An estimated 11 million Syrians have been displaced since the start of the civil war in 2011.1 Of these, 10 000 immigrated to the United States in 2016 alone.2 Prior to the start of this conflict, Syria was considered a low-middle income country served by a government-run healthcare system that provided most primary care services, supplemented by a private sector, which provided advanced care and specialty services.3 In 2010, Syria had an estimated 15 000 physicians for a population of 22 million, averaging 1.5 physicians for every 1000 persons.4 However, since the start of the conflict, Syria’s health infrastructure has been under siege.5 The previously functioning healthcare system has been replaced by an inadequate system under constant attack by government forces.6
A failing healthcare system results in increased morbidity and decreased quality of life associated with poorly controlled chronic diseases, including vision impairment.6 Vision impairment represents a significant public health concern, particularly among the aging population.7 Vision loss directly affects social participation, limiting employment and self-care.8 As such, vision impairment is associated with a high disease burden.9
Estimates suggest that the potential cost savings in addressing vision related concerns are greater than US$102 billion.9 The quality-adjusted life-year losses associated with vision impairment are comparable to or higher than those associated with other major chronic conditions such as diabetes, stroke, myocardial infarction/ischemic heart disease, asthma, and obesity.7 Blindness has largely become a disease of poverty, with greater than 80% of individuals with vision loss coming from low-income countries.7 In one camp in Lebanon, 24% of elderly Syrian refugees reported significant vision loss.10 In a nationwide survey in the United States, participants ranked concerns over loss of eyesight as equal to, or worse than, concerns over loss of memory, speech, hearing, or a limb.11
The World Health Organization’s Global Eye Plan 2014-2019 aims to reduce avoidable vision impairment as a global public health concern.9 As part of the objectives, the magnitude and causes of vision impairment must be identified in order to identify priorities, monitor progress, and advocate for greater commitment to eye health.9 Surveillance of visual health is essential in order to document rates of vision impairment, eye disease, vision-related functioning, and access to vision and eye care.12 Through a complete evaluation of vision impairment and the associated morbidity in specific populations member states can allocate the resources necessary to facilitate improved health and quality of life.
The burden of chronic disease and unmet medical needs among displaced Syrian refugees requires evaluation and action.13 Overall, few studies have focused on needs assessments or epidemiological evaluations among this population. Moreover, no study to date has focused on the specific burden of eye health and eye care access.10
Several health surveillance systems exist in the United States that include assessment of vision health in the general population.12 While these systems are imperfect, drawing upon them to guide assessment of the visual healthcare access and quality of life of resettled Syrian refugees can enhance the validity of the evaluation and provide data comparable to existing population surveys.12
The increasing influx of Syrian refugees worldwide represents a frontier for medical intervention. Efforts to address healthcare needs must include the appropriate assessment and treatment of eye health. Improving eye care resources for this underserved group requires the identification of the specific visual health concerns, needs, and barriers to care. As such, this study sought to provide a critical assessment of the prevalence of self-reported vision impairment, the barriers to eye care access, and the risk factors associated with vision impairment in a group of recently resettled Syrian refugees. Through these aims, this study provides the framework necessary to develop better vision related public heath interventions in immigrant and refugee populations both in the United States and in host countries that continue to welcome Syrian refugees.
METHODS
Participant recruitment
Participants were a convenience sample of Syrian refugees undergoing resettlement assistance through the Nationalities Service Center (NSC), the largest resettlement agency in Philadelphia. Participants were solicited for enrollment in person during scheduled NSC visits. Interested participants were invited to speak with a study representative and to review the study information. Non-Syrian refugees were excluded from this study. Participants that met all inclusion criteria were invited to participate. All study material was translated into Arabic and on-site translators were used as necessary.
Survey procedures
Participants completed a one-time 53-item survey, comprised of previously validated questionnaires. Part one of the survey contained components from the Arabic Behavioral Risk Factor Surveillance System (BRFSS),14 a US national survey that collects state data about health-related risk behaviors, chronic health conditions, and use of preventive services. The BRFSS was previously translated into Arabic by researchers in the state of Michigan in conjunction with the Arab Community Center for Economic and Social Services and the Department of Health and Human Services.15 We received permission to use select questions as part of our questionnaire.
Part one included 15 additional questions related to the etiology of vision impairment, visual health history, and vision-related health care access. These questions were translated into Arabic and tested for accuracy of translation. Part two of the survey included the Arabic translation of the Visual Function Questionnaire-25 (VFQ), a previously validated tool used to evaluate vision-related quality of life.16 We utilized all 12 VFQ sub-scale scores and the overall composite vision-related quality of life score. The sub-scales included general vision, general health, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, color vision, peripheral vision, and the overall composite. Each sub-scale category was calculated using the VFQ algorithm.16 The composite score was calculated as a combination of the weighted total from each sub-category.16 The scores were scaled from 0 to 100, with 100 representing the highest quality of life.
Analysis
The primary outcomes were self-reported visual impairment, VFQ composite and sub-scale scores, and eye care access. The self-reported prevalence of visual impairment and ocular health issues were identified using descriptive statistics. Sample characteristics, including socio-demographic characteristics and variables associated with refugee status, for both the adult and child groups (eg, age, gender, time since resettlement, and education level) were assessed. VFQ composite and sub-scale scores were determined using the VFQ algorithm.15 Descriptive statistics were used to summarize eye care access.
We also assessed the associations between sub-groups within the Syrian refugee community and both quality of life and increased barriers to access to care. We explored demographic variables and the relationship with quality of life and barriers to access to care. Correlates of quality of life and barriers to care included: age, level of education, gender, and length of stay in the United States. Pearson correlation, ANOVA, and chi-square were used to explore these correlates of vision-related quality of life and eye care access.
RESULTS
Sample
A total of 17 adults (mean age=42.3, range=19-77) and 6 children (mean age=10, range=5-16) completed the survey and were included in the analysis. One adult participant was unable to complete the survey due to difficulty seeing and was excluded from the analyses. About half of the adult participants were male (47.1%) and the average time since resettlement in the United States was 20.5 months (SD=12.9 months). See Table 1 for the complete description of the sample.
Self-reported visual impairment
In the adult sample, 41.2% (n=7) used glasses or contacts, and 35.2% (n=6) of the participants reported ocular pathology. The most common pathology was traumatic accident (23.5%; n=4), followed by macular degeneration and retinal detachment, both at 5.9% (n=1).
Eye care access
In the adult sample, 47.1% (n=8) of the participants had an eye exam within the past year. 29.4% (n=5) of participants reported never having their eyes checked by a primary care provider, while 23.5% (n=4) reported eye exams at each primary care visit. Of those that had not had an eye exam in over a year, the most common reason was cost/insurance (17.6%; n=3) and lack of knowledge of eye doctors and resources (17.6%; n=3). Only 23.5% (n=4) rated their eye care as excellent while 35.3% (n=6) rated the care as poor.
Visual-Function Questionnaire
The VFQ composite score had a mean of 69.4 and standard deviation of 22.1. Table 2 contains a breakdown of sub-scale scores.
Demographic and resettlement characteristics related to the VFQ
There were no significant differences in composite or sub-scale VFQ scores between genders, individuals with or without visual impairment, or education level (*P>*0.05). There was a significant difference between individuals aged 40 and older and those younger than 40 regarding ocular pain (F(1,15)=5.21, *P=*0.037), near activities (F(1,15)=8.74, *P=*0.01), distance activities (F(1,15)=4.82, *P=*0.044), social function (F(1,15)=4.95, *P=*0.042), mental health (F(1,15)=6.79, *P=*0.020), role difficulties (F(1,15)=5.14, *P=*0.039), dependency (F(1,15)=5.43, *P=*0.034), and peripheral vision (F(1,15)=3.97, *P=*0.003), compared to individuals under age 40. There was also a significant difference in composite score between individuals over 40 years of age (mean=57.7), and those under age 40 (mean= 82.5) (F(1,15)=7.47, *P=*0.015).
A significant difference was observed between individuals in the United States for 8 weeks or less and those in the U.S. for greater than 8 weeks with regards to general health F(1,15)=6.38, *P=*0.023) and general vision (F(1,15)=5.11, *P=*0.039). General health improved from a mean score of 28 to 59.5. General vision decreased from 52.4 to 29.3.
Time in United States and eye care access
We designated two groups based on participants’ last eye exam: less than 2 years or greater than 2 years, including never having had an eye exam. Participants with an eye exam within 2 years had an average time in the United States of 24.45 weeks (SD=11.23) while those with a last eye exam greater than 2 years ago had an average time in the United States of 12 weeks (SD=14.61). However, there was no significant difference in time in the United States between the two groups (F(1,14)=3.52, *P=*0.082).
Children
The average amount of time spent in the United States was 9 months. All 6 participants reported never having had their eyes checked by a pediatrician or another clinician. The most common reason for not visiting an eye doctor was that they did not have an eye doctor (66.7%, n=4).
DISCUSSION
Syrian refugees are at increased risk for poor vision and poor vision-related quality of life due to the severally diminished health infrastructure and ongoing social unrest in Syria. Individuals with a previously functioning health system have rapidly lost access to even basic health needs. During displacement, refugees shift between various countries and camps before reaching a final resettlement location. As a result, all health needs, including visual health, are compromised. This lack of stability results in a decrease in visual health and a subsequent significant decrease in vision-related quality of life. Given these realities, this study sought to document the self-reported rate and nature of vision impairment and vision-related quality of life among Syrian refugees resettled in the US.
A high number of participants in both child and adult survey groups reported never having had an eye exam. The American Academy of Ophthalmology recommends that children receive their first eye exam at six months, with a repeat exam first at age three, and again at the start of primary school.17 Given the young mean age of the child participants, most had spent the majority of their lives displaced or living in a war-torn country, without access to eye care. These barriers to access were likely present both prior to and during the civil war, creating disparities within the country such that some individuals had better access to eye care than others.
According to the National Eye Institute, 66% of Americans report using glasses or contacts. In this sample, only 41% of the adult participants reported using glasses. This may represent an unidentified need in this refugee group. Furthermore, the high rate of ocular trauma, which may be attributed to the ongoing war and political unrest in Syria, highlights the unique needs of this population. Our small sample size limits population level conclusions; however, both adult and child refugees would benefit from vision testing to address their corrective needs.
Cost and lack of knowledge of resources were the primary barriers to eye exams. This confirms the need for improved education surrounding health needs and available resources to improve visual health in similar groups. Eye care initiatives that target refugee groups must increase accessibility to quality, culturally sensitive eye care that addresses the unique needs of these populations.
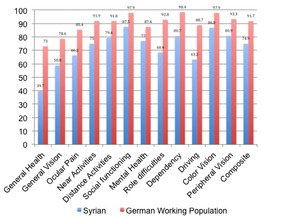
The overall mean VFQ composite score was low, especially related to the relatively young age of this sample. The lowest sub-scale score was for general vision, indicating a low overall quality of life associated with vision in this group. The VFQ is often used in ophthalmological practice to better understand ongoing ocular pathologies. However, in order to better understand the VFQ scores in the Syrian refugee population, we compared the present data to those from past studies of general adult populations. Syrian refugees had a lower vision-related quality of life than a random population of working-age German adults (Figure 1).18 In fact, the average composite VFQ for the present sample was closer to that reported by those with macular degeneration than the random population (Figure 2).19
We observed several sub-group differences in vision-related quality of life. Previous research has found age to be an independent risk factor for decreasing vision and visual health.18 Hirneiss and colleagues reported a 1.0 point decrease in composite score for every decade of life.18 In our sample, there was a decrease in vision-related quality of life between individuals greater than age 40 and those aged 40 or younger.18 This decrease in vision-related quality of life would likely be expected in any population and is not unique to refugees.
There was a significant difference in general health and general vision between individuals that had been in the United States for more or less than eight weeks. The greater than 30-point increase in reported general health may be attributed to the initial increase in healthcare utilization during the eight month insurance coverage that refugee receive. Quality of life related to general vision decreased from 52.4 in the newly resettled participants to 29.3 in those having been in the United States for over eight weeks. This paradoxical finding is in line with the refugee literature which shows that chronic disease actual worsens with increased time in the United States.20 Furthermore, this decrease in general vision may be due to an increase in actual use of vision. Recently resettled individuals have limited resources and spend a large portion of their time on health and educational training. However, after the first few weeks, they begin English classes and are able to furnish their homes. This may increase their visual demands, bringing attention to ongoing visual problems. Finally, it is possible that visual health problems developed after resettlement. Regardless of the cause, this finding highlights the need for eye care services in refugees with varying times since resettlement.
Limitations
This study was the first of its kind to use these survey instruments to understand vision and vision-related quality of life in a population of Syrian refugees. However, there were important limitations to consider. First, this was a small convenience sample of recently resettled refugees in Philadelphia. While the information can be used to inform further studies, there is limited external validity. Second, the age of the population was young for vision loss. The results may vary with an older population. Finally, our study had to end early due to a changing political climate, limiting our sample size.
CONCLUSIONS
Visual health and vision-related quality of life are important factors for overall wellness. This sample had distinctive eye care needs and lower vision-related quality of life indicators than those reported in other groups, highlighting the need for improved resources surrounding visual health and eye care access for resettled Syrian refugees. The work of this study should be used to inform research and develop interventions among similar groups to improve visual health and vision-related quality of life in refugees.
Acknowledgements
Thanks to Nationalities Service Center, University of Pennsylvania School of Public Health and Nasr Saradar.
Funding
None.
Competing interests
The author has completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declares no conflict of interest.
Correspondence to:
Sila Bal
University of Pennsylvania
Perelman School of Medicine
3400 Civic Center Boulevard
Philadelphia, PA 19104
United States of America
[email protected]