Global, national and regional burden of diarrhoea
Diarrhoea is one of the leading causes of under-five morbidity and mortality across the globe. In the past 20 years or so, there has been tremendous improvement in child survival across different regions of the world. However, the reduction in diarrhoea related morbidity and mortality is uneven and most of the disease burden is in lower and middle income countries.1 Global burden of diseases reported that in the year 2004, more than 80% of child deaths due to diarrhoea occurred in Africa and South Asia. The same study also reported that around 75% of all diarrhoea related deaths globally happen in just 15 countries and India tops this list with 386 600 deaths annually caused by diarrhoea.2 The most recent national level data on burden of diarrhoea in India is available from National Family Health Survey – 4 (NFHS4) (2015-16) that reports the prevalence of diarrhoea as percentage (2 weeks prior to survey) in India is 9.2 which has increased from the level of 9.0 percent reported by the same survey conducted in the year 2005-06. Furthermore, NFHS-4, reports that the prevalence of diarrhoea in rural India is 9.6 percent as against the prevalence of 8.2 percent in urban India. The prevalence of diarrhoea as reported by NFHS -4 in rural Udham Singh Nagar and urban Kolkata is 13.1 and 6.1 percent respectively.3 The prevalence of diarrhoea in urban Kolkata is not a true reflection of burden of disease in slums of Kolkata. We conducted our research under “Stop Diarrhoea Initiative” in rural block of Udham Singh Nagar and slums of Kolkata.
Challenges in diarrhoea control in rural areas and urban slums
Controlling childhood diarrhoea has always been a challenging task for public health practitioners. Health behavior and community practices are complex and vary from place to place. Human behavior is influenced by physical, social and biological factors around them. People behave differently based on their conscious and unconscious responses to these factors. A particular intervention that works in a particular set of conditions may work quite differently in another setting. Hence the outcomes of an intervention may also vary depending upon where it is implemented – in a rural area or in an urban slum.4 There are marked differences in the characteristics of urban slums and rural areas but despite this fact, the outcomes of intervention to control childhood diarrhoea may not necessarily be linked to these specific locations. There are certain other factors, such as mother’s education, quality of housing, sharing of water sources, sanitation facilities and use of surface water that may influence childhood diarrhoea outcomes.5 Adverse housing and environmental conditions are the two major factors that are strongly and persistently associated with risk of diarrhoea.6 Hence, it appears that analyzing diarrhoea and associated risk factors merely from the point of view of urban slum and rural locations would not be sufficient, particularly for policy makers and public health practitioners responsible for developing and implementing population wide health programmes.
Under “Stop Diarrhoea Initiative” of Save the Children, India a research study was conducted at two sites comprising rural Udham Singh Nagar district and urban slum of Kolkata to examine the effect of community based interventions on the incidence and longitudinal prevalence of diarrhoea and develop an understanding on how the same intervention works differently in urban slum and rural locations. The study also attempts to flash some light on whether diarrhoea control programmes should be seen from the lens of urban and rural locations or from the risk factors and health determinants lens for a desired level of change.
METHODS
Data collection on diarrhoea episodes
The study was conducted at 2 project sites in 2 states of India namely Uttarakhand and West Bengal. The study site in Uttarakhand state was a rural site in a district called Udham Singh Nagar and in West Bengal it was an urban site in the city of Kolkata. In Kolkata, 2 Municipal Wards namely ward number 58 and 65 were chosen. In district Udham Singh Nagar, a block called Sitranganj was chosen for the study. This block was the project implementation block under “Stop Diarrhoea Initiative (SDI)”. Within this block, 10 villages were chosen randomly where a cohort of 729 households was followed up for four weeks where under five children were found. In these households, we found 927 children below the age of 5 years. For the study, children below the age of 6 months were not included. These 927 children were followed up by community health volunteers (CHVs) for 4 weeks starting in the third week of February 2016. Out of these 927 children we found in 729 households, 484 children were followed up directly by CHVs and 245 children were followed up by mothers of these children. The follow up of these children was done to observe them for diarrhoeal episodes in the coming four weeks.
The CHVs were trained on diagnosis of diarrhoea based on the definition – “Passing of 3 or more loose or watery stool in 24 hours which contain more water than fecal content”.
The mothers were also trained by the community health workers under the supervision of block level training coordinator supported by SDI project. The data collection on the diarrhoeal episodes was done based on two different formats developed for CHVs and mothers. The data collection format was a simple format that required only putting a mark against the days when a diarrhoeal episode was observed. One such format was used for one week. So for all 4 weeks of data collection, 4 formats were used for each household. A regular follow up of the households was done for both the types of households – where data collection was done by CHVs and where the data collection was done by mothers directly (we called it self-reporting by mothers).
The diarrhoeal episode – in a period of four weeks when data was collected, if the same child had diarrhoea twice or thrice, they were treated as different cases for calculation of incidence and longitudinal prevalence.
The formats were developed in English and later on were translated in Hindi and Bangla. After the format development and translation, field testing of these formats was done at both the study sites comprising Sitarganj in Uttarakhand and Kolkata in West Bengal. Based on the experience of field testing, these formats were improved for ease of data collection and reporting.
In a similar fashion, data collection was done for 10 clusters spread over 2 wards of Kolkata city as mentioned earlier. The CHVs followed 353 children for a period of 4 weeks starting the third week of February 2016. Mothers in a similar way as in Sitarganj block, followed 192 children for the same period. This cohort of children followed by CHVs and mothers was spread over 10 clusters in both wards of Kolkata and households were selected randomly. The incidence and longitudinal prevalence calculated based on the data collected by community health volunteers are comparable to that of data reported by mothers. No statistical difference was found in incidence and longitudinal prevalence calculated using the two data sets.7 We collected data using these two methods (CHVs data sets and self-reporting of cases by mothers) and compared incidence and longitudinal prevalence to improve the validity of the results under the study.
After one year of implementation, in year 2017, the same data collection was done using the same formats by the CHVs and by the mothers. In this year also the mothers were trained on diagnosing the diarrhoea cases using the standard definition as mentioned earlier in the methodology section. In both the study sites comprising rural location in Sitarganj and urban location in Kolkata, in the third week of February 2017, data collection was done using the same format as used in the year 2016.
The households were again selected randomly at both the study sites. In Sitarganj block 899 children were followed up for 4 weeks and in both the wards of Kolkata, 545 children were followed up for 4 weeks.
The criteria for selecting the size of cohort was determined on the basis of the workload of CHVs. On the basis of workload analysis of the CHVs, it was determined that it is feasible for each CHV to collect data from 50 households and to support mothers in 25 households for self-reporting of diarrhoeal episodes. The SDI project supported 10 CHVs at each site in urban and rural areas and hence at each site a cohort of 500 households was directly followed by CHVs and 250 households were supported by these CHVs for self-reporting. In both the years, the cohorts which were followed for data collection (year 2016 and 2017), different number of children were found who were below 5 years of age and above the age of 6 months. All the available children based on this criterion were included in the study and followed up. This is the reason why we had different number of children reported in the study before and after the intervention.
Intervention
After the data was collected by mothers and CHVs, community level interventions were implemented in the entire block of Sitarganj and both the municipal wards of Kolkata. The interventions comprised enhancing the knowledge and skills of frontline health workers for diagnosis and treatment of diarrhoea, working with the community on Social and Behavior Change Communication (SBCC) by means of campaigns, interpersonal meetings with mothers and caregivers, group meetings and school sessions (Online Supplementary Document(Online Supplementary Document)). The SBCC mainly focused on positive behavior change on issues related to use of zinc and ORS (Oral Rehydration Salts), hand washing with soap, use of toilets, safe drinking water, immunization of children, early and exclusive breastfeeding, continued feeding during diarrhoea and vitamin A supplementation. In the intervention area, the community was also supported by building individual toilets, community toilet complexes, school sanitary blocks and repairing the water collection points. These works were only done for the purpose of demonstration.
Data collection on community behavior, practices and skills of service providers
The data collection on community behavior and practices related to diarrhoea prevention, control and treatment was done using a structured questionnaire. Simultaneously frontline workers were also interviewed using a structured questionnaire. This survey was conducted in February 2016, before the start of the intervention, and after 1 year in February 2017. The surveys were conducted at both the urban as well as rural sites. A sample size of 318 was calculated for Sitarganj block of Uttarakhand state and 135 households for urban wards number 58 and 65 for Kolkata city in the year 2016. For the year 2017, the sample size for Sitarganj was 330 households and 151 households for the wards number 58 and 65. The households were selected randomly where under-five children were found at the time of data collection. A listing of such households was done and then specified numbers of households were selected randomly. The frontline health workers in Sitarganj block and those in urban wards of Kolkata (No. 58 and 65) were contacted. In Sitarganj 30 frontline health workers were interviewed in February 2016 and 36 were interviewed in February 2017. In Kolkata their numbers were 12 and 9 for the respective years. For these surveys including community and frontline health workers for both the rounds in year 2016 and 2017, finite population sampling formula was used considering 5% margin of error.
Data analysis
The data analysis was done using an Excel spreadsheet and IBM SPSS Statistics (2015). The quantitative data which was collected using diarrhoeal episode recording formats by CHVs and by mothers for self-reporting was analyzed using excel sheet. For the 10 villages at rural locations and the 10 clusters at urban sites, longitudinal prevalence and incidence were calculated.
The longitudinal prevalence (LP) was calculated by using the below mentioned formula8:
LP = Number of days with diarrhoea/Number of days under observation
The incidence was calculated by using the below mentioned formula:
Incidence = Number of new events in a defined population over a defined period of time/Total person-time at risk during the defined period of time
Longitudinal Prevalence (LP) and incidence of disease were calculated using excel sheet and reported for block for rural sites and ward for urban sites. The LP and incidence of disease were compared for the study sites before and after the intervention.
The data from the surveys were analyzed for behavior and practice indicators and were reported at 95% confidence interval for the year 2016 and 2017. The comparison of these indicators was done for the year 2016 and 2017 to check the impact of the intervention on behavior and practices of the community and frontline health workers.
Limitations of the study
The biggest limitation of the study is the lack of control group in the study to be able to make attribution of the intervention on the outcome of interest. Another limitation of the study was that the sample size for the handwashing indicator was small hence the data of Sitarganj block was mixed with the data of another block to report it at 95% confidence interval. For the indicator on immunization, the data was collected by investigators by seeing the immunization card for the survey conducted in year 2016. For the same indicator for the year 2017, data was collected by seeing the immunization card as well as asking question on immunization based on recall. The hand washing data reported is based on self-reporting by mothers.
Ethical considerations
The permission for the study was taken internally from the Save the Children, India. The research study related documents were shared with the department of health. The ethical issues concerning the work were considered carefully. All the children who were below five years of age were part of the study at the sites which were selected for data collection. The participants were informed about the purpose of data collection and their consent for participation was taken. During the course of investigation, the children who were found to be having diarrhoea, were given ORS and zinc and their mothers were counselled on the home based management of the cases.
RESULTS
Change in health behavior and practices at the community level
Table 1 shows that the intervention in the rural area of the project has resulted in a marked improvement in the health related behavior and practices in the community pertaining to childhood diarrhoea. The highest improvement is recorded in the treatment of children with zinc in terms of percentage; however the actual proportion of the children treated with zinc still remains low at around 11% and 25% in rural and urban areas respectively. Exclusive breastfeeding for first 6 months of life was higher initially in rural areas and intervention may have helped it to improve further but it remained low in comparison to urban area. Similarly early breastfeeding within 1 hour of birth increased in rural area but decreased in the urban area after the intervention. Another impression that table 1 gives is that the knowledge about the disease, treatment of the disease and vaccination have shown more improvement in urban areas in comparison to rural areas post intervention. The early initiation of breastfeeding in urban areas shows a decline after the intervention but exclusive breastfeeding for first 6 months of life has shown a marked improvement after the intervention.
Table 2 shows that after the intervention (figures are given in parenthesis), hand washing behavior at critical stages has improved in both rural and urban areas. The proportion of women washing their hands after defecation, after cleaning the feces of the child and before feeding the child has improved more in urban areas compared to rural areas after the intervention. However, after the intervention, in rural areas, higher proportion of women wash their hands before cooking and before eating compared to that in urban area. So we observed a differential change in hand washing behavior in urban and rural areas after the intervention.
Table 3 delineates that training of frontline health workers on managing childhood diarrhoea cases at the community level has shown marginal improvement in skills of the workers both in rural as well as urban areas.
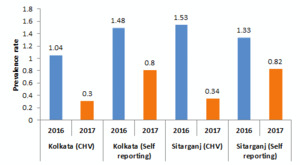
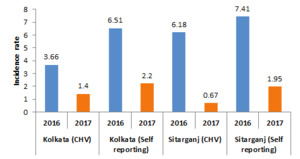
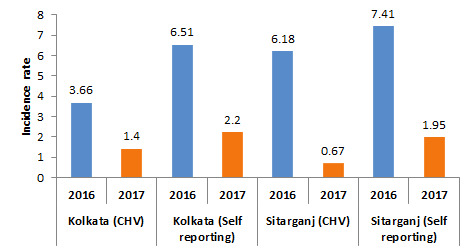
Both the data sets (Community Health Volunteer and self-reporting by mothers) in Figure 1 and Figure 2 shows that intervention in rural and urban areas has resulted in reduction in the longitudinal prevalence and incidence of childhood diarrhoea. The reduction in incidence in rural areas (for CHV reported data set) is more striking, where it decreased from 6.18 cases per 1000 population to 0.67 cases per 1000 population compared to urban areas where the incidence has come down from 3.66 cases per 1000 population to 1.4 cases per 1000 population. The trend from data set of self-reporting by mothers also looks similar where it has come down from 6.51 to 2.2 for urban areas and from a level of 7.41 to 1.95 in rural areas. Both the data sets suggest that reduction in diarrhoea incidence is sharper in rural areas as compared to urban areas of the project.
Figure 1 also shows that longitudinal prevalence has come down post intervention in both – the urban and rural locations but there is no striking difference in rural and urban locations as observed in the case of incidence of diarrhoea (Figure 2). The CHV data set and data set of self-reporting by mothers – both shows similar trend of reduction in longitudinal prevalence of diarrhoea after the intervention.
Figure 2 shows that incidence of diarrhoea is recorded higher in rural as well as in urban areas from the data sets which were based on self-reporting by mothers of children who suffered diarrhoea during the course of investigation.
The longitudinal prevalence shows a sharp decline for rural areas (from 1.53 to 0.34) compared to urban areas (1.04 to 0.3), (Figure 1) if we look at the data reported by CHVs however, for self-reporting data sets for the urban and rural areas, such sharp decline in longitudinal prevalence of diarrhoea is not observed after the intervention. But longitudinal prevalence has come down after the intervention in both the areas (rural and urban) and both the data sets confirm this observation.
Overall Figure 2 shows that the incidence of diarrhoea in rural areas has come down to a lower level (from 6.18 to 0.67 for CHV data set and from 7.41 to 1.95 for self-reporting) when compared to that of urban areas where reduction is less (from 3.66 to 1.4 for CHV data set and from 6.51 to 2.2). The data suggest that urban area looks more challenging from the point of view of reducing incidence. But if longitudinal prevalence is seen at the end of intervention in the year 2017, it is observed that reduction in longitudinal prevalence is more in urban areas (Urban area LP reduced to 0.3 from 1.04 for CHV data and from 1.48 to 0.8 for self-reporting data set) compared to rural areas (LP reduced to 0.34 from 1.53 for CHV data set and 0.82 from 1.33 for self-reporting) and both the data sets show a similar trend.
DISCUSSION
Our findings indicate that both in the rural areas as well as in the urban slums, community based interventions with mothers, caregivers and frontline health workers; related to health education, hygiene, community based treatment of childhood diarrhoea cases using ORS and Zinc have helped in improving the health behavior and practices at the family level. Results indicate that hand washing has improved in both the urban slums and rural areas of the project. This may have contributed to reduced diarrhoeal incidence at the study sites. Other research studies have also confirmed similar findings.
In a study conducted in Burundi, the authors concluded that in rural areas, hygiene education at household and community levels pertaining to hand washing with soap has helped in reducing the burden of diarrhoea among under five children.9 The Cochrane review also suggests that promotion of hand washing with soap in lower and middle income country settings reduces diarrhoeal episodes by around 30%.10 Nevertheless, this review also highlighted the fact that maintaining the hand washing behavior in the community for long is less understood10 hence in our settings the improvement in hand washing behavior and reduction in diarrhoeal incidence and also the longitudinal prevalence might be an immediate effect of the SDI intervention.
Similar to our study, a study was conducted in Lusaka, Zambia where a package of prevention and treatment interventions was introduced and post and pretest surveys were conducted. This study revealed that the diarrhoeal episodes, 2 weeks preceding the survey in the intervention area declined from 15.8% to 12.7%.11 The findings from all these studies support that reduction in incidence and longitudinal prevalence in our study may be attributed to the community based interventions that we had with mothers, caregivers, community people in villages and urban slums and frontline health workers at the project sites. Our interventions have improved early and exclusive breastfeeding, immunization, hand washing with soap at critical times such as after defecation and after cleaning the child feces. The intervention has also improved diagnosis and treatment of children with ORS and Zinc at the community level. These factors would have contributed to the reduction in the incidence of diarrhoea and longitudinal prevalence at our research sites.
There are several other studies that indicate that modification in risk factors contribute to lower mortality and morbidity caused by diarrhoea. In a study conducted in the urban slums of Bankura, West Bengal, the authors found that poor feeding practices, low immunization rates and poor nutrition statuses increase the risk of diarrhoea among the under five children and health education helped in tackling these risk factors.12 In a systematic review, Das et al also found that community based interventions on health education and treatment have reduced diarrhoea related morbidity and mortality and have potential for scale-up.13 Based on our findings and supportive evidence from different parts of the world, we conclude that our community based interventions in urban and rural settings have contributed to the reduction in diarrhoea incidence and longitudinal prevalence primarily by modifying the risk factors.
Post intervention, results indicate that in rural area less number of children are being affected by diarrhoea compared to urban area as reduction in diarrhoea incidence is more in rural areas compared to that of urban areas; and both the data sets support this finding. Urban slums are characterized by poor sanitation conditions and overcrowding compared to rural areas. Rural areas on the other hand are characterized by more open spaces and comparatively better sanitation. These observations are in line with a study conducted in urban slums in India that reveals that environmental characteristics in urban areas significantly increase the risk of children being affected by diarrhoea.5 Consequently, children living in rural areas have advantage over children living in the urban areas, as they have less risk of getting diarrhoea.
This observation is in conformity with a recent study conducted by Kawakatsu et al. in Kenya. They reported that children living in rural areas were significantly less likely to experience diarrhoeal symptoms than those living in urban areas.14 A study conducted in Bangladesh also confirms this finding.6 Hence diarrhoea control in urban slums is apparently seems more complicated than diarrhoea control in rural areas. Therefore, a different strategy may be required to have the same degree of effect over diarrhoea incidence. This is primarily because of differences in the risk factors prevailing in urban slums and rural areas than merely because of the location itself.
We found that there are some studies conducted in some other parts of the world which concluded that human behavior is complex and depends upon human responses – conscious or unconscious, to prevailing set of factors in an area. The health determinants such as access to housing, water sources, livelihood, education, availability of health services determine the behavior of the people and thereby health outcomes. Hence linking health outcomes simply to location might not be correct because within a location, a set of factors may lead to different health outcomes.4,6
Those children who developed diarrhoea in urban slums, took less time to recover compared to children who developed diarrhoea in rural area as the results indicate that after the intervention, longitudinal prevalence in urban slums has come down to a lower level compared that of rural area. Both the data sets confirmed this observation. After the intervention, in urban slums the treatment of childhood diarrhoea cases with ORS and Zinc increased to more than two fold compared to that of rural area. This proportionate increase in treatment of the cases in urban slums over rural area might have reduced the longitudinal prevalence in urban area more than in rural area.
In many other studies zinc treatment has shown to reduce the duration and severity of diarrhoea. Walker and coworker in their study have concluded that zinc supplementation has reduced duration of diarrhoea.15 In an another randomized control trail, Bhatnagar and coworkers found that oral rehydration therapy along with zinc treatment have reduced the duration of diarrhoea and stool output in children suffering from diarrhoea.16 Another possible reason of comparatively higher reduction in longitudinal prevalence in urban slums than that of rural area may be due to better access to health facility or a health care provider in and around the urban slums. This finding in our research is in line with the Wardlaw and coworkers’ research who studied the burden and distribution of childhood diarrhoea and found that children living in urban areas (42%) are more likely to receive the recommended treatment for diarrhoea than those children who are living in rural areas (38%).2 One more probable reason of reduced longitudinal prevalence in urban areas in our study might be due to higher awareness of symptoms of diarrhoea among the mothers which might have prompted early treatment seeking behavior. There are some evidences available which suggest improved community awareness along with treatment availability reduce burden of diarrhoea.17 In another research conducted in Brazil, authors concluded that increased education about diarrhoea directly reduces prevalence of the disease in the community.18
In our study, there are some other findings as well which need further investigation to develop better understanding. We found that early initiation of breast feeding and exclusive breast feeding for first six months of life of children improved more in rural areas compared to that of urban areas after the intervention. We also found a drastic increase in immunization in urban areas than that in rural areas after the intervention. The results also indicated a marked change in handwashing practice after defecating and after cleaning the child feces but only a marginal improvement seen in hand washing practice before cooking and eating in both rural and urban areas. The explanations for these findings specific to the sites of research study need to be found and further research would be helpful to understand these phenomena.
CONCLUSIONS
Our community based intervention with mothers, caregivers and frontline workers on childhood diarrhoea prevention, control and treatment has helped in reducing diarrhoea incidence and longitudinal prevalence in both rural and urban areas. The reduction in diarrhoea incidence was recorded more in rural area compared to that in urban area, however reduction in longitudinal prevalence was recorded more in urban area compared to that in rural area. Reducing diarrhoea incidence in urban area seems more challenging, however treatment of diarrhoea in rural area is apparently more challenging than reducing its incidence.
Finally, we conclude that for a comprehensive diarrhoea control and treatment in rural areas and urban slums, differential approaches may be more useful which are based on community behavior, risk factors and access to child care services to have a similar degree of impact on diarrhoea burden in urban slums and rural areas, than merely based on the perceptions of urban slums and rural areas.
Data availability
The data formats in hard forms are available at the project sites.
Funding
Generous financial support from Reckitt and Benckiser to conduct the study is duly acknowledged.
Conflict of Interest
The authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no competing interests.
Correspondence to:
Farhad Ali
Health Advisor
Save the Children
National Support Office
Plot no 91, Sector 44, Gurgaon – 122003
Haryana, India
[email protected]