the weight of the indicator is inversely proportional to the number of indicators in the domain” where a facility obtains a total score—that is, the sum of all indicators standardized to have a maximum of 100. Equal weighting is the most spontaneous approach to generate a composite measurement compared with other frequently used weighting patterns.19,20 Mean availability of item for each domain and the total number of items available in the domain was calculated in the analysis. Multivariate linear regression analysis was used to assess the relationship between covariates and the dependent variable ie, general service readiness score. P value and 95% confidence interval (CI) were considered in the analysis. Covariates used in the study are facility type (hospitals and PHCCs), ecological region (Mountain, Hill and Terai), Province (Province 1-7), external supervision in the facility in last 4 months, monthly management meeting, system for collecting opinion, routine quality assurance activities. Facility type and managing authority showed collinearity, hence the variable ‘managing authority’ was dropped from the multivariate model.
RESULTS
Distribution of sample facilities
The sample facilities: PHCCs and hospitals (n=134: weighted) were selected from 963 total health facilities that were surveyed in 2015 NHFS (Table 2). More than half of the sample facilities (52%) were private hospitals, nearly one third (32%) were PHCCs and 16% were government hospitals. Almost equal proportions of sample facilities were privately owned (52%) and publicly owned (48%). Higher proportion of health facilities (PHCCs and hospitals) were from hill region (48%) followed by Terai (45%) and mountain region (7%). About one third (31%) of study health facilities were located in province 3 while less than 10 percent were located in province 6 and 7.
Readiness status in five domains
The average readiness score for basic amenities of PHCCs and hospitals was 86.5 (Table 3). The average basic amenities readiness score was higher in Terai (88.7) and Hill (85.6) than mountain region (77.8). Among all provinces, province 6 had the lowest mean readiness score for basic amenities. Private hospitals (93.5) had a higher mean readiness score for basic amenities compared to public hospitals (91.3).
The average basic equipment readiness score of PHCCs and hospitals was 81.4. There was no much difference observed in the mean score of public and private hospitals. The average equipment readiness score was higher in Mountain (85.6) and Hill (84.5) than Terai region (79.2). Province-wise, province 2 had the lowest mean readiness score for basic equipment (72.5) while other provinces scored more than 80 mean readiness score.
The average score for standard precautions for infection prevention readiness measures in the sample facilities was 53.9. There were no remarkable differences observed in the mean score by type of HF, by management authority and ecological region. Province 2 (45) and province 7 (48) had lower mean readiness score for infection prevention than other provinces (Table 3).
The average diagnostic capacity readiness score of PHCCs and hospitals in the study sample was 71.2. Public hospitals had a higher score for diagnostic capacity than private hospitals, however PHCCs fared worse than hospitals. There were no remarkable differences in the mean score for diagnostic capacity among facilities located in Mountain, Hill and Terai. Province 4 had higher mean score for diagnostic capacity (75) than other provinces (~70).
The average score for essential medicine readiness for PHCCs and hospitals was 46.2. Table 3 shows that the mean readiness score (essential medicine) was the highest among government hospitals (52.2) followed by private hospitals (51.4) and PHCCs (34.7). Similar to diagnostic capacity, there is also a significant difference in the mean of score for hospitals and PHCCs in essential medicines. The significant difference was also observed in the mean score for public and private health facilities. Facilities in Hill region had higher mean readiness score for essential medicine than those in Mountain and Terai region. By province, province 4 had higher mean essential medicine scores (62) than other provinces. Province 1 and 2 had the lowest score (~38). Furthermore, percentage availability for each of the items within each domain was also calculated (Table S1- Table S5 in the Online Supplementary Document).
General Service Readiness Status
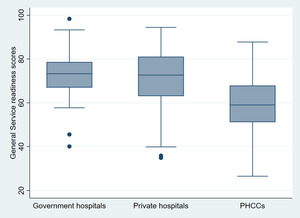
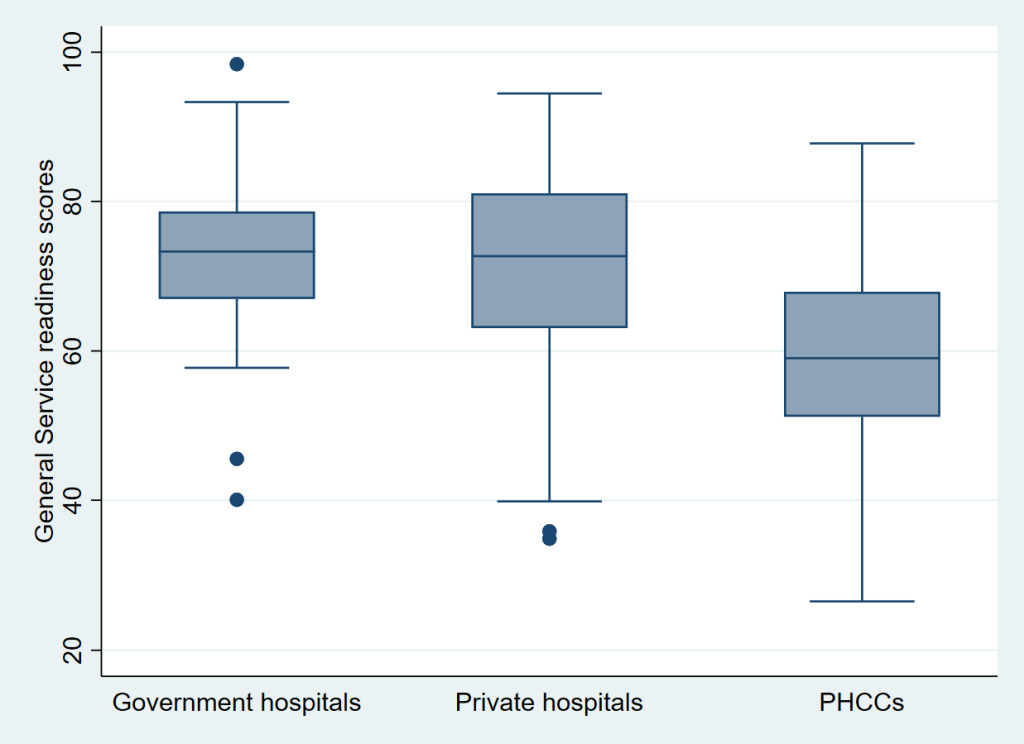
The average general service readiness score of study facilities in the study was 68.0. Table 4 shows that the mean readiness score was highest among facilities under private management (72.1) compared facilities under public management (63.6). No remarkable difference was observed in the mean readiness index of hospitals (government and private). A significant difference was observed in the mean readiness index of hospitals and PHCCs (Figure 1). Health facilities in Terai region had low mean readiness score compared to those in Mountain and Hill. Province 4 had the highest mean readiness score while province 2 had the lowest mean readiness score.
Correlates of general service readiness
The variables included in the model explained 31.1% of the variation in general service readiness (R squared=0.311). As shown in Table 5, PHCCs had significantly lower (-13.5 lower score) readiness score compared to private hospitals after adjusting for ecological region, province and key management practices (P<0.0001). Hospitals and PHCCs from Province 4 had marginally significant higher readiness score than those from Province 1 after adjusting for ecological region, HF type, and key management practices (*P=*0.009).
Hospitals and PHCCs having a system of collecting feedback from service users had a significantly higher general service readiness score compared to those which did not have such mechanism. Additionally, facilities receiving external supervision in last 4 months had a marginally significant higher score compared to facilities who did not receive supervision (P=0.05) after adjusting for ecological region, province and other management practices (quality assurance, opinion collection, monthly management meeting, routine QA meeting).
DISCUSSION
Our aim was to find gaps in service readiness and to assess differences in readiness by type and location of health facility as well as to examine effect of key management practices on service readiness. This analysis showed that average readiness score among the sample health facilities was 68.0 which was similar to average readiness score from Zambia (mean score=68) but higher than mean score from a survey of facilities from Sierra Leone (mean score=52) using a similar tool.10 The current analysis revealed that among the 5 domains of service readiness, availability of essential medicine (46.2), standard precautions for Infection Prevention (53.9) and diagnostic capacity (71.2) were worse than for availability of basic equipment (82.2) and basic amenities (86.5). Deficiencies in structural inputs identified in our study are similar to the findings from other low and middle income countries confirming that even hospitals and higher level health facilities lack basic equipment, infection prevention measures and essential medicines.1,21
By ecological region, Terai (66.0) had the lowest general service readiness, followed by Mountain (68.1) and Hill (70.0). The readiness scores by geographical reason shows poor readiness in Nepal’s hospitals and health centres compared to mission health facilities in Ghana (Southern: 76.0, middle: 91.0, and Northern: 81.0) after the introduction of National Health Insurance Scheme.22 Although health facilities in Terai (88.7) scored better than those from Mountain (77.8) and Hill (85.6) for basic amenities, health facilities in Terai scored worse for availability of basic equipment, infection prevention measures, essential medicine and diagnostic capacity compared to those in Mountain and Hill region. The findings point to a need of adequate provision of essential medicine, standard precautions for IP, and diagnostic capacity in Hospitals and PHCCs in Terai region while health facilities in Mountain region need improved availability of basic amenities, increased availability of essential medications, infection prevention materials and improved diagnostic services.
Overall average score for general service readiness was similar for private hospitals and public hospitals in Nepal. Results from facility assessments conducted in Haiti, Kenya, Malawi and Uganda also found higher median readiness score among private hospitals compared to public hospitals.1 In the current analysis, hospitals scored very low in terms of Infection prevention measures (public: 53.3, private: 55.1), and availability of essential medications (public: 52.2, private: 51.4) compared to availability basic amenities, basic equipment and diagnostic capacity. Therefore, both the public and private hospitals in Nepal need immediate improvement in these areas.
General service readiness score appeared generally better in the hospitals (public: 72.9 and private: 72.1) than in the PHCCs (58.8). Similar results were found in Zambian health facilities in terms of obstetric care with health centres having lower readiness compared to hospitals.10 In the current analysis, PHCCs had the lowest score in all 5 domains of service readiness in comparison to private and public hospitals with worst status in availability of essential medicine, standard precaution for IP and diagnostic capacity. Since PHCCs are the first referral centers in rural and underserved areas of Nepal with the provision of a medical doctor,23,24 GoN needs to heavily invest in strengthening PHCCs as referral facilities for lower level health facilities (health posts).Therefore, quality improvement initiatives must be national in scope and, in most cases, need a focus in health facilities located in rural areas and Terai region. Improvement of infrastructure, laboratory facilities, medical equipment and communication facilities, among others can contribute to retention of health workers in these rural health facilities, 24 eventually contributing to improved service readiness. Identification of the best-performing facilities as model for better practices and standardizing nationwide support for service readiness could be a starting point.1
Multivariate analysis indicated that system of collecting feedback from clients and external supervision in last 4 months were associated with higher readiness score compared to facilities not having such feedback process and supervision. Trap et al conducted a randomized controlled trial to see the impact of supervision on stock management, or rational use of drugs in Zimbabwe and found a significant improvement in stock management indicators among health facilities receiving supervision than those not receiving supervision.25 The study showed that supervision in another area of service also had a positive effect on overall performance of health workers. Therefore, investments in regular supervision to primary health care workers can give positive results on stock management of drugs and equipment. Additionally, the higher readiness score among facilities with client feedback system indicates how valuable patient experiences and their feedbacks are for service improvement.26
Health system that is responsive to changing population health need is critical to achieve UHC goal.2 Availability and adequate preparation for infrastructure, human resources, essential medication and equipment that meets current and future health need is imperative for a resilient health system. However, current analysis revealed substantial gaps to provide basic health care in PHCCs and hospitals of Nepal. Gaps were more severe for essential medicines, diagnostics, and infection prevention than multi-use items such as equipment and basic amenities. A previous multi-country study including Nepal showed that comprehensive non-communicable disease service availability was below 25 percent in Nepal.27 Primary care facilities and facilities located in rural areas had a lower score than higher level facilities and those located in urban areas. Since NCDs are burgeoning health problems in Nepal,28 a proactive approach to deal with these problem with adequate provision of structural inputs for prevention, diagnosis and management of NCDs is imperative.
These findings indicate that health systems in Nepal experience shortages in fundamental resources for essential health services. This calls for an immediate action to meet constitutional commitments of “health as a human right” of all Nepalese. On the basis of these findings, federal and local governments needs to increase health sector budget and re-examine allocation priorities within health sector.29 Availability of essential medicine and standard precaution for infection prevention need the highest priority since these are lifesaving interventions and availability can be ensured within a short time-frame. Sustainable financing for health sector with the highest priority for essential medicine and infection prevention measures, monitoring of rational use of drugs, and improving the supply chain mechanisms30 are necessary steps towards the goal of universal basic health care. Along with the delegation of authority and resources, technical support from provincial/federal governments to local governments is critical to manage year round availability of essential medicine in health facilities.
This study uses data from a nationally representative survey comprising public and private health facilities hence the findings can be generalized to hospitals and PHCCs of Nepal. Some limitations of this study are worth mentioning. We did not analyze on process quality through observations of all clinical service because NHFS was assessed for specific services (family planning, maternal health and curative services for sick children). We also did not explore health worker competency while this study is limited in the facility level infrastructure and management.
CONCLUSIONS
This study found mean general service readiness score among sample PHCCs and hospitals to be 68.0. Service readiness was lower in PHCCs compared to hospitals, HFs from Terai region compared to those in Mountain and Hilly region and in Province 2 compared to other provinces. Health facilities had a worse status on availability of essential medicine, standard precautions for Infection Prevention and diagnostic capacity than for availability of basic equipment and basic amenities. Additionally, the study detected a positive association of service readiness with the presence of external supervision and client feedback mechanism. Hence, improving availability of basic inputs for essential health care and integrating supervision and client feedback mechanisms in health facilities is crucial to develop a universally accessible and effective health care for all Nepalese.
Acknowledgements: The authors would like to acknowledge the MEASURE DHS program for providing the datasets. We thank Dr. Wenjuan Wang, ICF for inputs to the draft manuscript. NHFS survey 2015 in Nepal was reviewed and approved by the Institutional Review Board of Nepal Health Research Council, Nepal; data were publicly available and did not include individual identities and thus did not require ethics approval.
Funding: None. Article processing charge was waived to the authors by the waiver/Journal of Global Health Reports.
Competing interests: The authors declare that there are no conflict interests regarding the publication of this paper. The authors completed the Unified Competing Interest form atwww.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Kiran Acharya
New ERA
Rudramati Marga, Kalopul,
Kathmandu Province 3 Nepal
[email protected]