Non-communicable diseases (NCDs), including cardiovascular disease, chronic respiratory disease, diabetes and cancer are major causes of morbidity and mortality worldwide.1 The majority of premature NCD deaths (82%) occur in low-and middle-income countries, including countries in sub-Saharan Africa where age-standardised mortality rates from NCDs have been shown to be higher than in high-income countries and projected to increase even further.1–3 Sub-Saharan Africa is currently experiencing a dual burden of disease resulting from an increasing burden of NCDs and a persistence of certain communicable diseases including malaria, tuberculosis and HIV, with significant population health, health systems and economic implications.4,5 NCDs have a huge negative economic impact and can significantly impede social development, reduce productivity and contribute to poverty.6–8 The economic impact of NCDs is likely to be high in Africa, as these diseases appear to occur at younger ages and be associated with poorer outcomes.3,9
Addressing the increasing burden of NCDs in sub-Saharan Africa requires relevant research assessing population-specific disease burdens and trends, and understanding of unique local risk factors, as well as genetic heterogeneity in the African population. Findings from such research are necessary to stimulate political will for health promotion and improvement in the health system response to NCDs, and to inform effective preventive and management strategies.10,11
NCDs as challenges to development was recognised in the 2030 Agenda for Sustainable Development adopted by the United Nations Summit on Sustainable Development in September 2015.12 Heads of State and Government agreed to develop national responses to implement the Sustainable Development Goals, including specific measures to address NCDs. In particular, they agreed to support the research and development of vaccines and medicines for NCDs that affect developing countries.
However, there currently exists a wide gap between the burden of NCDs in sub-Saharan Africa and the research response, possibly owing to limited resources for such activities and prioritisation of infectious diseases over NCDs.2,13,14 Compared to the rest of the world, Africa produces the lowest number of biomedical publications in general (less than 1%) with relatively little published on NCDs.2,15–17 Research findings from high-income countries may not always be generalizable to Africa, considering the unique environmental and genetic determinants of disease, highlighting the importance of conducting Africa-specific NCD research.
The GlaxoSmithKline (GSK) Africa NCD Open Lab was established in 2014 to help address NCDs, a major healthcare problem in Africa, by working with multiple partners including world-class academic centres globally and African research centres to deliver high quality and impactful research into NCDs, and to strengthen African research capability.18 To kick start these research efforts, the first call for proposals was published in November 2014 with up to £4 million (US $5.6 million) available to fund projects. The purpose of this paper is to outline the processes involved in launching and facilitating the first call for proposals, the outcome of the call, including brief descriptions of the successful proposals, lessons learned and the scope for future calls for funding NCD research in Africa.
Objective
The GSK Africa NCD Open Lab aims to improve the understanding of the unique attributes of NCDs in Africa and the treatment response in African patients. It provides financial support and engages scientifically with African researchers to answer locally relevant research questions pertinent to NCDs. There is also the ambition to encourage sustainable NCD research capability that will attract and retain the next generation of scientific talent within Africa, by supporting the education and training of African scientific researchers in various disciplines.
The goal for the first call for proposals was to fund research projects that aimed to improve understanding and generate new knowledge on the unique disease mechanisms, pathophysiology and aetiology of NCDs in African populations, which would subsequently inform interventions for the prevention and treatment of NCDs. Proposals had to address at least one of the priority NCD areas, ie, cancer, cardiovascular disease, diabetes, or chronic respiratory disease.19 Chronic kidney diseases and the interplay between these NCDs and infectious diseases were also in scope.
The proposal had to be led by African scientists. The first call for proposals was open to African researchers based in academic or research institutions in the following countries covering Western, Eastern and Southern Africa: Cameroon, The Gambia, Ghana, Kenya, Côte d’Ivoire, Malawi, Nigeria and Uganda. Decisions on the design and scope of the call for proposals were made in consultation with the Scientific Advisory Board members appointed to provide input and guidance on the strategy of the Africa NCD Open Lab. The Scientific Advisory Board consists of twelve leading scientists (see acknowledgements), the majority of whom are Africans.
METHODS
The call for proposals, launched in November 2014, was advertised on http://www.gsk.com and in the included countries, with significant input from GSK country medical directors. The advertisements reached 17 countries and resulted in a total of 171 pieces of media coverage, including local newspapers and scientific journals.
Proposals were subject to a two-stage application process: preliminary and full application stages.
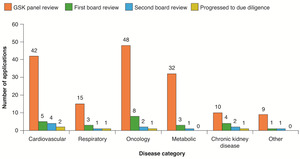
Figure 1 shows a flow diagram of the application and review processes and the outcome at each stage. At the preliminary stage, applicants submitted an outline of their proposed study electronically, indicating the knowledge gap and research questions, study objectives and the potential impact of the project, study design and proposed methods. The applications were checked for eligibility against the guidance documents that had been issued with the call for proposals, before being entered into a two-stage review process. At first review, scientific and clinical specialty experts and statisticians from GSK reviewed and scored the proposals against agreed, consistent criteria. These included the scope and scientific merit of the proposed project, its significance, feasibility and impact, the training and experience of the research team to successfully complete the proposed project, the appropriate consideration of ethical issues, the suitability of the host environment and the potential for GSK to engage in scientific collaboration for capacity strengthening. Following this initial screening, shortlisted applicants were invited to submit a full proposal providing more details on the proposed project, methods, budget and the curriculum vitae of all investigators. GSK clinical speciality experts offered support to the applicants at this stage and provided scientific and statistical input to applicants on request. The aim was to strengthen the proposals and make them more competitive for the next phase of review, or for submission to other funding agencies if unsuccessful. Applicants were given a six-week period to submit their full proposals. These were reviewed and scored by the Africa NCD Open Lab Scientific Advisory Board members. The reviewers assessed the significance and impact, the research team, the approach or methods described and the research environment of the applicants. The proposals were then ranked according to the scores obtained and discussed at a final panel meeting involving the Scientific Advisory Board and key Africa NCD Open Lab team members. Panel members were encouraged to read through all the proposals even when they were not the lead discussants. Every effort was made to ensure that any apparent or potential conflicts of interest were disclosed and eliminated throughout the review process.
Following the multi-stage review process of full applications, the five highest scoring proposals were recommended for funding and were progressed to due diligence prior to the signing of research collaboration agreements and the release of funding.
RESULTS
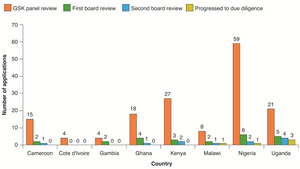
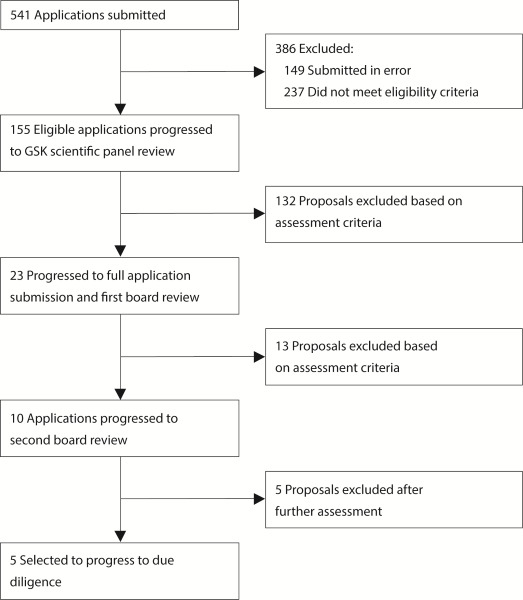
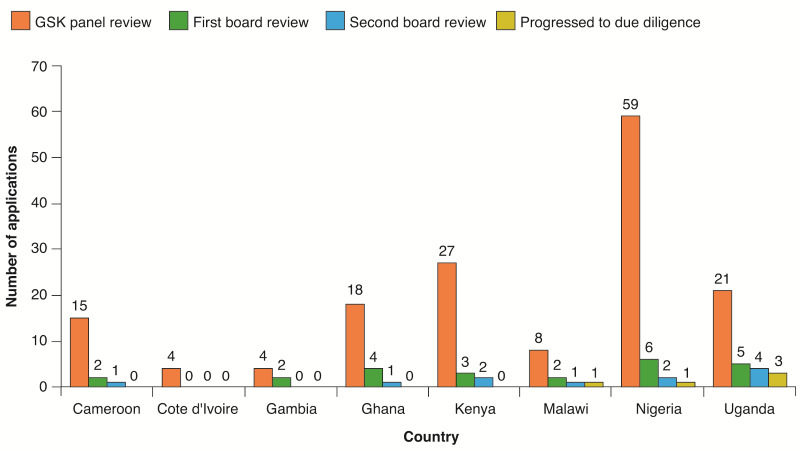
Of the 392 submitted proposals (after removing those submitted in error and duplicates), 155 met the eligibility criteria (39.5%) and were entered into the review process. The proposals covered a wide range of NCDs including oncology (31.0%), cardiovascular disease (27.1%), metabolic disorders such as diabetes (20.6%), chronic respiratory disease (9.7%) and chronic kidney disease (6.5%). The highest number of applications were submitted by scientists from Nigeria (37.8%) followed by Kenya (17.3%) and Uganda (13.5%). The progression of these applications through the various stages of review is shown by disease area and country of the principal investigator in Figure 2 and Figure 3.
The main reasons for ineligibility of proposals were applications that were out of scope (as outlined in the guidance document issued along with the call), including those focusing on health promotion, health policy, environmental science or behavioural science, proposals that did not address the priority NCD disease areas, or principal investigators from countries not included in the call. Overall, 23 proposals (6% of all submitted applications and 15% of all eligible applications) were progressed to first Scientific Advisory Board panel review and ten of these were invited to submit full applications.
Projects funded by the call for proposals
A brief description of the five projects that were funded is shown in Table 1. These projects covered different NCD areas including cardiovascular disease, the interaction between cardiovascular disease and HIV infection, oncology (breast cancer), chronic respiratory disease (asthma) and chronic kidney disease/diabetes. The principal investigators of the final selected proposals were from Nigeria, Uganda and Malawi but the projects involved collaborations with other African countries including Cameroon, Ethiopia, Kenya, Malawi, Mozambique and South Africa as well as international collaborations involving researchers from the UK, USA, and the Netherlands. All of the projects involved research capacity strengthening elements including training of MSc and PhD students in fields such as biostatistics and acquisition of clinical skills in various specialised areas. These projects if completed have the potential to improve the understanding of the aetiology and natural history of specific NCDs, while also informing the development of clinical guidelines for the effective management of disease.
DISCUSSION
The GSK Africa NCD Open Lab’s first call for proposals involving eight African countries generated a huge interest among researchers with 392 applications submitted. The high response from African scientists suggests a widespread interest in conducting NCD research in Africa, possibly reflecting the growing burden of NCDs as an important health priority. It may also reflect the limited funding opportunities for NCD research in Africa.
NCDs are an important cause of morbidity and mortality globally, occurring alongside an ongoing epidemic of infectious diseases in Africa. Current projections indicate that Africa and other low and middle income countries will have the largest increase in NCD mortality by 2020.19 In 2012 the World Health Assembly endorsed a global health goal to reduce premature mortality from NCDs by 25% by 2025.20 Research is crucial to inform diagnostic and preventive strategies and to improve the primary care response that will ensure that African countries are able to meet this goal, yet the region has the least resources for an effective response.11 Most research funding in the African region is from external sources and usually focused on infectious diseases such as HIV/AIDS, tuberculosis and malaria.21 It is, therefore, apparent that there is a pronounced gap in NCD research funding and it is important for funding initiatives, both local and international, to be sustained and to ensure the availability of resources for NCD research in the future whilst responding effectively to the changing health needs of local relevance to Africa.22,23
The level of response to the call varied among the included countries, possibly indicating differences in the level of interest in NCD research or in the research capacity and capability in these different countries. Interestingly, the country response to the call correlated well with the health research output pattern reported from the Africa region.24 The response to the call for proposals and the quality of the submitted proposals suggested that institutions with significant prior experience in obtaining research funding and those with experience of international collaborative research were over represented in the final selection process. These findings highlight a need for funding agencies to consider including training on grant application processes and proposal writing in future research funding opportunities for less experienced institutions and researchers as a means of making their proposals more competitive. The opportunity given in this call to offer scientific input by GSK scientists was highly utilised, with many researchers seeking guidance to strengthen aspects of their application, particularly in the areas of biostatistics, genetics and molecular biology. It is expected that, even if such proposals do not get funded, any improvements will make them more competitive for submission to other funders, hence increasing their chance of ultimately being funded.
The conditions for applicants in the GSK call explicitly requested investigators to include plans in their proposals for strengthening capacity in various areas of NCD research. Ensuring that all investigators highlight their plans for providing relevant training on conducting NCD research in Africa is important in promoting research sustainability efforts in the region and equipping the next generation of African NCD researchers with the skills required to conduct translational research. Building the skills for managing and delivering health research is essential for development, and for ensuring that African researchers own and drive their specific health research agendas.25 It may be useful for funding agencies to ask researchers to explicitly outline their plans for building research capacity in all submitted proposals. Greater national and international investment in capacity building in low-income countries has the greatest potential for securing dynamic knowledge systems that can deliver better health and equity, now and in the future.13
The majority of proposals that were submitted in response to the GSK call more often involved international collaborations. Although collaborations with researchers from high-income countries have been shown to be important in transferring skills to African partners, they have been reported to sometimes generate a power imbalance, where the high-income partners end up directing the research agenda without equal collaboration from the African partners.13,26 It is important to encourage South–South collaborations, as these can strengthen the ability of researchers from low-income countries to identify their own problems and needs, and to enable them to design solutions to those problems.27 Efforts to promote inter-organisational collaborations within Africa aimed at addressing a broader NCD research agenda should be encouraged.
There were variations in the disease areas of proposals submitted in response to the GSK call for proposals, with a large number of applications in oncology and fewer covering chronic respiratory diseases. The prevalence of NCDs and risk factors have been reported to vary considerably between African countries.2 The high mortality rates often associated with cancers in Africa may have led to the increased interest in oncology.28 Overall across the disease areas, the spread of research proposals submitted mirrored that of the prevalence of the major groups of NCDs.
It is evident that initiatives such as the GSK call for research proposals directed at funding NCD research in Africa and increasing local African research capability, are urgently required. To ensure the availability of locally relevant evidence-based research, such initiatives should highlight the need to include research capacity strengthening in the proposal and promote South–South research partnerships and collaborations.
Geolocation: Cameroon, The Gambia, Ghana, Kenya, Côte d’Ivoire, Malawi, Nigeria and Uganda.
Acknowledgements
The authors sincerely thank the Scientific Advisory Board for their guidance and enthusiasm during the project: Professor Clement Adebamowo, Associate Director (Population Science), University of Maryland Greenebaum Comprehensive Cancer Center, Baltimore, MD, United States of America, and Research Scientist, Center for Bioethics and Research, Ibadan, Nigeria; Dr Dwomoa Adu, Consultant Nephrologist, University of Ghana Medical School, Accra, Ghana; Professor Corey Casper, Chief Medical Officer, Infectious Disease Research Institute, Seattle, WA, United States of America; Professor Tumani Corrah, Director of the Africa Research Excellence Fund, the Medical Research Council’s Foundation Director of Africa Research Development, and Emeritus Director of the MRC Unit The Gambia, Banjul, The Gambia; Dr Julie Makani, Wellcome Trust Research Fellow and Associate Professor, Department of Haematology and Blood Transfusion, Muhimbili University of Health and Allied Sciences, Tanzania; Professor Bongani Mayosi, Professor and Head of Department of Medicine, Faculty of Health Science, University of Cape Town, South Africa; Professor Jean Claude Mbanya, Professor of Medicine and Endocrinology, Faculty of Medicine and Biomedical Sciences, University of Yaoundé 1, Cameroon; Professor Nicola Mulder, Head of Computational Biology Group, University of Cape Town, South Africa; Professor Nelson Sewankambo, Principal and Dean Emeritus, School of Medicine, Makerere University College of Health Sciences, Uganda; Professor Moffat Nyirenda, Professor of Medicine (Global Non-Communicable Diseases), London School of Hygiene and Tropical Medicine, London, United Kingdom, and NCD Theme Leader, MRC/UVRI Uganda Research Unit, Entebbe, Uganda; Professor Gerald Yonga, Professor of Medicine and Head of Non-Communicable Diseases Research to Policy Unit at Aga Khan University, Kenya, East Africa; and Prof Heather Zar, Head of the Department of Paediatrics and Child Health, Red Cross Children’s Hospital and Director of the MRC Unit on Child & Adolescent Health, University of Cape Town, South Africa. Naomi Richardson of Magenta Communications Ltd provided copyediting and graphic design assistance and was funded by GlaxoSmithKline.
Funding information
This study was funded by GlaxoSmithKline.
Competing interests
All authors are employees of GlaxoSmithKline Ltd. All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author) and declare no other conflicts of interest.
Correspondence to:
Dr Juliet Addo
Africa NCD Open Lab
R&D Alternative Discovery & Development
GSK
980 Great West Road
Brentford, Middlesex TW8 9GS
United Kingdom
[email protected]